Abstract
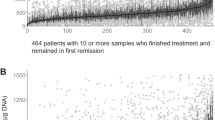
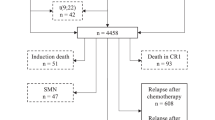
Drug doses, blood levels of drug metabolites and myelotoxicity during 6-mercaptopurine/methotrexate (MTX) maintenance therapy were registered for 59 adolescents (⩾10 years) and 176 non-adolescents (<10 years) with B-cell precursor acute lymphoblastic leukemia (ALL) and a white blood cell count (WBC) <50 × 109/l at diagnosis. Event-free survival was lower for adolescents than non-adolescents (pEFS12y:0.71 vs 0.83, P=0.04). For adolescents staying in remission, the mean WBC during maintenance therapy (mWBC) was related to age (rS=0.36, P=0.02), which became nonsignificant for those who relapsed (rS=0.05, P=0.9). The best-fit multivariate Cox regression model to predict risk of relapse included mWBC and thiopurine methyltransferase activity, which methylates mercaptopurine and reduces the intracellular availability of cytotoxic 6-thioguanine nucleotides (coefficient: 0.11, P=0.02). The correlation of mWBC to the risk of relapse was more pronounced for adolescents (coefficient=0.65, P=0.003) than for non-adolescents (coefficient=0.42, P=0.04). Adolescents had higher mean neutrophil counts (P=0.002) than non-adolescents, but received nonsignificantly lower mercaptopurine and MTX doses during maintenance therapy. Red blood cell MTX levels were significantly related to the dose of MTX among adolescents who stayed in remission (rS=0.38, P=0.02), which was not the case for those who developed a relapse (rS=0.15, P=0.60). Thus, compliance to maintenance therapy may influence the risk of relapse for adolescents with ALL.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Gustafsson G, Schmiegelow K, Forestier E, Clausen N, Glomstein A, Jonmundsson G et al. Improving outcome through two decades in childhood ALL in the Nordic countries: the impact of high-dose methotrexate in the reduction of CNS irradiation. Nordic Society of Pediatric Haematology and Oncology (NOPHO). Leukemia 2000; 14: 2267–2275.
Smith M, Arthur D, Camitta B, Carroll AJ, Crist W, Gaynon P et al. Uniform approach to risk classification and treatment assignment for children with acute lymphoblastic leukemia [see comments]. J Clin Oncol 1996; 14: 18–24.
Pui CH, Robison LL, Look AT . Acute lymphoblastic leukaemia. Lancet 2008; 371: 1030–1043.
Barry E, DeAngelo DJ, Neuberg D, Stevenson K, Loh ML, Asselin BL et al. Favorable outcome for adolescents with acute lymphoblastic leukemia treated on Dana-Farber Cancer Institute Acute Lymphoblastic Leukemia Consortium Protocols. J Clin Oncol 2007; 25: 813–819.
Hjalgrim LL, Rostgaard K, Schmiegelow K, Soderhall S, Kolmannskog S, Vettenranta K et al. Age- and sex-specific incidence of childhood leukemia by immunophenotype in the Nordic countries. J Natl Cancer Inst 2003; 95: 1539–1544.
Forestier E, Schmiegelow K . The incidence peaks of the childhood acute leukemias reflect specific cytogenetic aberrations. J Pediatr Hematol Oncol 2006; 28: 486–495.
Harrison CJ . Cytogenetics of paediatric and adolescent acute lymphoblastic leukaemia. Br J Haematol 2009; 144: 147–156.
Schmiegelow K, Bjork O, Glomstein A, Gustafsson G, Keiding N, Kristinsson J et al. Intensification of mercaptopurine/methotrexate maintenance chemotherapy may increase the risk of relapse for some children with acute lymphoblastic leukemia. J Clin Oncol 2003; 21: 1332–1339.
Schmiegelow K, Heyman M, Kristinsson J, Mogensen UB, Rosthoj S, Vettenranta K et al. Oral Methotrexate/6-Mercaptopurine may be superior to a multi-drug LSA2L2 maintenance therapy for higher risk childhood acute lymphoblastic leukemia. J Pediatr Hematol Oncol 2009; 31: 385–392.
