Abstract
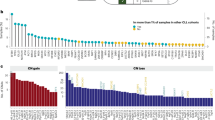
Genetic lesions are crucial for cancer initiation. Recently, whole genome sequencing, using next generation technology, was used as a systematic approach to identify mutations in genomes of various types of tumors including melanoma, lung and breast cancer, as well as acute myeloid leukemia (AML). Here, we identify tumor-specific somatic mutations by sequencing transcriptionally active genes. Mutations were detected by comparing the transcriptome sequence of an AML sample with the corresponding remission sample. Using this approach, we found five non-synonymous mutations specific to the tumor sample. They include a nonsense mutation affecting the RUNX1 gene, which is a known mutational target in AML, and a missense mutation in the putative tumor suppressor gene TLE4, which encodes a RUNX1 interacting protein. Another missense mutation was identified in SHKBP1, which acts downstream of FLT3, a receptor tyrosine kinase mutated in about 30% of AML cases. The frequency of mutations in TLE4 and SHKBP1 in 95 cytogenetically normal AML patients was 2%. Our study demonstrates that whole transcriptome sequencing leads to the rapid detection of recurring point mutations in the coding regions of genes relevant to malignant transformation.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Mrozek K, Marcucci G, Paschka P, Whitman SP, Bloomfield CD . Clinical relevance of mutations and gene-expression changes in adult acute myeloid leukemia with normal cytogenetics: are we ready for a prognostically prioritized molecular classification? Blood 2007; 109: 431–448.
Yamamoto Y, Kiyoi H, Nakano Y, Suzuki R, Kodera Y, Miyawaki S et al. Activating mutation of D835 within the activation loop of FLT3 in human hematologic malignancies. Blood 2001; 97: 2434–2439.
Nakao M, Yokota S, Iwai T, Kaneko H, Horiike S, Kashima K et al. Internal tandem duplication of the flt3 gene found in acute myeloid leukemia. Leukemia 1996; 10: 1911–1918.
Reindl C, Bagrintseva K, Vempati S, Schnittger S, Ellwart JW, Wenig K et al. Point mutations in the juxtamembrane domain of FLT3 define a new class of activating mutations in AML. Blood 2006; 107: 3700–3707.
Pabst T, Mueller BU, Zhang P, Radomska HS, Narravula S, Schnittger S et al. Dominant-negative mutations of CEBPA, encoding CCAAT/enhancer binding protein-alpha (C/EBP alpha), in acute myeloid leukemia. Nat Genet 2001; 27: 263–270.
Yu M, Honoki K, Andersen J, Paietta E, Nam DK, Yunis JJ . MLL tandem duplication and multiple splicing in adult acute myeloid leukemia with normal karyotype. Leukemia 1996; 10: 774–780.
Falini B, Mecucci C, Tiacci E, Alcalay M, Rosati R, Pasqualucci L et al. Cytoplasmic nucleophosmin in acute myelogenous leukemia with a normal karyotype. N Engl J Med 2005; 352: 254–266.
Zhang DE, Zhang P, Wang ND, Hetherington CJ, Darlington GJ, Tenen DG . Absence of granulocyte colony-stimulating factor signaling and neutrophil development in CCAAT enhancer binding protein alpha-deficient mice. Proc Natl Acad Sci USA 1997; 94: 569–574.
Caligiuri MA, Schichman SA, Strout MP, Mrozek K, Baer MR, Frankel SR et al. Molecular rearrangement of the ALL-1 gene in acute myeloid leukemia without cytogenetic evidence of 11q23 chromosomal translocations. Cancer Res 1994; 54: 370–373.
Ley TJ, Mardis ER, Ding L, Fulton B, McLellan MD, Chen K et al. DNA sequencing of a cytogenetically normal acute myeloid leukaemia genome. Nature 2008; 456: 66–72.
Mardis ER, Ding L, Dooling DJ, Larson DE, McLellan MD, Chen K et al. Recurring mutations found by sequencing an acute myeloid leukemia genome. N Engl J Med 2009; 361: 1058–1066.
Pleasance ED, Cheetham RK, Stephens PJ, McBride DJ, Humphray SJ, Greenman CD et al. A comprehensive catalogue of somatic mutations from a human cancer genome. Nature 2010; 463: 191–196.
Pleasance ED, Stephens PJ, O’Meara S, McBride DJ, Meynert A, Jones D et al. A small-cell lung cancer genome with complex signatures of tobacco exposure. Nature 2010; 463: 184–190.
Stephens PJ, McBride DJ, Lin ML, Varela I, Pleasance ED, Simpson JT et al. Complex landscapes of somatic rearrangement in human breast cancer genomes. Nature 2009; 462: 1005–1010.
