Abstract
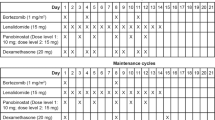
Panobinostat is a potent oral pandeacetylase inhibitor that leads to acetylation of intracellular proteins, inhibits cellular proliferation and induces apoptosis in leukemic cell lines. A phase Ia/II study was designed to determine the maximum-tolerated dose (MTD) of daily panobinostat, administered on two schedules: three times a week every week or every other week on a 28-day treatment cycle in patients with advanced hematologic malignancies. The criteria for hematologic dose-limiting toxicities differed between patients with indications associated with severe cytopenias at baseline (leukemia and myeloid disorders) and those less commonly associated with baseline cytopenias (lymphoma and myeloma). In patients with leukemia and myeloid disorders, 60 mg was the MTD for weekly as well as biweekly panobinostat. In patients with lymphoma and myeloma, 40 mg was the recommended dose for phase II evaluation (formal MTD not determined) of weekly panobinostat, and 60 mg was the MTD for biweekly panobinostat. Overall, panobinostat-related grade 3–4 adverse events included thrombocytopenia (41.5%), fatigue (21%) and neutropenia (21%). Single-agent activity was observed in several indications, including Hodgkin lymphoma and myelofibrosis. This phase Ia/II study provided a broad analysis of the safety profile and efficacy of single-agent panobinostat in patients with hematologic malignancies.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Choudhary C, Kumar C, Gnad F, Nielsen ML, Rehman M, Walther TC et al. Lysine acetylation targets protein complexes and co-regulates major cellular functions. Science 2009; 325: 834–840.
Bolden JE, Peart MJ, Johnstone RW . Anticancer activities of histone deacetylase inhibitors. Nat Rev Drug Discov 2006; 5: 769–784.
Minucci S, Pelicci PG . Histone deacetylase inhibitors and the promise of epigenetic (and more) treatments for cancer. Nat Rev Cancer 2006; 6: 38–51.
Fraga MF, Ballestar E, Villar-Garea A, Boix-Chornet M, Espada J, Schotta G et al. Loss of acetylation at Lys16 and trimethylation at Lys20 of histone H4 is a common hallmark of human cancer. Nat Genet 2005; 37: 391–400.
StatBite FDA oncology drug product approvals in 2009. J Natl Cancer Inst 2010; 102: 219.
Mann BS, Johnson JR, Cohen MH, Justice R, Pazdur R . FDA approval summary: vorinostat for treatment of advanced primary cutaneous T-cell lymphoma. Oncologist 2007; 12: 1247–1252.
Gu W, Roeder RG . Activation of p53 sequence-specific DNA binding by acetylation of the p53 C-terminal domain. Cell 1997; 90: 595–606.
Qian DZ, Kachhap SK, Collis SJ, Verheul HM, Carducci MA, Atadja P et al. Class II histone deacetylases are associated with VHL-independent regulation of hypoxia-inducible factor 1 alpha. Cancer Res 2006; 66: 8814–8821.
Qian DZ, Kato Y, Shabbeer S, Wei Y, Verheul HM, Salumbides B et al. Targeting tumor angiogenesis with histone deacetylase inhibitors: the hydroxamic acid derivative LBH589. Clin Cancer Res 2006; 12: 634–642.
Yang Y, Rao R, Shen J, Tang Y, Fiskus W, Nechtman J et al. Role of acetylation and extracellular location of heat shock protein 90alpha in tumor cell invasion. Cancer Res 2008; 68: 4833–4842.
Bali P, Pranpat M, Bradner J, Balasis M, Fiskus W, Guo F et al. Inhibition of histone deacetylase 6 acetylates and disrupts the chaperone function of heat shock protein 90: a novel basis for antileukemia activity of histone deacetylase inhibitors. J Biol Chem 2005; 280: 26729–26734.
Bishton MJ, Johnstone RW, Dickinson M, Harrison S, Prince HM . Overview of histone deacetylase inhibitors in haematological malignancies. Pharmaceuticals 2010; 3: 2674–2688.
Verheul HM, Salumbides B, Van Erp K, Hammers H, Qian DZ, Sanni T et al. Combination strategy targeting the hypoxia inducible factor-1 alpha with mammalian target of rapamycin and histone deacetylase inhibitors. Clin Cancer Res 2008; 14: 3589–3597.
Atadja P . Development of the pan-DAC inhibitor panobinostat (LBH589): successes and challenges. Cancer Lett 2009; 280: 233–241.
Prince HM, Bishton MJ, Johnstone RW . Panobinostat (LBH589): a potent pan-deacetylase inhibitor with promising activity against hematologic and solid tumors. Fut Oncol 2009; 5: 601–612.
