Abstract
Clostridium difficile is the leading cause of nosocomial infections in the United States. Clinical disease outcomes after C. difficile infection (CDI) are dependent on intensity of host inflammatory responses. Specifically, peak peripheral white blood cell (WBC) count >20 × 109 l−1 is an indicator of adverse outcomes in CDI patients, and is associated with higher 30-day mortality. We show that homozygosity for a common single nucleotide polymorphism (Q to R mutation in leptin receptor that is present in up to 50% of people), significantly increases the risk of having peak peripheral WBC count >20 × 109 l−1 (odds ratio=5.41; P=0.0023) in CDI patients. In a murine model of CDI, we demonstrate that mice homozygous for the same single nucleotide polymorphism (RR mice) have more blood and tissue leukocytes (specifically neutrophils), exaggerated tissue inflammation, and higher mortality as compared with control mice, despite similar pathogen burden. Further, we show that neutrophilia in RR mice is mediated by gut microbiota-directed expression of CXC chemokine receptor 2 (CXCR2), which promotes the release of neutrophils from bone marrow reservoir. Overall these studies provide novel mechanistic insights into the role of human genetic polymorphisms and gut microbiota in regulating the fundamental biological process of CDI-induced neutrophilia.
Similar content being viewed by others
Introduction
Clostridium difficile is the most common cause of hospital-acquired infections in the United States1 and is ranked in the top three urgent public health threats by the CDC (www.cdc.gov).2 Host genetic factors can alter the risk of acquiring C. difficile: a common single nucleotide polymorphism (SNP) in the interleukin-8 gene increases susceptibility to C. difficile colitis,3 and we have previously shown that a non-synonymous SNP, rs1137101, on the extra cellular domain of leptin receptor (LEPR) increases the risk of C. difficile diagnosis.4 We found that individuals homozygous for the derived allele G, which encodes for Arginine (R) at position 223 (RR genotype) were at a higher risk of being diagnosed with C. difficile infection (CDI) (odds ratio 3.03), as compared with individuals either homozygous or heterozygous for the ancestral allele A, which encodes for Glutamine (Q, QQ, or QR genotype) at the same position.4 Q223R is a common SNP in humans with a mean allelic frequency of ∼50% in European-Americans and 40–60% in African-Americans (http://hgdp.uchicago.edu). Notably, RR genotype has been associated with more severe disease and worse outcomes after intra-abdominal infections: increased risk of amebic colitis in children,5 increased incidence of amobic liver abscess5 and higher mortality after secondary bacterial peritonitis in adults.6 But the influence of LEPR SNP on CDI clinical disease severity and the mechanisms that could alter infectious disease outcomes in individuals with RR genotype remain unknown.
Indigenous gut microbial flora and host inflammatory responses are key determinants of clinical disease outcomes after CDI.7, 8, 9 Alterations in gut microbial communities (dysbiosis), typically caused by antibiotic exposure, create an ideal niche for initial C. difficile spore colonization and germination.10 After spore germination, the vegetative C. difficile bacteria produce an enterotoxin and a cytotoxin (toxins A and B), which are the major C. difficile virulence determinants that cause colonic tissue damage. The inflammatory response elicited by C. difficile and its toxins is predominated by neutrophils and is characterized by peripheral blood leukocytosis, immune cell infiltration into colonic tissue, and production of many pro-inflammatory mediators.11 Neutrophils are the primary innate effector cells in the host response to C. difficile but neutrophil responses in CDI need to be tightly regulated as both an over-exuberant neutrophil response after infection or neutropenia can be deleterious to the host. For example, peripheral white blood cell (WBC) count >20 × 109 l−1 (mainly comprised on blood neutrophils) is an independent risk factor for increased 30-day mortality,9 and patients with severe CDI develop pseudomembranous colitis, which is characterized by excessive colonic neutrophil infiltration and tissue damage.12 The importance of neutrophils in CDI pathogenesis is further highlighted by studies in animal models where depletion of neutrophils protects colonic tissue from injury after C. difficile toxin challenge.13, 14 However, complete lack of neutrophils is also not favorable to the host: neutropenic patients have higher incidence of CDI (both initial and recurrent),15, 16 and in murine models, antibody-mediated neutrophil depletion prior to infection with C. difficile (instead of intoxication) results in higher mortality owing to increased translocation of gut bacterial pathobionts from colonic lumen to intra-abdominal organs.17 Taken together, these studies highlight the importance of indigenous gut microbial flora and the dichotomous nature of host neutrophil response in CDI pathogenesis that can affect clinical disease outcomes.
In this study, we investigated the innate immune responses to C. difficile in the context of LEPR Q to R mutation in humans and mice. We show that CDI patients homozygous for the derived LEPR allele (RR genotype) had higher peripheral blood leukocytosis, compared with patients homozygous or heterozygous for the ancestral allele (QQ/QR genotype). We modeled human CDI in mice with the same SNP and show that similar to patients, mice homozygous for the derived LEPR allele (RR mice) had exaggerated systemic leukocytosis and neutrophilia. In addition, RR mice had higher tissue neutrophils and inflammatory cytokine expression, increased colonic tissue damage and higher mortality, as compared with control QQ mice, despite equivalent C. difficile burden. Our studies elucidate the complex interplay between host genetics, immunity, and gut microbiome, and show that the enhanced neutrophilia in RR mice is mediated by gut microbiota-directed increase in cell surface expression of neutrophil-recruiting CXC chemokine receptor 2 (CXCR2) that promotes the release of bone marrow neutrophils in response to C. difficile.
