Abstract
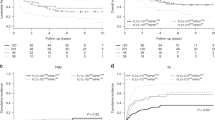
Natural killer (NK) cells are expanded in chronic myeloid leukemia (CML) patients on tyrosine kinase inhibitors (TKI) and exert cytotoxicity. The inherited repertoire of killer immunoglobulin-like receptors (KIR) may influence response to TKI. We investigated the impact of KIR-genotype on outcome in 166 chronic phase CML patients on first-line imatinib treatment. We validated our findings in an independent patient group. On multivariate analysis, KIR2DS1 genotype (RR=1.51, P=0.03) and Sokal risk score (low-risk RR=1, intermediate-risk RR=1.53, P=0.04, high-risk RR=1.69, P=0.034) were the only independent predictors for failure to achieve complete cytogenetic response (CCyR). Furthermore, KIR2DS1 was the only factor predicting shorter progression-free (PFS) (RR=3.1, P=0.03) and overall survival (OS) (RR=2.6, P=0.04). The association between KIR2DS1 and CCyR, PFS and OS was validated by KIR genotyping in 174 CML patients on first-line imatinib in the UK multi-center SPIRIT-1 trial; in this cohort, KIR2DS1(+) patients had significantly lower 2-year probabilities of achieving CCyR (76.9 vs 87.9%, P=0.003), PFS (85.3 vs 98.1%, P=0.007) and OS (94.4 vs 100%, P=0.015) than KIR2DS1(−) patients. The impact of KIR2DS1 on CCyR was greatest when the ligand for the corresponding inhibitory receptor, KIR2DL1, was absent (P=0.00006). Our data suggest a novel role for KIR-HLA immunogenetics in CML patients on TKI.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Druker BJ, Guilhot F, O’Brien SG, Gathmann I, Kantarjian H, Deininger MW et al. Five-year follow-up of patients receiving imatinib for chronic myeloid leukemia. N Engl J Med 2006; 355: 2408–2417.
Hughes TP, Kaeda J, Branford S, Rudzki Z, Hochhaus A, Hensley ML et al. Frequency of major molecular responses to imatinib or interferon alfa plus cytarabine in newly diagnosed chronic myeloid leukemia. N Engl J Med 2003; 349: 1423–1432.
Kolb HJ, Schmid C, Barrett AJ, Schendel DJ . Graft-versus-leukemia reactions in allogeneic chimeras. Blood 2004; 103: 767–776.
Caligiuri MA . Human natural killer cells. Blood 2008; 112: 461–469.
Lanier LL . NK cell recognition. Annu Rev Immunol 2005; 23: 225–274.
Vivier E, Nunes JA, Vely F . Natural killer cell signaling pathways. Science 2004; 306: 1517–1519.
Clausen J, Wolf D, Petzer AL, Gunsilius E, Schumacher P, Kircher B et al. Impact of natural killer cell dose and donor killer-cell immunoglobulin-like receptor (KIR) genotype on outcome following human leucocyte antigen-identical haematopoietic stem cell transplantation. Clin Exp Immunol 2007; 148: 520–528.
Cooley S, Trachtenberg E, Bergemann TL, Saeteurn K, Klein J, Chap T et al. Donors with group B KIR haplotypes improve relapse-free survival after unrelated hematopoietic cell transplantation for acute myelogenous leukemia. Blood 2009; 113: 726–732.
Kroger N, Binder T, Zabelina T, Wolschke C, Schieder H, Renges H et al. Low number of donor activating killer immunoglobulin-like receptors (KIR) genes but not KIR-ligand mismatch prevents relapse and improves disease-free survival in leukemia patients after in vivo T-cell depleted unrelated stem cell transplantation. Transplantation 2006; 82: 1024–1030.
Ruggeri L, Capanni M, Urbani E, Perruccio K, Shlomchik WD, Tosti A et al. Effectiveness of donor natural killer cell alloreactivity in mismatched hematopoietic transplants. Science 2002; 295: 2097–2100.