Bradner JE, Mak R, Tanguturi SK, Mazitschek R, Haggarty SJ, Ross K et al. Chemical genetic strategy identifies histone deacetylase 1 (HDAC1) and HDAC2 as therapeutic targets in sickle cell disease. Proc Natl Acad Sci U S A 2010; 107: 12617–12622.
Babb J, Rogatko A, Zacks S . Cancer phase I clinical trials: efficient dose escalation with overdose control. Stat Med 1998; 17: 1103–1120.
Cheson BD, Bennett JM, Kopecky KJ, Buchner T, Willman CL, Estey EH et al. Revised recommendations of the International Working Group for Diagnosis, Standardization of Response Criteria, Treatment Outcomes, and Reporting Standards for Therapeutic Trials in Acute Myeloid Leukemia. J Clin Oncol 2003; 21: 4642–4649.
Tefferi A, Barosi G, Mesa RA, Cervantes F, Deeg HJ, Reilly JT et al. International Working Group (IWG) consensus criteria for treatment response in myelofibrosis with myeloid metaplasia, for the IWG for Myelofibrosis Research and Treatment (IWG-MRT). Blood 2006; 108: 1497–1503.
Cheson BD, Horning SJ, Coiffier B, Shipp MA, Fisher RI, Connors JM et al. Report of an international workshop to standardize response criteria for non-Hodgkin's lymphomas. NCI Sponsored International Working Group. J Clin Oncol 1999; 17: 1244.
Young H, Baum R, Cremerius U, Herholz K, Hoekstra O, Lammertsma AA et al. Measurement of clinical and subclinical tumour response using [18F]-fluorodeoxyglucose and positron emission tomography: review and 1999 EORTC recommendations. Eur J Cancer 1999; 35: 1773–1782.
San-Miguel JF, Richardson PGG, Sezer O, Guenther A, Siegel DSD, Blade J et al. A phase lb study of oral panobinostat and IV bortezomib in relapsed or relapsed and refractory multiple myeloma. J Clin Oncol 2011; 29, (abstract 8075).
Younes A, Sureda A, Ben-Yehuda D, Zinzani PL, Ong TC, Prince HM et al. Panobinostat in patients with relapsed/refractory Hodgkin’s lymphoma after autologous stem-cell transplantation: results of a phase II study. J Clin Oncol 2012; 30: 2197–2203.
Dickinson M, Ritchie D, DeAngelo DJ, Spencer A, Ottmann OG, Fischer T et al. Preliminary evidence of disease response to the pan deacetylase inhibitor panobinostat (LBH589) in refractory Hodgkin lymphoma. Br J Haematol 2009; 147: 97–101.
Burbury KL, Bishton MJ, Johnstone RW, Dickinson MJ, Szer J, Prince HM . MLL-aberrant leukemia: complete cytogenetic remission following treatment with a histone deacetylase inhibitor (HDACi). Ann Hematol 2010; 90: 847–889.
Richardson PG, Alsina M, Weber DM, Coutre SE, Lonial S, Gasparetto C et al. Phase II study of the pan-deacetylase inhibitor panobinostat in combination with bortezomib and dexamethasone in relapsed and bortezomib-refractory multiple myeloma (PANORAMA 2). Blood 2011; 118, (abstract 814).
Whittaker SJ, Demierre MF, Kim EJ, Rook AH, Lerner A, Duvic M et al. Final results from a multicenter, international, pivotal study of romidepsin in refractory cutaneous T-cell lymphoma. J Clin Oncol 2010; 28: 4485–4491.
Duvic M, Talpur R, Ni X, Zhang C, Hazarika P, Kelly C et al. Phase 2 trial of oral vorinostat (suberoylanilide hydroxamic acid, SAHA) for refractory cutaneous T-cell lymphoma (CTCL). Blood 2007; 109: 31–39.
Giver CR, Jaye DL, Waller EK, Kaufman JL, Lonial S . Rapid recovery from panobinostat (LBH589)-induced thrombocytopenia in mice involves a rebound effect of bone marrow megakaryocytes. Leukemia 2011; 25: 362–365.
Bishton MJ, Harrison SJ, Martin BP, McLaughlin N, James C, Josefsson EC et al. Deciphering the molecular and biological processes that mediate histone deacetylase inhibitor-induced thrombocytopenia. Blood 2011; 117: 3658–3668.
Woo MM, Culver K, Li W, Liu A, Scott J, Parker K et al. Panobinostat (LBH589) pharmacokinetics (PK): implication for clinical safety and efficacy. Ann Oncol 2008; 19, (abstract 487P).
