In late July 2020, 28-year-old Sumit Verma (name changed) was wheeled into a private healthcare facility in Gurgaon. He had slipped into a coma after experiencing severe convulsions.
“We put him on a ventilator. He was in a deep comatose state,” says Praveen Gupta, Director of Neurology at the Fortis Memorial Research Institute (FMRI). Gupta speculated that this was an unusual manifestation of COVID-19.
Verma went on to develop typical COVID-19 symptoms – respiratory distress, fever, cough and cold. Occasionally, there was blood in his sputum. In the days that followed, he tested positive for COVID-19 twice before finally getting a negative test result in 17 days of being treated with hydrochloroquine along with antibiotics and anti-seizure medication.
Within a month, five more COVID-19 cases were admitted to FMRI, all with neurological symptoms followed by other flu-like symptoms, Gupta says.
Researchers across the world are gathering more evidence around the neurological manifestations of COVID-19. Epileptic seizures, haemorrhage and acute stroke-like conditions are being added to the repertoire of COVID-19 symptoms. In a recent study in China, five per cent of COVID-19 patients were found to develop blood clots impeding the flow of oxygen to the brain that caused such cerebrovascular incidences1.
Invading the brain
The blood-brain barrier – the fence between the brain and the rest of the body – protects the brain against viral invasions.
However, a COVID-19 triggered cytokine storm – an exaggerated immune reaction set by SARS-CoV-2 – can breach that barrier.
Reviewing the neuropathological assaults of SARS-CoV-2, researchers at the National Brain Research Centre (NBRC) in Manesar near Delhi reassessed its role as more than just a respiratory virus2 . The team had earlier reported that the Zika virus, which crosses the blood-brain barrier to infect human foetuses, is capable of altering the properties of human neural stem cells.
“The MERS and SARS virus have earlier been reported to invade the brain’s nervous tissue through the blood-brain barrier. A similar invasion route is possible for SARS-CoV-2,” says Pankaj Seth, who leads the NBRC group.
Autopsy studies3 of COVID19 mortalities have revealed SARS-CoV-2 viral load in neurons as also in other non-neural tissues. The loss of taste and smell senses, headache, nausea, dizziness and incoherence in COVID-19 patients can be strongly correlated to the brain function, Seth says. Since SARS-CoV-2 perturbs the gut lining as well, the gut-brain axis may aid in transfer of the virus to brain tissue.
In a three month follow-up4 of 60 patients who had recovered from COVID-19 in China, researchers corroborate this neuro-invasive potential of SARS-CoV-2. Studying the micro-structural changes in their brains through MRI scans, they found that during the SARS-CoV-2 infection, 41 of these patients displayed neurological symptoms such as loss of a sense of taste or smell, numbness in the limbs and memory deficits. Three months after the infection, their MRI scans revealed enlarged volumes of the olfactory cortex, hippocampus, insula and the cingulate cortex. Together, these areas of the brain regulate the sense of smell, memory formation and emotional processing.
The researchers also traced the possible route of the SARS-CoV-2 invasion into the brain. The brain’s seat of the sense of smell, the olfactory cortex, increased in volume in COVID-19 patients indicating that the brain was trying to compensate for an impaired sense of smell.
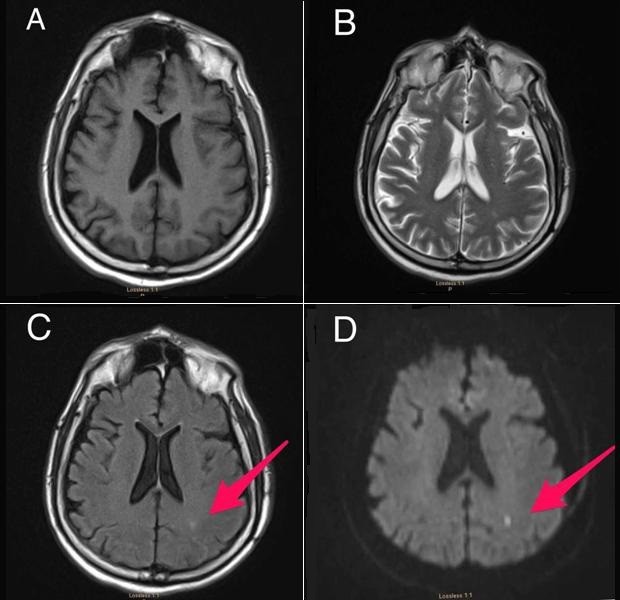
MRI brain scan of a COVID-19 patient shows an infarct spot, a cerebrovascular occurrence due to restricted blood flow in acute stroke, marked by red arrow in C and D. Standard scans of the same patient show brain tissue in A and B. © Espinosa, P. S. et al. Cureus. doi: 10.7759/cureus.7930
The sensory cells of the nasal cavity which project directly to the olfactory bulb in the brain, robustly express ACE 2 – the cellular receptors that SARS-CoV-2 binds to for its survival and replication5.