Forestier E, Heyman M, Andersen MK, Autio K, Blennow E, Borgstrom G et al. Outcome of ETV6/RUNX1-positive childhood acute lymphoblastic leukaemia in the NOPHO-ALL-1992 protocol: frequent late relapses but good overall survival. Br J Haematol 2008; 140: 665–672.
Mitelman F . An International System for Human Cytogenetic Nomenclature. S Karger AG: Basel, Switzerland, 1995, 1–114.
Skarby TV, Anderson H, Heldrup J, Kanerva JA, Seidel H, Schmiegelow K . High leucovorin doses during high-dose methotrexate treatment may reduce the cure rate in childhood acute lymphoblastic leukemia. Leukemia 2006; 20: 1955–1962.
Bruunshuus I, Schmiegelow K . Analysis of 6-mercaptopurine, 6-thioguanine nucleotides, and 6-thiouric acid in biological fluids by high-performance liquid chromatography. Scand J Clin Lab Invest 1989; 49: 779–784.
Kamen BA, Takach PL, Vatev R, Caston JD . A rapid, radiochemical-ligand binding assay for methotrexate. Anal Biochem 1976; 70: 54–63.
Wang L, Weinshilboum R . Thiopurine S-methyltransferase pharmacogenetics: insights, challenges and future directions. Oncogene 2006; 25: 1629–1638.
Schmiegelow K, Forestier E, Kristinsson J, Soderhall S, Vettenranta K, Weinshilboum R et al. Thiopurine methyltransferase activity is related to the risk of relapse of childhood acute lymphoblastic leukemia: results from the NOPHO ALL-92 study. Leukemia 2009; 3: 557–564.
Weinshilboum RM, Raymond FA, Pazmino PA . Human erythrocyte thiopurine methyltransferase: radiochemical microassay and biochemical properties. Clin Chim Acta 1978; 85: 323–333.
Siegel S, Castellan NJ . Nonparametric Statistics for the Behavioral Sciences. 2nd ed. McGraw-Hill Publishing Co.: Singapore, 1988, 1–330.
Cox DR . Regression models and life-tables (with discussion). J R Stat Soc (B) 1972; 34: 187–220.
Andersen PK, Borgan Ø, Gill RD, Keiding N . Statistical Models Based on Counting Processes. Springer-Verlag: New York, 1993, 1–767.
Schmiegelow K, Pulczynska MK . Maintenance chemotherapy for childhood acute lymphoblastic leukemia: should dosage be guided by white blood cell counts? Am J Pediatr Hematol Oncol 1990; 12: 462–467.
Kaplan EJ, Meier P . Non-parametric estimation from incomplete observations. J Am Stat Assoc 1958; 53: 457–481.
Mantel N . Evaluation of survival data and two new rank order statistics arising in its consideration. Cancer Chemother 1966; 50: 163–170.
Schmiegelow K, Al-Modhwahi I, Andersen MK, Behrendtz M, Forestier E, Hasle H et al. Methotrexate/6-mercaptopurine maintenance therapy influences the risk of a second malignant neoplasm after childhood acute lymphoblastic leukemia - results from the NOPHO ALL-92 study. Blood 2009; 113: 6077–6084.
Schroder H, Clausen N, Ostergaard E, Pressler T . Pharmacokinetics of erythrocyte methotrexate in children with acute lymphoblastic leukemia during maintenance treatment. Cancer Chemother Pharmacol 1986; 16: 190–193.
Arico M, Baruchel A, Bertrand Y, Biondi A, Conter V, Eden T et al. The seventh international childhood acute lymphoblastic leukemia workshop report: Palermo, Italy, January 29–30, 2005. Leukemia 2005; 19: 1145–1152.
Schmiegelow K, Pulczynska MK . White-cell counts in childhood acute lymphoblastic leukemia. Eur J Haematol 1990; 44: 72–74.