Results
Individuals with RR genotype have higher peak peripheral blood leukocytosis after CDI
We have previously reported that individuals with RR genotype had higher risk of CDI diagnosis.4 Here, we investigated the host response to C. difficile in a cohort of CDI patients, and studied the association between LEPR Q223R polymorphism and peak peripheral WBC count (highest WBC value between 3 days before and 3 days after C. difficile diagnosis). Patients with RR genotype were more likely to have a peak WBC count of >20 × 109 l−1 in the peri-diagnosis time frame (odds ratio=5.41; P=0.0023; multivariate logistic regression analysis with adjustment for age, race and gender), compared to patients with QQ/QR genotype (Table 1 and Supplementary Table 1 online). Peripheral blood leukocytosis (predominated by neutrophils) is commonly seen in CDI, and magnitude of leukocytosis predicts clinical disease outcomes.9 The peak peripheral WBC count cut-off value and peri-diagnosis reference time frame used in our analysis was based on previous studies, which show that WBC count of >20 × 109 l−1 between 5 days before and 3 days after C. difficile diagnosis is an independent predictor of increased 30-day mortality.9, 18 Our data thus indicate that individuals with RR genotype are at an increased risk of having worse outcomes after CDI.
Mice with RR genotype have higher blood and tissue neutrophilia after CDI
To investigate how LEPR Q223R SNP influences host WBC response to C. difficile, we used a murine model of CDI. Age- and gender-matched QQ and RR mice were pre-treated with cefoperazone for 9 days in drinking water, followed by regular water without antibiotics for 2 days as previously described,19 and then challenged with purified C. difficile spores by oro-gastric gavage (Figure 1a). Mice were killed at day 1 and day 3 after infection to analyze peripheral blood and tissue immune responses. C. difficile challenge increased total WBC and neutrophil counts in both QQ and RR mice compared with their respective sham-challenged controls, but the cell numbers were significantly higher in RR mice (P<0.05; Figure 1b). Differential blood count revealed that the surge in WBCs in RR mice was owing to increased neutrophils (Figure 1c), and circulating monocytes and eosinophils were similar in both groups (Figures 1d and e). By day 3 after infection, QQ and RR mice had comparable total (and differential) WBC counts (Figures 1b and e). Antibiotic pre-treated QQ and RR mice had similar number of circulating total and differential WBCs (Figures 1b and e).
RR mice have higher blood leukocytosis and neutrophilia after CDI. (a) Schematic representation of experimental design of C. difficile infection in mice. Age- and gender-matched QQ and RR mice were pre-treated with antibiotics for 9 days in drinking water and challenged with 1 × 106 C. difficile (VPI 10463) spores by oro-gastric gavage 2 days after cessation of antibiotics. Animals are killed at time points indicated to evaluate the peripheral and tissue cellular response dynamics using Hemavet and fluorescent activated cell sorting (FACS) analysis, respectively. Plots show number of (b) total WBC (dotted line indicates the maximum of normal range in mice), (c) neutrophils (d) monocytes and (e) eosinophils per ml of blood. Data shown as mean±s.e.m. from 6 to 9 mice per group. (*P<0.05, **P<0.01, ***P<0.001; Students’ t-test).
We next examined the immune cell infiltrate in cecum and colon of QQ and RR mice by flow cytometry of lamina propria cells. Prior to infection, both QQ and RR mice had very few immune cells in the lamina propria (Figure 2a). By day 1 of C. difficile challenge, a large number of immune cells were recruited to the colon in both groups of mice, but similar to peripheral blood, RR mice had significantly higher number of total immune cells (CD45.2+) and neutrophils (CD45.2+CD11b+Ly6G+) per gram of cecal tissue (P=0.017; Figures 2a and b). As seen in peripheral blood, the number of monocytes (CD45.2+CD11b+Ly6G−Ly6C+) and eosinophils (CD45.2+CD11b+Ly6ClowSiglecF+) in tissue was comparable between QQ and RR mice (Figures 2c and d). By day 3 after infection, and concurrent with improvement in clinical disease, the total number of immune cells, neutrophils and monocytes in cecal lamina propria of RR mice decreased significantly but the number of tissue neutrophils and monocytes in QQ mice was similar to day 1 levels.
RR mice have higher tissue leukocytosis and neutrophilia after CDI. (a) CD45+ cells (b) neutrophils (c) monocytes, and (d) eosinophils per gram of cecal tissue. Data shown as mean±s.e.m. from 6 to 9 mice per group. (*P<0.05, **P<0.01, ***P<0.001; Students’ t-test).
RR mice have higher tissue inflammation and decreased survival after CDI
Within 1 day after C. difficile challenge, RR mice had higher expression of pro-inflammatory cytokines: interferon-gamma, macrophage migration inhibitory factor, tumor necrosis factor alpha, and interleukin-6 in cecum (*P<0.05; Figure 3a) and significantly more colonic tissue damage (*P<0.05; Figures 3b and c), as compared with control QQ mice. Specifically, RR mice had more inflammatory cells and submucosal edema (Figures 3d and f and Supplementary Figure S1). This enhanced inflammation was not owing to higher pathogen burden, as the number of C. difficile colony forming units per gram of cecal content and levels of C. difficile toxins were comparable in QQ and RR mice at all time points after infection (Figures 4a and b). Notably, we saw mortality only in RR mice (across six different experiments) and mice died between 36 and 60 h after CDI (Figure 4c and Supplementary Figure S2a). By day 3 after infection, all QQ mice and the surviving RR mice had improved histology scores (Figures 3c–f) and better clinical disease (improved weight and reduced diarrhea; Figure 4d and Supplementary Figure S2b). Overall, our data from patients with CDI and from the mouse model reveal that host genetics has a role in regulating the systemic and tissue immune response, and clearly show that RR genotype is associated with an exaggerated immune response and tissue damage to the same number of C. difficile bacteria.
RR mice have higher inflammation after CDI. (a) mRNA expression in cecal tissue represented as fold change vs uninfected controls. Data shown as mean±SEM from six mice per group. (b) Representative histology of hematoxylin and eosin–stained colon sections at day 1 (D1) and day 3 (D3) of C. difficile infection. Scale bar=1 mm. (c) Total histology score for (d) submucosal edema, (e) inflammatory cell infiltration, and (f) epithelial damage in cecal tissue sections. Data shown as mean±s.e.m. from 10 to 13 mice per group. (*P<0.05, ###P<0.001; Students’ t-test).
