Abstract
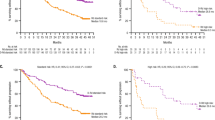
Polymerase chain reaction (PCR)-based minimal residual disease (MRD) analysis is a useful prognostic tool in multiple myeloma (MM), although its long-term impact still needs to be addressed. This report presents the updated results of the GIMEMA-VEL-03-096 trial. Thirty-nine MM patients receiving bortezomib–thalidomide–dexamethasone after autologous transplantation were monitored for MRD by both nested and real-time quantitative-PCR until relapse. Our data confirm the strong impact of MRD on survival: overall survival was 72% at 8 years median follow-up for patients in major MRD response versus 48% for those experiencing MRD persistence (P=0.041). In addition, MRD kinetics resulted predictive for relapse: indeed median remission duration was not reached for patients in major MRD response, 38 months for those experiencing MRD reappearance and 9 months for patients with MRD persistence (P<0.001). Moreover: (1) 26 patients achieving major MRD response (67%) benefit of excellent disease control (median TNT: 42 months); (2) MRD reappearance heralds relapse, with a TNT comparable to that of MRD persistence (9 versus 10 months, P=0.706); (3) the median lag between MRD reappearance and need for salvage treatment is 9 months. These results suggest the usefulness of a long-term MRD monitoring in MM patients and the need for maintenance or pre-emptive treatments ensuring durable responses.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Kumar SK, Rajkumar SV, Dispenzieri A, Lacy MQ, Hayman SR, Buadi FK et al. Improved survival in multiple myeloma and the impact of novel therapies. Blood 2008; 111: 2516–2520.
Palumbo A, Anderson K . Multiple myeloma. N Engl J Med 2011; 364: 1046–1060.
Chanan-Khan AA, Giralt S . Importance of achieving a complete response in multiple myeloma, and the impact of novel agents. J Clin Oncol 2010; 28: 2612–2624.
Paiva B, Vidriales MB, Cerveró J, Mateo G, Pérez JJ, Montalbán MA et al. Multiparameter flow cytometric remission is the most relevant prognostic factor for multiple myeloma patients who undergo autologous stem cell transplantation. Blood 2008; 112: 4017–4023.
Ladetto M, Pagliano G, Ferrero S, Cavallo F, Drandi D, Santo L et al. Major tumor shrinking and persistent molecular remissions after consolidation with bortezomib, thalidomide, and dexamethasone in patients with autografted myeloma. J Clin Oncol 2010; 28: 2077–2084.
Terragna C, Zamagni E, Petrucci MT, Durante S, Patriarca F, Narni F et al. Molecular remission after bortezomib-thalidomide-dexamethasone compared with thalidomide-dexamethasone as consolidation therapy following double autologous transplantation for multiple myeloma: results of a qualitative and quantitative analysis. [abstract]. Blood 2010; 116: abstract 861.
Korthals M, Sehnke N, Kronenwett R, Bruns I, Mau J, Zohren F et al. The level of minimal residual disease in the bone marrow of patients with multiple myeloma before high-dose therapy and autologous blood stem cell transplantation is an independent predictive parameter. Biol Blood Marrow Transplant 2012; 18: 423–431.e3.
Paiva B, Gutiérrez NC, Rosiñol L, Vídriales MB, Montalbán MÁ, Martínez-López J et al. High-risk cytogenetics and persistent minimal residual disease by multiparameter flow cytometry predict unsustained complete response after autologous stem cell transplantation in multiple myeloma. Blood 2012; 119: 687–691.
Kröger N, Badbaran A, Zabelina T, Ayuk F, Wolschke C, Alchalby H et al. Impact of high-risk cytogenetics and achievement of molecular remission on long-term freedom from disease after autologous-allogeneic tandem transplantation in patients with multiple myeloma. Biol Blood Marrow Transplant 2013; 19: 398–404.
Ladetto M, Ferrero S, Drandi D, Omedè P, Patriarca F, Mordini N et al. High rates of prolonged molecular remissions after tandem autologous-nonmyeloablative allografting in newly diagnosed myeloma. ASH Annu Meet Abstr 2012; 120: 4204.