Mascarenhas J, Mercado A, Rodriguez A, Lu M, Kalvin C, Li X et al. Prolonged low dose therapy with a pan-deacetylase inhibtor, panobinostat (LBH589), in patients with myelofibrosis. Blood 2011; 118, (abstract 794).
DeAngelo DJ, Tefferi A, Fiskus W, Mesa RA, Paley CS, Wadleigh M et al. A phase II trial of panobinostat, an orally available deacetylase inhibitor (DACi), in patients with primary myelofibrosis (PMF), post essential thrombocythemia (ET), and post polycythemia vera (PV) myelofibrosis. Blood 2010; 116, (abstract 630).
Rambaldi A, Dellacasa CM, Finazzi G, Carobbio A, Ferrari ML, Guglielmelli P et al. A pilot study of the histone-deacetylase inhibitor givinostat in patients with JAK2V617F positive chronic myeloproliferative neoplasms. Br J Haematol 2010; 150: 446–455.
Wang Y, Fiskus W, Chong DG, Buckley KM, Natarajan K, Rao R et al. Cotreatment with panobinostat and JAK2 inhibitor TG101209 attenuates JAK2V617F levels and signaling and exerts synergistic cytotoxic effects against human myeloproliferative neoplastic cells. Blood 2009; 114: 5024–5033.
Fiskus W, Verstovsek S, Manshouri T, Rao R, Balusu R, Venkannagari S et al. Heat shock protein 90 inhibitor is synergistic with JAK2 inhibitor and overcomes resistance to JAK2-TKI in human myeloproliferative neoplasm cells. Clin Cancer Res 2011; 17: 7347–7358.
Slany RK . The molecular biology of mixed lineage leukemia. Haematologica 2009; 94: 984–993.
Krivtsov AV, Feng Z, Lemieux ME, Faber J, Vempati S, Sinha AU et al. H3K79 methylation profiles define murine and human MLL-AF4 leukemias. Cancer Cell 2008; 14: 355–368.
Kalff A, Shortt J, Farr J, McLennan R, Lui A, Scott J et al. Laboratory tumor lysis syndrome complicating LBH589 therapy in a patient with acute myeloid leukaemia. Haematologica 2008; 93: e16–e17.
Schlenk RF, Krauter J, Schaich M, Bouscary D, Dombret H, Winiger IJ et al. Determination of the maximum tolerated dose of panobinostat in combination with cytarabine and mitoxantrone as salvage therapy for relapsed/refractory acute myeloid leukemia. Blood 2011; 118, (abstract 423).
Ottmann OG, DeAngelo DJ, Garcia-Manero G, Lubbert M, Jillella A, Sekeres MA et al. Determination of a phase II dose of panobinostat in combination with 5-azacitidine in patients with myelodysplastic syndromes, chronic myelomonocytic leukemia, or acute myeloid leukemia. Blood 2011; 118, (abstract 459).
Maiso P, Colado E, Ocio EM, Garayoa M, Martín J, Atadja P et al. The synergy of panobinostat plus doxorubicin in acute myeloid leukemia suggests a role for HDAC inhibitors in the control of DNA repair. Leukemia 2009; 23: 2265–2274.
Fiskus W, Buckley K, Rao R, Mandawat A, Yang Y, Joshi R et al. Panobinostat treatment depletes EZH2 and DNMT1 levels and enhances decitabine mediated de-repression of JunB and loss of survival of human acute leukemia cells. Cancer Biol Ther 2009; 8: 939–950.
Catley L, Weisberg E, Kiziltepe T, Tai YT, Hideshima T, Neri P et al. Aggresome induction by proteasome inhibitor bortezomib and alpha-tubulin hyperacetylation by tubulin deacetylase (TDAC) inhibitor LBH589 are synergistic in myeloma cells. Blood 2006; 108: 3441–3449.
Hideshima T, Richardson PG, Anderson KC . Mechanism of action of proteasome inhibitors and deacetylase inhibitors and the biological basis of synergy in multiple myeloma. Mol Cancer Ther 2011; 10: 2034–2042.
Badros A, Burger AM, Philip S, Niesvizky R, Kolla SS, Goloubeva O et al. Phase I study of vorinostat in combination with bortezomib for relapsed and refractory multiple myeloma. Clin Cancer Res 2009; 15: 5250–5257.
Harrison SJ, Quach H, Link E, Seymour JF, Ritchie DS, Ruell S et al. A high rate of durable responses with romidepsin, bortezomib, and dexamethasone in relapsed or refractory multiple myeloma. Blood 2011; 118: 6274–6283.