RR mice have decreased survival irrespective of similar C.difficile burden. C. difficile (a) bacterial colony forming unit (CFU) and (b) toxin A/B per gram of cecal content of C. difficile-challenged mice. Data shown as mean±s.e.m from 6–9 mice per group (c) Percent mortality and (d) percent weight change of C. difficile-challenged mice. Data shown as mean±s.e.m. from six different experiments with a total n=42–44 mice per group. (*P<0.05; Students’ t-test or ANOVA).
Q223R polymorphism does not alter leptin levels or neutrophil functional capacity
Leptin is known to affect immune cell functions such as generation of reactive oxygen species, inflammatory cytokines/chemokines production, and phagocytic capacity of neutrophils, monocytes, and macrophages,20 thus we measured leptin levels and neutrophil functions in QQ and RR mice. Total leptin in plasma and tissue was similar between the two groups of mice (plasma; Figure 5a, tissue; Supplementary Figure S3a). But the amount of bioavailable leptin is regulated by soluble LEPR, which binds to free leptin21 and decreases overall leptin signaling, thus we measured soluble LEPR in plasma of QQ and RR mice. We saw no difference in soluble LEPR concentration in uninfected or C. difficile-infected QQ and RR mice (uninfected; Supplementary Figure S3b, Infected; Figure 5b); suggesting that Q223R polymorphism does not impact leptin signaling upstream of LEPR. In vitro transfection studies have shown that signaling from LEPR mutant allele (RR) leads to diminished signal transducer and activator of transcription 3 (STAT3) signaling,22 and a lack of leptin-STAT3 signaling reduces phagocytic ability of alveolar macrophages,23 but the impact of Q223R polymorphism on neutrophil functions is not known.
Q223R polymorphism does not alter leptin levels or neutrophil functional capacity. (a) Leptin and (b) soluble leptin receptor concentration in plasma on day 1 of CDI. Flow cytometric analysis of (c) phagocytosis (E. coli AF-488) and (d) oxidative burst; DHR-123 in cecal tissue neutrophils after ex vivo fMLP stimulation. Myeloperoxidase (MPO) activity in tissue homogenates of C. difficile-infected QQ and RR mice on day 1 of infection (e) normalized to tissue weight and (f) number of tissue neutrophils. Data shown as mean±s.e.m. from 4 to 5 mice per group, representative of at least two independent experiments. (*P<0.05; Students’ t-test).
Thus, we tested the functional status of sorted QQ and RR neutrophils. Magnetic bead sorted colonic neutrophils from C. difficile-infected QQ and RR mice phagocytosed similar proportions of Escherichia coli bioparticles and generated comparable levels of reactive oxygen species in response to ex vivo N-Formyl methionyl-leucyl-phenylalanine stimulation (Figures 5c and d). Arguably, tissue neutrophils from C. difficile-infected mice are already exposed to an inflammatory environment and may have impaired ability to respond to a second ex-vivo stimulus, thus we examined phagocytosis and generation of reactive oxygen species in purified bone marrow neutrophils from naive QQ and RR mice. Similar to ex vivo isolated neutrophils, the functional capacity of bone marrow neutrophils from QQ and RR mice was not different after in vitro challenge with N-Formyl methionyl-leucyl-phenylalanine (Supplementary Figure S3c–d). Myeloperoxidase (MPO) is a component of neutrophil azurophilic granules, which is secreted upon neutrophil activation. While extracellular MPO activity causes tissue damage, intracellular MPO activity represents the number of neutrophils in tissue.24 At day 1 of infection, colonic tissue lysates (includes both intracellular and extracellular MPO activity) from RR mice had significantly high MPO activity (Figure 5e) compared with QQ tissue. However, difference in MPO activity was lost when normalized against total neutrophil numbers, indicating that there is no difference in MPO activity on a per cell basis between QQ and RR neutrophils (Figure 5f). Taken together, these experiments showed that LEPR Q to R SNP does not alter the functional capacity of neutrophils.
RR mice have increased expression of CXCR2 on bone marrow and blood neutrophils
Infectious challenge induces a rapid release of neutrophils from bone marrow reservoir and migration to peripheral blood and inflamed tissue.25 In the tissues, neutrophils control pathogen and regulate inflammation, but a large number of cells also die in the process.26 Therefore, higher neutrophil numbers observed in RR mice could be due to decreased cell death in tissues or increased cellular release from bone marrow. We found that there was no difference in cell death between QQ and RR neutrophils without infection and after CDI (Figure 6a). However, 1 day after C. difficile challenge, and concurrent to increased neutrophils in blood and tissue, we found a significant reduction in number of neutrophils in the bone marrow of RR mice (P=0.03; Figure 6b) indicating enhanced neutrophil release from bone marrow after CDI. Thus, we examined the factors involved in neutrophil mobilization from bone marrow. Neutrophil release from bone marrow is directed by binding of chemokines to chemokine receptors. CXC chemokines (CXCL1 and CXCL2) bind to their cognate receptor CXCR2 and induce neutrophil mobilization from bone marrow to peripheral blood and to colonic tissue.27, 28 CDI increased CXCL1 and CXCL2 expression (day 1 after infection) in both QQ and RR mice, as compared with sham-infected controls, but the levels of these chemokines were similar in QQ and RR mice both in plasma and in cecal tissue (plasma; Figure 6c, tissue; Supplementary Figure S3e). Levels of other neutrophil recruiting cytokines, GM-CSF and G-CSF, were also comparable in the two groups of mice (Figure 6c and Supplementary Figure S3e).