Schmiegelow K, Pulczynska MK . Maintenance chemotherapy for childhood acute lymphoblastic leukemia: should dosage be guided by white blood cell counts? Am J Pediatr Hematol Oncol 1990; 12: 462–467.
Hayder S, Bjork O, Nilsson B . Relapse factors during maintenance therapy of acute lymphoblastic leukemia in children. Pediatr Hematol Oncol 1992; 9: 21–27.
Dolan G, Lilleyman JS, Richards SM . Prognostic importance of myelosuppression during maintenance treatment of lymphoblastic leukaemia. Leukaemia in Childhood Working Party of the Medical Research Council. Arch Dis Child 1989; 64: 1231–1234.
Relling MV, Hancock ML, Boyett JM, Pui CH, Evans WE . Prognostic importance of 6-mercaptopurine dose intensity in acute lymphoblastic leukemia. Blood 1999; 93: 2817–2823.
Gobrecht O, Gobel U, Graubner U, Gutjahr P, Schock V, Spaar HJ et al. Effect of dose intensity and therapy-induced leukocytopenia in intensive therapy on the prognosis of acute lymphatic leukemia in childhood. Results in 213 patients of the COALL-85 study. Klin Padiatr 1992; 204: 230–235.
Lucas K, Gula MJ, Blatt J . Relapse in acute lymphoblastic leukemia as a function of white blood cell and absolute neutrophil counts during maintenance chemotherapy. Pediatr Hematol Oncol 1992; 9: 91–97.
Schmiegelow K . Prognostic significance of methotrexate and 6-mercaptopurine dosage during maintenance chemotherapy for childhood acute lymphoblastic leukemia. Pediatr Hematol Oncol 1991; 8: 301–312.
Peeters M, Koren G, Jakubovicz D, Zipursky A . Physician compliance and relapse rates of acute lymphoblastic leukemia in children. Clin Pharmacol Ther 1988; 43: 228–232.
Bohnstedt C, Taskinen M, Zeller B, Bjorgvinsdottir H, Hafsteinsdottir S, Schmiegelow K . Poor treatment compliance in children with Down syndrome and acute lymphoblastic leukemia. J Pediatr Hematol Oncol 2009; 31: 79–80.
Schmiegelow K, Ifversen M . Myelotoxicity, pharmacokinetics, and relapse rate with methotrexate/6-mercaptopurine maintenance therapy of childhood acute lymphoblastic leukemia. Pediatr Hematol Oncol 1996; 13: 433–441.
Schmiegelow K, Pulczynska MK . White-cell counts in childhood acute lymphoblastic leukemia. Eur J Haematol 1990; 44: 72–74.
Kearney SL, Dahlberg SE, Levy DE, Voss SD, Sallan SE, Silverman LB . Clinical course and outcome in children with acute lymphoblastic leukemia and asparaginase-associated pancreatitis. Pediatr Blood Cancer 2009; 53: 162–167.
Lau RC, Matsui D, Greenberg M, Koren G . Electronic measurement of compliance with mercaptopurine in pediatric patients with acute lymphoblastic leukemia. Med Pediatr Oncol 1998; 30: 85–90.
Lancaster D, Lennard L, Lilleyman JS . Profile of non-compliance in lymphoblastic leukaemia. Arch Dis Child 1997; 76: 365–366.
Davies HA, Lilleyman JS . Compliance with oral chemotherapy in childhood lymphoblastic leukaemia. Cancer Treat Rev 1995; 21: 93–103.
Pritchard MT, Butow PN, Stevens MM, Duley JA . Understanding medication adherence in pediatric acute lymphoblastic leukemia: a review. J Pediatr Hematol Oncol 2006; 28: 816–823.
Lancaster D, Lennard L, Lilleyman JS . Profile of non-compliance in lymphoblastic leukaemia. Arch Dis Child 1997; 76: 365–366.
Lancaster D, Lennard L, Lilleyman JS . Profile of non-compliance in lymphoblastic leukaemia. Arch Dis Child 1997; 76: 365–366.