Siegel DS, Dimopoulos MA, Yoon S, Laubach JP, Kaufman JL, Goldschmidt H et al. Vantage 095: vorinostat in combination with bortezomib in salvage multiple myeloma patients: final study results of a global phase 2b trial. Blood 2011; 118, (abstract 480).
San-Miguel JF, de Moraes Hungria VT, Yoon S, Wiktor-Jedrzejczak W, Elghandour A, Siritanaratkul N et al. Update on a phase III study of panobinostat with bortezomib and dexamethasone in patients with relapsed multiple myeloma: PANORAMA 1. Blood 2011; 118, (abstract 3976).
Dimopoulos MA, Jagannath S, Yoon S, Siegel DS, Lonial S, Hajek R et al. Vantage 088: vorinostat in combination with bortezomib in patients with relapsed/refractory multiple myeloma: results of a global, randomized phase 3 trial. Blood 2011; 118, (abstract 811).
Olsen EA, Kim YH, Kuzel TM, Pacheco TR, Foss FM, Parker S et al. Phase IIb multicenter trial of vorinostat in patients with persistent, progressive, or treatment refractory cutaneous T-cell lymphoma. J Clin Oncol 2007; 25: 3109–3115.
Piekarz RL, Frye R, Prince HM, Kirschbaum MH, Zain J, Allen SL et al. Phase 2 trial of romidepsin in patients with peripheral T-cell lymphoma. Blood 2011; 117: 5827–5834.
Piekarz RL, Frye R, Turner M, Wright JJ, Allen SL, Kirschbaum MH et al. Phase II multi-institutional trial of the histone deacetylase inhibitor romidepsin as monotherapy for patients with cutaneous T-cell lymphoma. J Clin Oncol 2009; 27: 5410–5417.
Kirschbaum M, Frankel P, Popplewell L, Zain J, Delioukina M, Pullarkat V et al. Phase II study of vorinostat for treatment of relapsed or refractory indolent non-Hodgkin's lymphoma and mantle cell lymphoma. J Clin Oncol 2011; 29: 1198–1203.
Acknowledgements
Oliver G Ottmann is an endowed professor of the German Jose Carreras Leukemia Foundation. Financial support for this study was provided by Novartis Pharmaceuticals. We thank William Fazzone, PhD, for medical editorial assistance with this manuscript and Tracy Liu, Hannah Mosca and Glen Laird for assistance with data collection and analysis.
Author contributions
PA, KB, DJD, TF, FJG, AL, OGO, HMP and JWS designed research; PA, KB, DJD, TF, FJG, TK, OGO, HMP, AS and MW performed research; PA contributed new analytical tools; KB, DJD, TF, FJG, TK, OGO, HMP and AS collected data; and KM performed statistical analyses. All authors analyzed and interpreted the data and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
TK: nothing to disclose; KB: Novartis research funding and honoraria; DJD: Novartis consultancy; TF: Novartis honoraria; FJG: Novartis consultancy and research funding; OGO: Novartis consultancy, research funding, honoraria and advisory committee; HMP: Novartis research funding, honoraria, speakers bureau and advisory committee; AS: Novartis research funding, honoraria and speakers bureau; PA, AL, KM, KP, JWS and MW: Novartis employment; and MW: Novartis equity ownership.
Additional information
Supplementary Information accompanies this paper on the Leukemia website
Supplementary information
Rights and permissions
About this article
Cite this article
DeAngelo, D., Spencer, A., Bhalla, K. et al. Phase Ia/II, two-arm, open-label, dose-escalation study of oral panobinostat administered via two dosing schedules in patients with advanced hematologic malignancies. Leukemia 27, 1628–1636 (2013). https://doi.org/10.1038/leu.2013.38
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/leu.2013.38
Keywords
This article is cited by
-
Post-transplant maintenance therapy in acute myeloid leukemia after allogeneic hematopoietic stem cell transplantation harmonizing multiple therapeutic modalities including targeted therapy, immunotherapy and cellular therapy
International Journal of Hematology (2023)
-
PDI inhibitor LTI6426 enhances panobinostat efficacy in preclinical models of multiple myeloma
Cancer Chemotherapy and Pharmacology (2022)
-
Panobinostat (LBH589) increase survival in adult xenografic model of acute lymphoblastic leukemia with t(4;11) but promotes antagonistic effects in combination with MTX and 6MP
Medical Oncology (2022)
-
Maintenance therapy in acute myeloid leukemia after allogeneic hematopoietic stem cell transplantation
Journal of Hematology & Oncology (2021)
-
Is more better? An analysis of toxicity and response outcomes from dose-finding clinical trials in cancer
BMC Cancer (2021)