RR mice have increased expression of CXC chemokine receptor 2 (CXCR2) on neutrophils. QQ and RR mice were challenged with C. difficile spores. (a) Annexin V+ 7AAD+ (apoptotic) neutrophils in cecal tissue as measured by flow cytometry. (b) Number of neutrophils in bone marrow (c) concentration of neutrophil chemokines in plasma, and (d) mean fluorescence intensity (MFI) of CXCR4 on mouse bone marrow neutrophils at day 1 of C. difficile infection. MFI of CXCR2 on (e) bone marrow neutrophils (f) blood neutrophils and (g) bone marrow monocytes after cefoperazone treatment (Abx) and at day 1 of CDI (inf_D1). CXCR2 inhibitor (SB225002) was injected intraperitoneally (1 mg kg−1 per day) for 2 days prior to C. difficile challenge and (h) MPO activity was assessed in cecal tissue homogenates on day 1 of infection. Data shown as mean±s.e.m. from 3 to 9 mice per group (*P<0.05, **P<0.01, ***P<0.001; Students’ t-test).
We thus postulated that expression of chemokine receptors on the cell surface could influence egress of neutrophils from bone marrow. Although binding of CXCL1 and CXCL2 to CXCR2 augments cellular release from bone marrow, CXC chemokine receptor 4 (CXCR4) interaction to its ligands promotes cellular retention in bone marrow.28 Expression of CXCR4 on bone marrow neutrophils was similar between QQ and RR mice (Figure 6d). However, compared with QQ mice, CXCR2 expression was higher on bone marrow and blood neutrophils of RR mice after antibiotic treatment alone and subsequent CDI (Figures 6e and f). In the case of bone marrow neutrophils, the effect of antibiotics on CXCR2 expression was compounded by CDI (Figure 6e). Consistent with more neutrophils (and not monocytes) in RR mice, the increased expression of CXCR2 was seen only on RR neutrophils, and not on bone marrow monocytes (Figure 6g). To study the role of CXCR2 in regulating neutrophil recruitment to cecum after CDI, we used a selective non-peptide inhibitor that blocks CXCR2 signaling (SB225002). Within 1 day of C. difficile challenge, MPO activity was induced in cecal tissue of mice (*P<0.05; Figure 6h). Blocking CXCR2 signaling by intra-peritoneal injection of SB225002 (1 mg kg−1 per day) for 2 days prior to CDI reduced MPO activity in cecal tissue as compared with vehicle-treated controls (**P<0.01; Figure 6h). Our data thus demonstrate a critical role for CXCR2 signaling in neutrophil recruitment to colonic tissue after CDI and show that LEPR SNP influences CXCR2 expression on bone marrow and blood neutrophils during the course of antibiotics and after CDI.
Differential dysbiosis of gut microbiota regulates bone marrow neutrophil CXCR2 expression
Antibiotic-induced dysbiosis was sufficient to induce CXCR2 expression in RR mice (Figure 4e). We thus determined the microbial composition of cecal contents in QQ and RR mice (both prior to antibiotics, and after antibiotics and CDI) by shot-gun sequencing. Before antibiotics, RR mice had a slightly more diverse flora compared with QQ mice and cefoperazone treatment reduced the microbial diversity in both groups of mice (Figure 7a). Notably, the phylum composition was significantly different between QQ and RR mice (P<0.05; Figure 7b): before antibiotics, RR mice had relatively fewer Bacteroidetes and more Firmicutes than QQ mice, and after cefoperazone Bacteroidetes abundance decreased further in RR mice (Figure 7b). Although CDI decreased Bacteroidetes in QQ mice, this phylum was almost completely lost in C. difficile-infected RR mice (Figures 7b and c). To determine the role of microbiota in regulating CXCR2 expression, we matched the microbial flora of QQ and RR mice by daily bedding exchange as previously described.29 Reciprocal transfer of microbial flora between QQ and RR mice during antibiotic pre-treatment resulted in similar levels of CXCR2 expression on QQ and RR bone marrow neutrophils, both after antibiotic treatment and after subsequent CDI (Figures 7d and e). These findings indicate that antibiotic-induced changes in composition of gut microbiota direct CXCR2 expression on bone marrow neutrophils.
Differential dysbiosis of gut microbiota regulates bone marrow neutrophil CXCR2 expression. (a) Changes in the Shannon diversity indices (SDI), (b) percent relative abundance of different phyla, and (c) Firmicutes to Bacteroidetes ratio phyla among gut microbiota of mice at baseline, after antibiotics (day 0) and after C. difficile infection (day 1) (n=3 mice per group). Data shown as mean±s.e.m.*P<0.05 at baseline, $P<0.05 after cefoperazone treatment, and #P<0.05 at day 1 of CDI (Students’ t test). Bedding was exchanged daily between QQ and RR mice for the entire duration of antibiotics (9 days) and CXCR2 expression on bone marrow neutrophils were analyzed by flow cytometry (d) after antibiotics and (e) after C. difficile infection (Day 1). Data shown as mean±s.e.m. from 3 to 8 mice per group. (*P<0.05; Students’ t-test).
Discussion
The most important finding of our studies is that a common SNP that is present in up to 50% of humans influences CDI-induced neutrophil responses in both humans and mice, and the mechanism of enhanced neutrophilia associated with the LEPR SNP is dependent on gut microbiota-induced expression of a neutrophil-recruiting CXCR2. Host genetics, immunity, and gut microbiome are intricately linked. Genetic make-up influences immune responses to infections and microbiota composition,30, 31 microbiota re-programs host genes by epigenetic modifications32 and shapes immunity, and the immune system in turn alters composition of the gut microbial communities.33, 34 Notably, all of these variables clearly influence CDI pathogenesis and outcomes as well.35 This study thus improves our understanding of how interactions between host genome and gut microbiome influence neutrophil response to C. difficile and impact CDI pathogenesis and clinical disease outcomes.