Kearns GL, bdel-Rahman SM, Alander SW, Blowey DL, Leeder JS, Kauffman RE . Developmental pharmacology—drug disposition, action, and therapy in infants and children. N Engl J Med 2003; 349: 1157–1167.
Balis FM, Holcenberg JS, Poplack DG, Ge J, Sather HN, Murphy RF et al. Pharmacokinetics and pharmacodynamics of oral methotrexate and mercaptopurine in children with lower risk acute lymphoblastic leukemia: a joint children's cancer group and pediatric oncology branch study. Blood 1998; 92: 3569–3577.
Borsi JD, Moe PJ . A comparative study on the pharmacokinetics of methotrexate in a dose range of 0.5 g–33.6 g/m2 in children with acute lymphoblastic leukemia. Cancer 1987; 60: 5–13.
Dupuis LL, Koren G, Silverman ED, Laxer RM . Influence of food on the bioavailability of oral methotrexate in children. J Rheumatol 1995; 22: 1570–1573.
Lafolie P, Bjork O, Hayder S, Ahstrom L, Peterson C . Variability of 6-mercaptopurine pharmacokinetics during oral maintenance therapy of children with acute leukemia. Med Oncol Tumor Pharmacother 1989; 6: 259–265.
Lancaster DL, Patel N, Lennard L, Lilleyman JS . 6-Thioguanine in children with acute lymphoblastic leukaemia: influence of food on parent drug pharmacokinetics and 6-thioguanine nucleotide concentrations. Br J Clin Pharmacol 2001; 51: 531–539.
Riccardi R, Balis FM, Ferrara P, Lasorella A, Poplack DG, Mastrangelo R . Influence of food intake on bioavailability of oral 6-mercaptopurine in children with acute lymphoblastic leukemia. Pediatr Hematol Oncol 1986; 3: 319–324.
Calado RT, Yewdell WT, Wilkerson KL, Regal JA, Kajigaya S, Stratakis CA et al. Sex hormones, acting on the TERT gene, increase telomerase activity in human primary hematopoietic cells. Blood 2009; 114: 2236–2243.
Acknowledgements
This study has received financial support from The Danish Childhood Cancer Foundation, The Carl and Ellen Hertz Foundation, The Children's Cancer Foundation of Sweden (grant no.: 53/91, 62/94, 72/96, 98/59), The Danish Cancer Society (grant no.: 91-048, 92-017, 93-017, 95-100-28), The JPC Foundation, The Lundbeck Foundation (grant no.: 38/99), The Minister Erna Hamilton Foundation, The Nordic Cancer Union (grant no.: 56-9257, 56-100-03-9102). Kjeld Schmiegelow holds the Danish Childhood Cancer Foundation Professorship in Pediatric Oncology.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Schmiegelow, K., Heyman, M., Gustafsson, G. et al. The degree of myelosuppression during maintenance therapy of adolescents with B-lineage intermediate risk acute lymphoblastic leukemia predicts risk of relapse. Leukemia 24, 715–720 (2010). https://doi.org/10.1038/leu.2009.303
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/leu.2009.303
Keywords
This article is cited by
-
Results of NOPHO ALL2008 treatment for patients aged 1–45 years with acute lymphoblastic leukemia
Leukemia (2018)
-
Influence of dihydrofolate reductase gene polymorphisms rs408626 (-317A>G) and rs442767 (-680C>A) on the outcome of methotrexate-based maintenance therapy in South Indian patients with acute lymphoblastic leukemia
European Journal of Clinical Pharmacology (2015)
-
Challenges in implementing individualized medicine illustrated by antimetabolite therapy of childhood acute lymphoblastic leukemia
Clinical Proteomics (2011)
-
Optimal therapy for acute lymphoblastic leukemia in adolescents and young adults
Nature Reviews Clinical Oncology (2011)
-
Bone marrow mesenchymal stem cells reduce the antitumor activity of cytokine-induced killer/natural killer cells in K562 NOD/SCID mice
Annals of Hematology (2011)