Sconocchia G, Lau M, Provenzano M, Rezvani K, Wongsena W, Fujiwara H et al. The antileukemia effect of HLA-matched NK and NK-T cells in chronic myelogenous leukemia involves NKG2D-target-cell interactions. Blood 2005; 106: 3666–3672.
Yong AS, Keyvanfar K, Hensel N, Eniafe R, Savani BN, Berg M et al. Primitive quiescent CD34+ cells in chronic myeloid leukemia are targeted by in vitro expanded natural killer cells, which are functionally enhanced by bortezomib. Blood 2009; 113: 875–882.
Kreutzman A, Juvonen V, Kairisto V, Ekblom M, Stenke L, Seggewiss R et al. Mono/oligoclonal T and NK cells are common in chronic myeloid leukemia patients at diagnosis and expand during dasatinib therapy. Blood 2010; 116: 772–782.
Borg C, Terme M, Taieb J, Menard C, Flament C, Robert C et al. Novel mode of action of c-kit tyrosine kinase inhibitors leading to NK cell-dependent antitumor effects. J Clin Invest 2004; 114: 379–388.
Cebo C, Da RS, Wittnebel S, Turhan AG, Abdelali J, Caillat-Zucman S et al. The decreased susceptibility of Bcr/Abl targets to NK cell-mediated lysis in response to imatinib mesylate involves modulation of NKG2D ligands, GM1 expression, and synapse formation. J Immunol 2006; 176: 864–872.
Kantarjian HM, Talpaz M . Definition of the accelerated phase of chronic myelogenous leukemia. J Clin Oncol 1988; 6: 180–182.
O’Brien SG, Deininger MW . Imatinib in patients with newly diagnosed chronic-phase chronic myeloid leukemia. Semin Hematol 2003; 40: 26–30.
Druker BJ, Guilhot F, O’Brien SG, Gathmann I, Kantarjian H, Deininger MW et al. Five-year follow-up of patients receiving imatinib for chronic myeloid leukemia. N Engl J Med 2006; 355: 2408–2417.
O’Brien SG, Deininger MW . Imatinib in patients with newly diagnosed chronic-phase chronic myeloid leukemia. Semin Hematol 2003; 40: 26–30.
National Institutes of Health National Cancer Institute. Cancer Therapy Evaluation Program: Common Toxicity Criteria. National Institutes of Health National Cancer Institute: Bethesda, MD, 1998.
Baccarani M, Castagnetti F, Gugliotta G, Palandri F, Soverini S . Response definitions and European Leukemianet Management recommendations. Best Pract Res Clin Haematol 2009; 22: 331–341.
Kantarjian HM, Talpaz M . Definition of the accelerated phase of chronic myelogenous leukemia. J Clin Oncol 1988; 6: 180–182.
Velickovic M, Velickovic Z, Dunckley H . Diversity of killer cell immunoglobulin-like receptor genes in Pacific Islands populations. Immunogenetics 2006; 58: 523–532.
Hsu KC, Chida S, Geraghty DE, Dupont B . The killer cell immunoglobulin-like receptor (KIR) genomic region: gene-order, haplotypes and allelic polymorphism. Immunol Rev 2002; 190: 40–52.
Single RM, Martin MP, Meyer D, Gao X, Carrington M . Methods for assessing gene content diversity of KIR with examples from a global set of populations. Immunogenetics 2008; 60: 711–725.
Sokal JE, Cox EB, Baccarani M, Tura S, Gomez GA, Robertson JE et al. Prognostic discrimination in “good-risk” chronic granulocytic leukemia. Blood 1984; 63: 789–799.
de Lavallade H, Apperley JF, Khorashad JS, Milojkovic D, Reid A, Bua M et al. Imatinib for newly diagnosed patients with chronic myeloid leukemia: incidence of sustained responses in an intention-to-treat analysis. J Clin Oncol 2008; 26: 3358–3363.