The exaggerated neutrophilic response after CDI associated with RR genotype was seen in both humans and mice. The WBC cutoff value of 20 × 109 l−1 that we used for our association studies has previously been shown to predict increased 30-day mortality in patients with CDI,9 and suggests that RR patients are likely to have higher mortality after CDI. While we did not have mortality data from our patient cohort, mortality was indeed seen in RR mice. Overall mortality seen in our animal studies was modest but this likely owing to the genetic background of QQ and RR mice (129J). In multiple studies using the same infection protocol, we have seen that mice on C57Bl/6 genetic background are more susceptible to CDI and have higher mortality. Regardless, across six different experiments and total N=86 mice, only RR mice succumbed to infection, and all QQ mice survived. In addition, the inflammatory response (as measured by cytokine expression and blood and tissue neutrophils) was clearly exaggerated in RR mice, compared with QQ mice. We did not see any difference in C. difficile (or its toxin) in the cecal contents of QQ and RR mice, but it is known that an over-exuberant neutrophil response can cause collateral host damage36 and increase mortality after CDI.9 Thus, our data indicate that the tissue damage and survival disadvantage seen in RR mice was owing to host-derived factors, that is, enhanced inflammation and surge in neutrophil infiltration. Of note, the surviving RR mice have slightly faster disease resolution as compared with QQ mice: decrease in tissue neutrophil infiltrate in RR mice on day 3 compared with day 1 after infection (Figure 3c), and faster weight gain (Figure 4d). This observation raises the intriguing possibility that a threshold effect based on host genetic polymorphism and magnitude of inflammatory response exists, and can influence CDI outcomes. Too much inflammation early in the course of disease can increase mortality but if the host survives the initial insult, outcomes are better (as seen in RR mice). On the other hand, slightly lower-level inflammation, which is persistent leads to better overall survival but longer duration of clinical disease (as seen in QQ mice).
At the mechanistic level, we found that CXCR2 signaling pathway is critical for colonic tissue recruitment of neutrophils after CDI, and the higher CXCR2 expression on RR neutrophils was mediated by gut microbiota. However, CXCR2 inhibition did not alter CDI disease severity during the early stage of infection (day 1 after challenge). Despite a complete lack of neutrophil infiltration to cecal tissue, mice with CXCR2 blockage had similar disease expression (as measured by weight loss and reduction in colon length, Supplementary Figure S4), as compared with vehicle-treated control mice. As both neutrophilia and neutropenia in patients (and mice) is associated with adverse outcomes after CDI,15, 16, 17, 37 this result is not entirely unexpected, and in fact underscores an important role of optimal neutrophil numbers in determining CDI outcomes. Thus, to define the role of CXCR2 in modulating neutrophil hoemostasis and impacting CDI susceptibility and disease severity, appropriate titration of the levels of CXCR2 inhibitor (and/or blocking antibody) will be needed.
A growing body of evidence indicates that gut microbiota influences inflammatory responses38 including neutrophil production, migration, and function.39, 40, 41 Our studies add to the current literature and show that antibiotic- and CDI-induced dysbiosis (specifically in the context of RR genotype) enhances CXCR2 on cell surface of bone marrow and blood neutrophils, and influences neutrophil migration from bone marrow. Prior to antibiotics, composition of gut microbial community was already different between QQ and RR mice, and RR mice had relatively higher abundance of Firmicutes phylum and lower abundance of Bacteroidetes phylum (Figure 7c). The increased ratio of Firmicutes to Bacteroidetes in RR mice was amplified after CDI (Figure 7c). Notably, exchange of microbiota between QQ and RR mice reversed the antibiotic- and CDI-induced differences in neutrophil CXCR2 expression. Thus, our data indicate that microbiota has a key role in regulating CXCR2 expression and are in concert with previous reports in animal models which show that dysbiosis in pregnant mice can impact bone marrow CXCR2 expression in offspring.40 But additionally our results highlight a critical role of host genetic polymorphism in regulating gut microbiota-mediated alteration in neutrophil chemokine receptor expression.
Somewhat contrary to our observations, a recent report has shown evidence of CXCR2 downregulation on blood neutrophils subsequent to antibiotic treatment.42 However, we used a single antibiotic, cefoperazone, whereas a cocktail of antibiotics comprising of ampicillin, neomycin, metronidazole, and vancomycin was used by Watanabe. et al.,42 which could contribute to opposing results. In fact, it is known that different antibiotic regimes can induce distinct perturbations in gut microbiota structure,43 and contrasting the findings from our study to Schubert et al.43 suggests that use of multiple antibiotic cocktail induces a more profound disruption of microbial communities as compared to cefoperazone alone. Although antibiotic treatment decreases the overall microbial diversity and reduces the abundance of many major bacterial phyla, proportion of some bacterial communities also increases. For example, Verrucomicrobia phyla is retained after cefoperazone treatment and its proportion is higher in RR mice (Figure 7b) but this phylum is completely abolished by metronidazole43 (one of the antibiotic used by Watanabe et al.). Of note, Akkermansia muciniphila is the predominant commensal species present in Verrucomicrobia phyla, and presence of A. muciniphila in microbiota enhances gut inflammation (including pro-inflammatory cytokine production and immune cells recruitment) and colonic tissue damage after Salmonella infection in mice.44 Thus, it is possible that the microbial communities that survive (or increase in relative proportion) after specific antibiotics are responsible for differences in neutrophil CXCR2 expression after CDI. Although transfer of “whole bacterial communities” by bedding exchange supports an important role for gut microbiota in regulating CXCR2 expression, shotgun sequencing data presented here has a relatively smaller sample size (n=3). Thus, a potential limitation of our study is the inability to establish associations between individual bacterial genera (or species) and neutrophil CXCR2 expression. Future studies with a higher sample size will be needed to identify specific microbial communities that regulate CXCR2 expression and promote neutrophil trafficking from bone marrow in RR mice.