Stratton MR, Campbell PJ, Futreal PA . The cancer genome. Nature 2009; 458: 719–724.
Gross S, Cairns RA, Minden MD, Driggers EM, Bittinger MA, Jang HG et al. Cancer-associated metabolite 2-hydroxyglutarate accumulates in acute myelogenous leukemia with isocitrate dehydrogenase 1 and 2 mutations. J Exp Med 2010; 207: 339–344.
Hurowitz EH, Drori I, Stodden VC, Donoho DL, Brown PO . Virtual Northern analysis of the human genome. PLoS ONE 2007; 2: e460.
Velculescu VE, Madden SL, Zhang L, Lash AE, Yu J, Rago C et al. Analysis of human transcriptomes. Nat Genet 1999; 23: 387–388.
Li H, Durbin R . Fast and accurate short read alignment with Burrows-Wheeler transform. Bioinformatics 2009; 25: 1754–1760.
Li H, Handsaker B, Wysoker A, Fennell T, Ruan J, Homer N et al. The Sequence Alignment/Map format and SAMtools. Bioinformatics 2009; 25: 2078–2079.
Mortazavi A, Williams BA, McCue K, Schaeffer L, Wold B . Mapping and quantifying mammalian transcriptomes by RNA-Seq. Nat Methods 2008; 5: 621–628.
Li H, Ruan J, Durbin R . Mapping short DNA sequencing reads and calling variants using mapping quality scores. Genome Res 2008; 18: 1851–1858.
Ng SB, Buckingham KJ, Lee C, Bigham AW, Tabor HK, Dent KM et al. Exome sequencing identifies the cause of a Mendelian disorder. Nat Genet 2010; 42: 30–35.
Peterson LF, Zhang DE . The 8;21 translocation in leukemogenesis. Oncogene 2004; 23: 4255–4262.
Osato M . Point mutations in the RUNX1/AML1 gene: another actor in RUNX leukemia. Oncogene 2004; 23: 4284–4296.
Dayyani F, Wang J, Yeh JR, Ahn EY, Tobey E, Zhang DE et al. Loss of TLE1 and TLE4 from the del(9q) commonly deleted region in AML cooperates with AML1-ETO to affect myeloid cell proliferation and survival. Blood 2008; 111: 4338–4347.
Borinstein SC, Hyatt MA, Sykes VW, Straub RE, Lipkowitz S, Boulter J et al. SETA is a multifunctional adapter protein with three SH3 domains that binds Grb2, Cbl, and the novel SB1 proteins. Cell Signal 2000; 12: 769–779.
Reindl C, Quentmeier H, Petropoulos K, Greif PA, Benthaus T, Argiropoulos B et al. CBL exon 8/9 mutants activate the FLT3 pathway and cluster in core binding factor/11q deletion acute myeloid leukemia/myelodysplastic syndrome subtypes. Clin Cancer Res 2009; 15: 2238–2247.
Liu JP, Liu NS, Yuan HY, Guo Q, Lu H, Li YY . Human homologue of SETA binding protein 1 interacts with cathepsin B and participates in TNF-Induced apoptosis in ovarian cancer cells. Mol Cell Biochem 2006; 292: 189–195.
Mayr C, Bartel DP . Widespread shortening of 3′UTRs by alternative cleavage and polyadenylation activates oncogenes in cancer cells. Cell 2009; 138: 673–684.
Acknowledgements
This work was funded by a Deutsche Krebshilfe grant 109031 to PA Greif and SK Bohlander, and by grants from the German Ministry of Research and Education (BMBF; 01GS0876) and the Deutsche Forschungsgemeinschaft (SFB 684-A6) to SK Bohlander.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Leukemia website
Supplementary information
Rights and permissions
About this article
Cite this article
Greif, P., Eck, S., Konstandin, N. et al. Identification of recurring tumor-specific somatic mutations in acute myeloid leukemia by transcriptome sequencing. Leukemia 25, 821–827 (2011). https://doi.org/10.1038/leu.2011.19
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/leu.2011.19
Keywords
This article is cited by
-
Calpain activity is negatively regulated by a KCTD7–Cullin-3 complex via non-degradative ubiquitination
Cell Discovery (2023)
-
Erythrocytosis with JAK2 GGCC_46/1 haplotype and without JAK2 V617F mutation is associated with CALR rs1049481_G allele
Leukemia (2021)
-
KCTD15 is overexpressed in human childhood B-cell acute lymphoid leukemia
Scientific Reports (2019)
-
Leukemia-propagating cells demonstrate distinctive gene expression profiles compared with other cell fractions from patients with de novo Philadelphia chromosome-positive ALL
Annals of Hematology (2018)
-
Understanding of leukemic stem cells and their clinical implications
Molecular Cancer (2017)