Grzywacz B, Miller JS, Verneris MR . Use of natural killer cells as immunotherapy for leukaemia. Best. Pract Res Clin Haematol 2008; 21: 467–483.
Sconocchia G, Lau M, Provenzano M, Rezvani K, Wingsena W, Fujiwara H et al. The antileukemia effect of HLA-matched NK and NK-T cells in chronic myelogenous leukemia involves NKG2D-target-cell interactions. Blood 2005; 106: 3666–3672.
Clausen J, Wolf D, Petzer AL, Gunsilius E, Schumacher P, Kircher B et al. Impact of natural killer cell dose and donor killer-cell immunoglobulin-like receptor (KIR) genotype on outcome following human leucocyte antigen-identical haematopoietic stem cell transplantation. Clin Exp Immunol 2007; 148: 520–528.
Giebel S, Locatelli F, Lamparelli T, Velardi, Davies S, Frumento G et al. Survival advantage with KIR ligand incompatibility in hematopoietic stem cell transplantation from unrelated donors. Blood 2003; 102: 814–819.
Miller JS, Cooley S, Parham P, Farag SS, Verneris MR, Mc Queen KL et al. Missing KIR ligands are associated with less relapse and increased graft-versus-host disease (GVHD) following unrelated donor allogeneic HCT. Blood 2007; 109: 5058–5061.
Ruggeri L, Capanni M, Urbani E, Perruccio, Shlomick WD, Tosti A et al. Effectiveness of donor natural killer cell alloreactivity in mismatched hematopoietic transplants. Science 2002; 295: 2097–2100.
Gabriel IH, Sergeant R, Szydlo R, Apperley JF, DeLavallade H, Alsuliman A et al. Interaction between KIR3DS1 and HLA-Bw4 predicts for progression-free survival following autologous stem cell transplantation in patients with multiple myeloma. Blood 2010; 116: 2033–2039.
Hsu KC, Chida S, Geraghty DE, Dupont B . The killer cell immunoglobulin-like receptor (KIR) genomic region: gene-order, haplotypes and allelic polymorphism. Immunol Rev 2002; 190: 40–52.
Single RM, Martin MP, Meyer D, Gao X, Carrington M . Methods for assessing gene content diversity of KIR with examples from a global set of populations. Immunogenetics 2008; 60: 711–725.
Martin MP, Nelson G, Lee JH, Pellett F, Gao X, Wade J et al. Cutting edge: susceptibility to psoriatic arthritis: influence of activating killer Ig-like receptor genes in the absence of specific HLA-C alleles. J Immunol 2002; 169: 2818–2822.
Stewart CA, Laugier-Anfossi F, Vely F, Saulquin X, Riedmuller J, Tisserant A et al. Recognition of peptide-MHC class I complexes by activating killer immunoglobulin-like receptors. Proc Natl Acad Sci USA 2005; 102: 13224–13229.
Biassoni R, Pessino A, Malaspina A, Cantoni, Bottino C, Sivori S et al. Role of amino acid position 70 in the binding affinity of p50.1 and p58.1 receptors for HLA-Cw4 molecules. Eur J Immunol 1997; 27: 3095–3099.
Arase H, Mocarski ES, Campbell AE, Hill AB, Lanier LL . Direct recognition of cytomegalovirus by activating and inhibitory NK cell receptors. Science 2002; 296: 1323–1326.
Daniels KA, Devora G, Lai WC, O’Donnell CL, Bennett M, Welsh RM . Murine cytomegalovirus is regulated by a discrete subset of natural killer cells reactive with monoclonal antibody to Ly49 h. J Exp Med 2001; 194: 29–44.
Smith HRC, Heusel JW, Mehta IK, Kim S, Dorner BG, Naidenko OV et al. Recognition of a virus-encoded ligand by a natural killer cell activation receptor. Proc Natl Acad Sci USA 2002; 99: 8826–8831.