In sum, our data support a scenario whereby host genetic cues (homozygosity for the mutant LEPR SNP, RR genotype) alters microbiota prior to antibiotics. Antibiotics further disrupt the microbiota structure and change the microbial composition that induces CXCR2 expression on bone marrow neutrophils of RR mice, and primes them for release. A secondary insult after antibiotics with C. difficile further increases CXCR2 expression and in conjunction with increased chemokines (CXCL1 and 2), manifests as increased neutrophil numbers in peripheral blood and tissue of RR mice. There is no impact on pathogen burden but the exaggerated inflammation in RR mice can then lead to increased mortality. Our study provides novel insights into how antibiotic-induced dysbiosis alters host neutrophil responses in the context of a specific SNP and influences clinical disease outcomes. Of note, both LEPR Q223R SNP and antibiotic-mediated dysbiosis are very common in our patient populations, and CXCR2-induced neutrophil trafficking from bone marrow to blood and tissue is a fundamental biological response to both infectious (e.g., influenza virus45), and inflammatory (e.g. dextran sulphate sodium-induced colitis46) stimuli. Thus, our study has important implications beyond CDI as well, and LEPR Q223R SNP has the potential to be used as a genetic biomarker to predict neutrophil responses to various diseases.
Methods
Human data collection and analysis
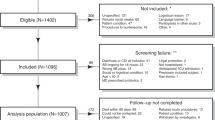
Discarded blood clot samples were collected from 156 consecutive C. difficile-positive patients at the UVA Medical Center, and DNA was extracted using Qiagen DNeasy Blood and Tissue kit, followed by LEPR SNP typing at the UVA bioinformatics core. Of these patients, clinical data (including gender, ethnicity, and daily WBC counts for the same admission as the CDI diagnosis) was available from 129 adults (age >18 years) in the UVA clinical database repository. As clinical data were collected retrospectively, availability of daily WBC counts was at the discretion of ordering physician, and we did not have daily blood count values for all patients. Thus, to get a peak WBC value for association analysis, we included data only from patients who had a minimum of four consecutive daily WBC count values. Thus, 19 patients were excluded and we had N=110 as our final study population. A more rigorous analysis where only patients with a minimum of five consecutive daily WBC counts (N=96) were included did not change our results. Patient data collection and analysis was approved by the University of Virginia Institutional Review Board (IRB-HSR #16926).
Mouse model of CDI
Mice homozygous for the Q223 or R223 LEPR allele (on 129/J background) were maintained and bred at the Department of Laboratory Animal Medicine, University of Cincinnati, accredited by the American Association for Accreditation of Laboratory Animal Care (Frederick, MD, USA), under pathogen-free conditions in individually ventilated cages. C. difficile (VPI 10463) spores were prepared for infection as previously described.11 Age-matched QQ and RR mice were treated with cefoperazone and challenged with purified C. difficile spores (1 × 106 per mouse) by oral gavage as previously described (Figure 1a).19 After infection, mice were single caged to prevent cross-infection and were monitored daily. In experiments performed to determine the impact of microbiota on CXCR2 expression, bedding was exchanged every day between QQ and RR mice throughout the course of antibiotics to equilibrate microbiota.
Estimation of C. difficile load
Pathogen load of C. difficile in mice was determined by plating 1:10 dilutions of cecal contents on beef heart infusion supplement plates containing taurocholate. Plates were incubated anaerobically at 37 °C for 24–48 h and colonies were counted manually to enumerate colony forming units per gram of cecal content. Level of toxins in cecal contents were determined using the C. difficile TOXA/B ELISA (TechLab, VA, USA) according to manufacturer’s instructions.
Histopathology
Tissue samples were fixed in Bouin’s solution (Sigma, St. Louis, MO, USA), washed, and dehydrated in 70% ethanol prior to paraffin embedding. Sections were prepared and stained with hematoxylin and eosin. The slides were examined microscopically and scored for inflammatory cell infiltration, edema, and epithelial disruption. A score of 0–4, denoting increasingly severe abnormality, was assigned by pathologist blinded to the identity of the samples.
Cell enumerations and flow cytometry
Peripheral blood was obtained by intra-cardiac puncture and collected in ethylenediaminetetraacetic acid microtainers (BD Biosciences, CA, USA). Bone marrow cells were harvested by flushing single femur and tibia with ice cold phosphate-buffered saline containing 2% fetal bovine serum (Thermo Fisher Scientific, MA, USA). Total and differential cell count was determined using a Hemavet hematology analyzer with veterinary software (Drew Scientific Inc., CT, USA).
Lamina propria cells were isolated and analyzed by flow cytometry as previously described44 and in Supplementary methods. Apoptosis of cecal tissue neutrophils was enumerated using Annexin V/7AAD-apoptosis assay kit (BD biosciences) as per manufacturer’s instructions. Flow cytometry of apoptosis assay was performed on a BD FACS Acuri C6 flow cytometer equipped with CFlow Plus (BD Biosciences) software and analyzed using FlowJo V.10 (Tree Star, OR, USA).
Estimation of inflammatory markers and neutrophil functional assays
Leptin, CXCL1, CXCL2, G-CSF, and GM-CSF were measured by ELISA following protocols provided by manufacturer (for leptin; Peprotech, NJ, USA, and for all other targets; R&D systems, MN, USA). Preparation of tissue and plasma samples for ELISA is described in supplementary methods. RNA from tissue samples was extracted using Qiagen RNEasy Plus Mini Kit (Qiagen, CA, USA) and expression of inflammatory markers were estimated by TaqMan qRT PCR. Cells from tissue and bone marrow were also used for functional assays (detailed in Supplementary methods).