Korthals M, Sehnke N, Kronenwett R, Schroeder T, Strapatsas T, Kobbe G et al. Molecular monitoring of minimal residual disease in the peripheral blood of patients with multiple myeloma. Biol Blood Marrow Transplant 2013; 19: 1109–1115.
Puig N, Sarasquete ME, Balanzategui A, Martínez J, Paiva B, García H et al. Critical evaluation of ASO RQ-PCR for minimal residual disease evaluation in multiple myeloma. A Comparative Analysis with Flow Cytometry. Leukemia 2014; 28: 391–397.
Voena C, Ladetto M, Astolfi M, Provan D, Gribben JG, Boccadoro M et al. A novel nested-PCR strategy for the detection of rearranged immunoglobulin heavy-chain genes in B cell tumors. Leukemia 1997; 11: 1793–1798.
Ladetto M, Donovan JW, Harig S, Trojan A, Poor C, Schlossnan R et al. Real-time polymerase chain reaction of immunoglobulin rearrangements for quantitative evaluation of minimal residual disease in multiple myeloma. Biol Blood Marrow Transplant 2000; 6: 241–253.
van der Velden VH, Cazzaniga G, Schrauder A, Hancock J, Bader P, Panzer-Grumayer ER et al. Analysis of minimal residual disease by Ig/TCR gene rearrangements: guidelines for interpretation of real-time quantitative PCR data. Leukemia 2007; 21: 604–611.
Rajkumar SV, Gahrton G, Bergsagel PL . Approach to the treatment of multiple myeloma: a clash of philosophies. Blood 2011; 118: 3205–3211.
Andersen NS, Pedersen LB, Laurell A, Elonen E, Kolstad A, Boesen AM et al. Pre-emptive treatment with rituximab of molecular relapse after autologous stem cell transplantation in mantle cell lymphoma. J Clin Oncol 2009; 27: 4365–4370.
Topp MS, Gökbuget N, Zugmaier G, Degenhard E, Goebeler ME, Klinger M et al. Long-term follow-up of hematologic relapse-free survival in a phase 2 study of blinatumomab in patients with MRD in B-lineage ALL. Blood 2012; 120: 5185–5187.
Ferrero S, Monitillo L, Mantoan B, Barbero D, Genuardi E, Barbiero S et al. Rituximab-based pre-emptive treatment of molecular relapse in follicular and mantle cell lymphoma. Ann Hematol 2013; 92: 1503–1511.
Ferrero S, Drandi D, Mantoan B, Ghione P, Omedè P, Ladetto M . Minimal residual disease detection in lymphoma and multiple myeloma: impact on therapeutic paradigms. Hematol Oncol 2011; 29: 167–176.
Martinez-Lopez J, Lahuerta JJ, Pepin F, González M, Barrio S, Ayala R et al. Prognostic value of deep sequencing method for minimal residual disease detection in multiple myeloma. Blood 2014; 123: 3073–3079.
Vij R, Mazumder A, Klinger M, O'Dea D, Paasch J, Martin T et al. Deep sequencing reveals myeloma cells in peripheral blood in majority of multiple myeloma patients. Clin Lymphoma Myeloma Leuk 2014; 14: 131–139.e1.
Ladetto M, Brüggemann M, Monitillo L, Ferrero S, Pepin F, Drandi D et al. Next-generation sequencing and real-time quantitative PCR for minimal residual disease detection in B-cell disorders. Leukemia 2013; 28: 1299–1307.
Martinez-Lopez J, Fulciniti M, Barrio S, Carlton V, Moorhead M, Lahuerta JJ et al. Deep sequencing reveals oligoclonality at the immunoglobulin locus in multiple myeloma patients. [abstract]. Blood 2013; 122: 401.