Vivier E, Biron CA . A pathogen receptor on natural killer cells. Science 2002; 296: 1248–1249.
Sconocchia G, Lau M, Provenzano M, Rezvani K, Wonsenga W, Fujiwara H et al. The antileukemia effect of HLA-matched NK and NK-T cells in chronic myelogenous leukemia involves NKG2D-target-cell interactions. Blood 2005; 106: 3666–3672.
Yong AS, Keyvanfar K, Hensel N, Enaife R, Savani BN, Berg M et al. Primitive quiescent CD34+ cells in chronic myeloid leukemia are targeted by in vitro expanded natural killer cells, which are functionally enhanced by bortezomib. Blood 2009; 113: 875–882.
Borg C, Terme M, Taieb J, Menard C, Flament C, Robert C et al. Novel mode of action of c-kit tyrosine kinase inhibitors leading to NK cell-dependent antitumor effects. J Clin Invest 2004; 114: 379–388.
Salih J, Hilpert J, Placke T, Grunebach F, Steinle A, Salih HR et al. The BCR/ABL-inhibitors imatinib, nilotinib and dasatinib differentially affect NK cell reactivity. Int J Cancer 2010; 127: 2119–2128.
Mustjoki S, Ekblom M, Arstila TP, Dybedal L, Epling-Burnette PK, Guihot F et al. Clonal expansion of T/NK-cells during tyrosine kinase inhibitor dasatinib therapy. Leukemia 2009; 23: 1398–1405.
Ghio M, Contini P, Negrini S Mazzei C, Zocchi MR, Poggi A . Soluble HLA-I-mediated secretion of TGF-beta1 by human NK cells and consequent down-regulation of anti-tumor cytolytic activity. Eur J Immunol 2009; 39: 3459–3468.
Nakamura K, Kitani A, Strober W . Cell contact-dependent immunosuppression by CD4(+)CD25(+) regulatory T cells is mediated by cell surface-bound transforming growth factor beta. J Exp Med 2001; 194: 629–644.
Naka K, Hoshii T, Muraguchi T, Tadokoro, Ooshio T, Kondo Y et al. TGF-beta-FOXO signalling maintains leukaemia-initiating cells in chronic myeloid leukaemia. Nature 2010; 463: 676–680.
Acknowledgements
We would like to acknowledge the participating centers in the SPIRIT 1 trial, the SPIRIT study Team especially Caroline Hodgson, Claire Oyston, Lynn Seeley, Wendy Banks, Meg Buckley and the support of the NCRN CML working group, United Kingdom. We acknowledge the support of the National Institute for Health Research (NIHR) Biomedical Research Center (BRC), United Kingdom. This work was supported by the NIHR BRC London, (grant no. P31514) and Leuka registered charity, 286231.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Marin, D., Gabriel, I., Ahmad, S. et al. KIR2DS1 genotype predicts for complete cytogenetic response and survival in newly diagnosed chronic myeloid leukemia patients treated with imatinib. Leukemia 26, 296–302 (2012). https://doi.org/10.1038/leu.2011.180
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/leu.2011.180
Keywords
This article is cited by
-
European LeukemiaNet laboratory recommendations for the diagnosis and management of chronic myeloid leukemia
Leukemia (2023)
-
Four novel candidate causal variants for deficient homozygous haplotypes in Holstein cattle
Scientific Reports (2022)
-
The proportion of different BCR-ABL1 transcript types in chronic myeloid leukemia. An international overview
Leukemia (2019)
-
Peptide-specific engagement of the activating NK cell receptor KIR2DS1
Scientific Reports (2017)
-
The favorable role of homozygosity for killer immunoglobulin-like receptor (KIR) A haplotype in patients with advanced-stage classic Hodgkin lymphoma
Journal of Hematology & Oncology (2016)