Microbiota analysis
DNA was extracted from cecal contents using PowerFecal DNA isolation kit (MO BIO, CA, USA) as per manufacturer’s instructions. Library generation was performed using dual NexteraXT adapters followed by sequencing on the NextSeq 500 Illumina platform in the Precision Metagenomic Core Laboratory at CCHMC for 150 bp paired end reads with a depth of sequencing targeting 10 million reads per sample. Annotation pipeline analysis for all samples was performed as previously described.47
Statistical analysis
All statistical analysis were performed using Graph Pad Prism 5.0 software (Graph pad software Corporation, Inc, CA, USA). For comparison of groups, a Student’s t-test or ANOVA with Bonferroni correction was used. A P value below 0.05 was considered significant.
References
Dubberke, E. Clostridium difficile infection: the scope of the problem. J. Hosp. Med. 7 (Suppl 3), S1–S4 (2012).
Lessa, FC et al. Burden of Clostridium difficile infection in the United States. N. Engl. J. Med. 372, 825–834 (2015).
Jiang, ZD et al. A common polymorphism in the interleukin 8 gene promoter is associated with Clostridium difficile diarrhea. Am. J. Gastroenterol. 101, 1112–1116 (2006).
Madan, R et al. Role of leptin-mediated colonic inflammation in defense against Clostridium difficile colitis. Infect. Immun. 82, 341–349 (2014).
Duggal, P et al. A mutation in the leptin receptor is associated with Entamoeba histolytica infection in children. J. Clin. Investig. 121, 1191–1198 (2011).
Bracho-Riquelme, RL, Loera-Castaneda, V, Torres-Valenzuela, A, Loera-Castaneda, GA & Sanchez-Ramirez, JP. Leptin and leptin receptor polymorphisms are associated with poor outcome (death) in patients with non-appendicular secondary peritonitis. Crit. Care 15, R227 (2011).
Perez-Cobas, AE, Artacho, A, Ott, SJ, Moya, A, Gosalbes, MJ & Latorre, A. Structural and functional changes in the gut microbiota associated to Clostridium difficile infection. Front. Microbiol. 5, 335 (2014).
El Feghaly, RE, Bangar, H & Haslam, DB. The molecular basis of Clostridium difficile disease and host response. Curr. Opin. Gastroenterol 31, 24–29 (2015).
Solomon, K et al. Mortality in patients with Clostridium difficile infection correlates with host pro-inflammatory and humoral immune responses. J. Med. Microbiol. 62 (Pt 9), 1453–1460 (2013).
Voth, DE & Ballard, JD. Clostridium difficile toxins: mechanism of action and role in disease. Clin.Microbiol. Rev. 18, 247–263 (2005).
McDermott, AJ et al. The role of Gr-1(+) cells and tumour necrosis factor-alpha signalling during Clostridium difficile colitis in mice. Immunology 144, 704–716 (2015).
Farooq, PD, Urrunaga, NH, Tang, DM & von Rosenvinge, EC. Pseudomembranous colitis. Dis. Mon. 61, 181–206 (2015).
Kelly, CP et al. Neutrophil recruitment in Clostridium difficile toxin A enteritis in the rabbit. J. Clin. Invest. 93, 1257–1265 (1994).
Qiu, B, Pothoulakis, C, Castagliuolo, I, Nikulasson, S & LaMont, JT. Participation of reactive oxygen metabolites in Clostridium difficile toxin A-induced enteritis in rats. Am. J. Physiol 276 (2 Pt 1), G485–G490 (1999).
Luo, R, Greenberg, A & Stone, CD. Outcomes of Clostridium difficile infection in hospitalized leukemia patients: a nationwide analysis. Infect. Control Hosp. Epidemiol. 36, 794–801 (2015).
Huang, AM, Marini, BL, Frame, D, Aronoff, DM & Nagel, JL. Risk factors for recurrent Clostridium difficile infection in hematopoietic stem cell transplant recipients. Transpl. Infect. Dis. 16, 744–750 (2014).
Jarchum, I, Liu, M, Shi, C, Equinda, M & Pamer, EG. Critical role for MyD88-mediated neutrophil recruitment during Clostridium difficile colitis. Infect. Immun. 80, 2989–2996 (2012).
Na, X et al. A multi-center prospective derivation and validation of a clinical prediction tool for severe clostridium difficile infection. PloS one 10, e0123405 (2015).
Theriot, CM, Koumpouras, CC, Carlson, PE, Bergin II, Aronoff, DM & Young, VB. Cefoperazone-treated mice as an experimental platform to assess differential virulence of Clostridium difficile strains. Gut Microbes 2, 326–334 (2011).
Abella, V et al. Leptin in the interplay of inflammation, metabolism and immune system disorders. Nat. Rev. Rheumatol. 13, 100–109 (2017).
Zastrow, O et al. The soluble leptin receptor is crucial for leptin action: evidence from clinical and experimental data. Int. J. Obes. Relat. Metab. Disord 27, 1472–1478 (2003).
Marie, CS, Verkerke, HP, Paul, SN, Mackey, AJ & Petri, WA Jr. Leptin protects host cells from Entamoeba histolytica cytotoxicity by a STAT3-dependent mechanism. Infect. Immun. 80, 1934–1943 (2012).
Mancuso, P et al. Disruption of leptin receptor-STAT3 signaling enhances leukotriene production and pulmonary host defense against pneumococcal pneumonia. J. Immunol. 186, 1081–1090 (2011).
Pulli, B et al. Measuring myeloperoxidase activity in biological samples. PloS ONE 8, e67976 (2013).
Gregory, AD, Hogue, LA, Ferkol, TW & Link, DC. Regulation of systemic and local neutrophil responses by G-CSF during pulmonary Pseudomonas aeruginosa infection. Blood 109, 3235–3243 (2007).
Manz, MG & Boettcher, S. Emergency granulopoiesis. Nat. Rev. Immunol. 14, 302–314 (2014).