This makes it a strong possibility that the respiratory coronavirus inhaled through droplets or aerosols may be using the olfactory route of infection as an entry point to the brain.
Past parallels
Earlier pandemics such as the Spanish Flu of 1918 provide possible historical parallels to the neuropathological indications of SARS-CoV-2.
In 1918, the ability to study the varied neurological and neuropsychiatric associations in the Spanish flu was limited, says Tom Solomon, Director of the National Institute for Health Research (NIHR) at the University of Liverpool in the UK. “Although SARS-CoV-2 is a completely different virus, we are much better placed (in 2020) with new technologies to understand exactly how such respiratory viruses lead to neurological disease,” Solomon, who is at the institute’s Health Protection Research Unit in Emerging and Zoonotic Infections, says.
A wave of neurological pandemic coincided with the Spanish Flu and lasted for another decade. It presented as an extreme form of exhaustion – called encephalitis lethargica – causing a profound and irreversible damage to the central nervous system.
There is an ongoing debate about the relationship between encephalitis lethargica and neuropsychiatric manifestations in COVID-19 as well. James J. Sejvar , a neurovirologist and epidemiologist at the US Centers for Disease Contol and Prevention (CDC), says conditions such as difficulty in memory and cognition and Parkinsonism earlier described in Spanish flu-triggered encephalitis lethargica are similar to those being observed as neuropsychiatric manifestations in SARS-CoV-2 infection. “In terms of symptomatology, I think there are lines that can be drawn between the two, but we need to be careful in drawing this comparison,” he says.
The lasting neurological effects of COVID-19 on the brain must be mitigated by closely monitoring COVID-19 patients beyond the duration of their infection. Collaborations such as the COVID-19 Neuro Network, a global effort led by the Liverpool Brain Infections Group, are facilitating such monitoring. The network is pooling patient data from across the globe with an aim to characterise neurological associations of COVID-19 and determine risk factors for development of neurological disease in COVID-19.
The repository aims to provide a framework for clinical decision making in the long haul, as medical practitioners and researchers strive to define what a textbook case of COVID-19’s effect on the brain may look like.
(*Vanshika Singh is a Senior Research Fellow at the National Brain Research Centre, Manesar, Haryana, India.)
Nature India's latest coverage on the novel coronavirus and COVID-19 pandemic here . More updates on the global crisis here .
References
1. Belany, P. et al. COVID-19 is an independent risk factor for acute ischemic stroke. Am. J. Neuroradiol. (2020) doi: 10.3174/ajnr.A6650
2. Singal, C. M. s. et al. SARS-CoV-2 more than a respiratory virus: Its potential role in neuropathogenesis. ACS Chem. Neurosci. (2020) doi:10.1021/acschemneuro.0c00251
3. Bulfamante, G. et al. First ultrastructural autoptic findings of SARS-CoV-2 in olfactory pathways and brainstem. Minerva Anestesiol. (2020) doi: 10.23736/S0375-9393.20.14772-24
. Lu, Y. et al. Cerebral micro-structural changes in COVID-19 patients – An MRI-based 3-month follow-up study. E Clinic. Med. (2020) doi: 10.1016/j.eclinm.2020.100484
5. Chen, M. et al. Elevated ACE2 expression in the olfactory neuroepithelium: Implications for anosmia and upper respiratory SARS-CoV-2 entry and replication. bioRxiv (2020) doi: 10.1101/2020.05.08.084996