Acknowledgements
We would like to thank the patients, nurses, physicians and data managers (Tiziana Marangon, Debora Caldarazzo and Antonella Fiorillo). This work was supported by Progetto di Rilevante Interesse Nazionale (PRIN 2009) from Ministero Italiano dell' Università e della Ricerca (MIUR), Roma, Italy (code: 7.07.02.60 AE01), Progetti di Ricerca Finalizzata 2008, head unit: IRCCS Centro di Riferimento Oncologico della Basilicata (CROB), Rionero in Vulture (Potenza), Italy (code: 7.07.08.60 P49), Progetto di Ricerca Sanitaria Finalizzata 2008, head unit: Divisione di Ematologia S. Cortellazzo, A. O. S. Maurizio, Bolzano/Bozen, Italy, (code: 7.07.08.60 P51), Progetto di Ricerca Sanitaria Finalizzata 2009, head unit: Divisione di Ematologia S. Cortellazzo, A. O. S. Maurizio, Bolzano/Bozen, Italy (code: RF-2009-1469205), Progetto di Ricerca Sanitaria Finalizzata 2010 (head unit: Divisione di Ematologia, A. O. S. Maurizio, Bolzano/Bozen, Italy, code: RF-2010-2307262), Progetti di Ateneo 2012 - Finanziatore Compagnia di San Paolo (code: TO_call03_2012_0055), Fondi di Ricerca Locale, Università degli Studi di Torino, Torino, Italy and Fondazione Neoplasie del Sangue (FO. NE. SA),Torino, Italy.
Disclaimer
This manuscript is an original paper and has not submitted or published in its current format anywhere else.
Author Contributions
ML, AP and MB designed the study. SF and ML wrote the report. AP supervised the clinical conduction of the study and data analysis. ML, SF and DD supervised the laboratory procedures. SF, FC, MU, SC, CT and SO supervised data collection, analyzed the data, and reviewed and assisted in writing the manuscript. DD and EG undertook the experimental procedures. RP and SF did the statistical analysis. FC, MG, FR, TG, CG, AML, VC, TC, CC, LDR, FP, APF, PP and PM recruited the patients.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
ML—Celgene, Jannsen Cilag, Mundipharma, Roche and Amgen: research funding, speaker's bureau. FC—Celgene and Jannsen Cilag: consultancy membership on an entity's Board of Directors and advisory committees. TC—Celgene: honoraria, research funding, Jannsen Cilag: honoraria. TG—Celgene: research funding. PM—Celgene: honoraria, research funding. MB—Celgene: consultancy, membership on an entity’s Board of Directors or advisory committees, research funding; Jannsen Cilag: consultancy, membership on an entity’s Board of Directors or advisory committees, research funding. AP—Bristol–Myers Squibb, Celgene, Janssen Pharmaceuticals, Onyx and Amgen: consultancy, honoraria. The remaining authors declare no conflict of interest.
Additional information
Data from interim analyses were presented as abstracts at the 2009, 2011 and 2013 American Society of Hematology (ASH) meetings and at the 2014 European Hematology Association (EHA) meeting.
Rights and permissions
About this article
Cite this article
Ferrero, S., Ladetto, M., Drandi, D. et al. Long-term results of the GIMEMA VEL-03-096 trial in MM patients receiving VTD consolidation after ASCT: MRD kinetics' impact on survival. Leukemia 29, 689–695 (2015). https://doi.org/10.1038/leu.2014.219
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/leu.2014.219
This article is cited by
-
Impact of minimal residual disease (MRD) in salvage autologous stem cell transplantation for relapsed myeloma: results from the NCRI Myeloma X (intensive) trial
Bone Marrow Transplantation (2024)
-
Longitudinal minimal residual disease assessment in multiple myeloma patients in complete remission – results from the NMSG flow-MRD substudy within the EMN02/HO95 MM trial
BMC Cancer (2022)
-
HLA class I-restricted T cell epitopes isolated and identified from myeloid leukemia cells
Scientific Reports (2019)
-
Methods and role of minimal residual disease after stem cell transplantation
Bone Marrow Transplantation (2019)
-
HashClone: a new tool to quantify the minimal residual disease in B-cell lymphoma from deep sequencing data
BMC Bioinformatics (2017)