Bento, AF, Leite, DF, Claudino, RF, Hara, DB, Leal, PC & Calixto, JB. The selective nonpeptide CXCR2 antagonist SB225002 ameliorates acute experimental colitis in mice. J. Leukoc. Biol. 84, 1213–1221 (2008).
Eash, KJ, Greenbaum, AM, Gopalan, PK & Link, DC. CXCR2 and CXCR4 antagonistically regulate neutrophil trafficking from murine bone marrow. J. Clin. Invest. 120, 2423–2431 (2010).
Hildebrand, F et al. Inflammation-associated enterotypes, host genotype, cage and inter-individual effects drive gut microbiota variation in common laboratory mice. Genome Biol. 14, R4 (2013).
Chapman, SJ & Hill, AV. Human genetic susceptibility to infectious disease. Nat. Rev. Genet. 13, 175–188 (2012).
Bonder, MJ et al. The effect of host genetics on the gut microbiome. Nat. Genet. 48, 1407–1412 (2016).
Woo, V & Alenghat, T. Host-microbiota interactions: epigenomic regulation. Curr. Opin. Immunol. 44, 52–60 (2017).
Chung, H et al. Gut immune maturation depends on colonization with a host-specific microbiota. Cell 149, 1578–1593 (2012).
Zhang, H & Luo, XM. Control of commensal microbiota by the adaptive immune system. Gut Microbes 6, 156–160 (2015).
Sorensen, TI, Nielsen, GG, Andersen, PK & Teasdale, TW. Genetic and environmental influences on premature death in adult adoptees. N. Engl. J. Med. 318, 727–732 (1988).
Smith, JA. Neutrophils, host defense, and inflammation: a double-edged sword. J. Leukoc. Biol 56, 672–686 (1994).
Fuereder, T et al. Risk factors for Clostridium difficile infection in hemato-oncological patients: a case control study in 144 patients. Sci. Rep. 6, 31498 (2016).
Maslowski, KM et al. Regulation of inflammatory responses by gut microbiota and chemoattractant receptor GPR43. Nature 461, 1282–1286 (2009).
Balmer, ML et al. Microbiota-derived compounds drive steady-state granulopoiesis via MyD88/TICAM signaling. J. Immunol. 193, 5273–5283 (2014).
Deshmukh, HS et al. The microbiota regulates neutrophil homeostasis and host resistance to Escherichia coli K1 sepsis in neonatal mice. Nat. Med. 20, 524–530 (2014).
Clarke, TB, Davis, KM, Lysenko, ES, Zhou, AY, Yu, Y & Weiser, JN. Recognition of peptidoglycan from the microbiota by Nod1 enhances systemic innate immunity. Nat. Med. 16, 228–231 (2010).
Watanabe, K et al. Microbiome-mediated neutrophil recruitment via CXCR2 and protection from amebic colitis. PLoS Pathog. 13, e1006513 (2017).
Schubert, AM, Sinani, H & Schloss, PD. Antibiotic-induced alterations of the murine gut microbiota and subsequent effects on colonization resistance against Clostridium difficile. mBio 6, e00974 (2015).
Ganesh, BP, Klopfleisch, R, Loh, G & Blaut, M. Commensal Akkermansia muciniphila exacerbates gut inflammation in Salmonella Typhimurium-infected gnotobiotic mice. PloS ONE 8, e74963 (2013).
Wareing, MD, Shea, AL, Inglis, CA, Dias, PB & Sarawar, SR. CXCR2 is required for neutrophil recruitment to the lung during influenza virus infection, but is not essential for viral clearance. Viral Immunol. 20, 369–378 (2007).
Farooq, SM, Stillie, R, Svensson, M, Svanborg, C, Strieter, RM & Stadnyk, AW. Therapeutic effect of blocking CXCR2 on neutrophil recruitment and dextran sodium sulfate-induced colitis. J. Pharmacol. Exp. Ther. 329, 123–129 (2009).
Andersen, H et al. Use of shotgun metagenome sequencing to detect fecal colonization with multidrug-resistant bacteria in children. J. Clin. Microbiol. 54, 1804–1813 (2016).
Acknowledgements
Human samples and data were collected in the laboratory of Dr. William A. Petri Jr. (University of Virginia) and financially supported by R01 AI-124214 to WAP. We thank TechLab, Inc. for generously providing TOX A/B ELISA kits. We would like to thank George S. Deepe Jr. (UC) and Senad Divanovic and Marie-Dominique Filippi (both at CCHMC) for critical review of the manuscript and valuable discussions; and Roman Jandarov (UC) for performing statistical analysis of patient data. We also thank the Live Microscopy Core in the department of Molecular and Cellular Physiology at UC and Research Flow Cytometry Core in the Division of Rheumatology at CCHMC for their assistance. This work was supported by the National Institutes of Health (NIH) K08-AI108801-01 to Rajat Madan. Microbiome analysis was supported by the NIH (T32ES010957-14) and the Centers for Disease Control (CDC) AR funding through a Broad Agency Announcement (200-2016-91939). This project was supported in part by PHS Grant P30 DK078392 (Research Pathology and Research Flow Cytometry Core) of the Digestive Disease Research Core Center in Cincinnati.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Author contributions
R.M. conceived the study and obtained funding. S.J. and R.M. designed the experiments and analyzed the data. S.J. conducted mouse studies. M.M.A. and R.M. collected and analyzed human data. A.M. and J.X. maintained the mouse colonies and assisted in experiments. H.A. and D.B.H. performed the shotgun sequencing and microbiota analysis. S.J. and R.M. wrote the manuscript.
SUPPLEMENTARY MATERIAL is linked to the online version of the paper
Supplementary information
Rights and permissions
About this article
Cite this article
Jose, S., Abhyankar, M., Mukherjee, A. et al. Leptin receptor q223r polymorphism influences neutrophil mobilization after Clostridium difficile infection. Mucosal Immunol 11, 947–957 (2018). https://doi.org/10.1038/mi.2017.119
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/mi.2017.119