Abstract
The ALL IC-BFM 2002 protocol was created as an alternative to the MRD-based AIEOP-BFM ALL 2000 study, to integrate early response criteria into risk-group stratification in countries not performing routine PCR-based MRD testing. ALL IC stratification comprises the response to prednisone, bone marrow (BM) morphology at days 15 and 33, age, WBC and BCR/ABL or MLL/AF4 presence. Here, we compared this stratification to the MRD-based criteria using MRD evaluation in 163 patients from four ALL IC member countries at days 8, 15 and 33 and week 12. MRD negativity at day 33 was associated with an age of 1–5 years, WBC<20 000 μl−1, non-T immunophenotype, good prednisone response and non-M3 morphology at day 15. There were no significant associations with gender or hyperdiploidy in the study group, or with TEL/AML1 fusion within BCP-ALL. Patients with M1/2 BM at day 8 tended to be MRD negative at week 12. Patients stratified into the standard-risk group had a better response than intermediate-risk group patients. However, 34% of them were MRD positive at day 33 and/or week 12. Our findings revealed that morphology-based ALL IC risk-group stratification allows the identification of most MRD high-risk patients, but fails to discriminate the MRD low-risk group assigned to therapy reduction.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
References
Cave H, van der Werff ten Bosch J, Suciu S, Guidal C, Waterkeyn C, Otten J et al. Clinical significance of minimal residual disease in childhood acute lymphoblastic leukemia. European Organization for Research and Treatment of Cancer—Childhood Leukemia Cooperative Group. N Engl J Med 1998; 339: 591–598.
Coustan Smith E, Sancho J, Hancock ML, Boyett JM, Behm FG, Raimondi SC et al. Clinical importance of minimal residual disease in childhood acute lymphoblastic leukemia. Blood 2000; 96: 2691–2696.
van Dongen JJ, Seriu T, Panzer-Grumayer ER, Biondi A, Pongers-Willemse MJ, Corral L et al. Prognostic value of minimal residual disease in acute lymphoblastic leukaemia in childhood. Lancet 1998; 352: 1731–1738.
Arico M, Baruchel A, Bertrand Y, Biondi A, Conter V, Eden T et al. The seventh international childhood acute lymphoblastic leukemia workshop report: Palermo, Italy, January 29–30, 2005. Leukemia 2005; 19: 1145–1152.
Pui CH, Relling MV, Sandlund JT, Downing JR, Campana D, Evans WE . Rationale and design of Total Therapy Study XV for newly diagnosed childhood acute lymphoblastic leukemia. Ann Hematol 2004; 83 (Suppl 1): S124–S126.
Schultz KR, Pullen DJ, Sather HN, Shuster JJ, Devidas M, Borowitz MJ et al. Risk- and response-based classification of childhood B-precursor acute lymphoblastic leukemia: a combined analysis of prognostic markers from the Pediatric Oncology Group (POG) and Children's Cancer Group (CCG). Blood 2007; 109: 926–935.
Zhou J, Goldwasser MA, Li A, Dahlberg SE, Neuberg D, Wang H et al. Quantitative analysis of minimal residual disease predicts relapse in children with B-lineage acute lymphoblastic leukemia in DFCI ALL Consortium Protocol 95-01. Blood 2007; 110: 1607–1611.
Stanulla M, Schaeffeler E, Flohr T, Cario G, Schrauder A, Zimmermann M et al. Thiopurine methyltransferase (TPMT) genotype and early treatment response to mercaptopurine in childhood acute lymphoblastic leukemia. JAMA 2005; 293: 1485–1489.
van der Velden VH, Panzer-Grumayer ER, Cazzaniga G, Flohr T, Sutton R, Schrauder A et al. Optimization of PCR-based minimal residual disease diagnostics for childhood acute lymphoblastic leukemia in a multi-center setting. Leukemia 2007; 21: 706–713.
Lauten M, Zimmermann M, Reiter A, Beier R, Gadner H, Niemeyer C et al. Bone marrow day 15 has an additional impact on the prediction of event free survival in children with acute lymphoblastic leukemia characterized by the prednisone response. Blood 2002; 100 (11): 69a, abstract [250].
Nachman JB, Sather HN, Sensel MG, Trigg ME, Cherlow JM, Lukens JN et al. Augmented post-induction therapy for children with high-risk acute lymphoblastic leukemia and a slow response to initial therapy. N Engl J Med 1998; 338: 1663–1671.
Schrappe M, Reiter A, Zimmermann M, Harbott J, Ludwig WD, Henze G et al. Long-term results of four consecutive trials in childhood ALL performed by the ALL-BFM study group from 1981 to 1995. Berlin-Frankfurt-Munster. Leukemia 2000; 14: 2205–2222.
Bene MC, Castoldi G, Knapp W, Ludwig WD, Matutes E, Orfao A et al. Proposals for the immunological classification of acute leukemias. European Group for the Immunological Characterization of Leukemias (EGIL). Leukemia 1995; 9: 1783–1786.
Hiddemann W, Wormann B, Ritter J, Thiel E, Gohde W, Lahme B et al. Frequency and clinical significance of DNA aneuploidy in acute leukemia. Ann N Y Acad Sci 1986; 468: 227–240.
Pongers-Willemse MJ, Seriu T, Stolz F, d’Aniello E, Gameiro P, Pisa P et al. Primers and protocols for standardized detection of minimal residual disease in acute lymphoblastic leukemia using immunoglobulin and T cell receptor gene rearrangements and TAL1 deletions as PCR targets: report of the BIOMED-1 CONCERTED ACTION: investigation of minimal residual disease in acute leukemia. Leukemia 1999; 13: 110–118.
Szczepanski T, Pongers Willemse MJ, Langerak AW, Harts WA, Wijkhuijs AJ, van Wering ER et al. Ig heavy chain gene rearrangements in T-cell acute lymphoblastic leukemia exhibit predominant DH6-19 and DH7-27 gene usage, can result in complete V-D-J rearrangements, and are rare in T-cell receptor alpha beta lineage. Blood 1999; 93: 4079–4085.
van Dongen JJ, Langerak AW, Bruggemann M, Evans PA, Hummel M, Lavender FL et al. Design and standardization of PCR primers and protocols for detection of clonal immunoglobulin and T-cell receptor gene recombinations in suspect lymphoproliferations: report of the BIOMED-2 Concerted Action BMH4-CT98-3936. Leukemia 2003; 17: 2257–2317.
Langerak AW, Wolvers-Tettero IL, van Gastel-Mol EJ, Oud ME, van Dongen JJ . Basic helix-loop-helix proteins E2A and HEB induce immature T-cell receptor rearrangements in nonlymphoid cells. Blood 2001; 98: 2456–2465.
van der Velden VH, Wijkhuijs JM, Jacobs DC, van Wering ER, van Dongen JJ . T cell receptor gamma gene rearrangements as targets for detection of minimal residual disease in acute lymphoblastic leukemia by real-time quantitative PCR analysis. Leukemia 2002; 16: 1372–1380.
van der Velden VH, Willemse MJ, van der Schoot CE, Hahlen K, van Wering ER, van Dongen JJ . Immunoglobulin kappa deleting element rearrangements in precursor-B acute lymphoblastic leukemia are stable targets for detection of minimal residual disease by real-time quantitative PCR. Leukemia 2002; 16: 928–936.
Verhagen OJ, Willemse MJ, Breunis WB, Wijkhuijs AJ, Jacobs DC, Joosten SA et al. Application of germline IGH probes in real-time quantitative PCR for the detection of minimal residual disease in acute lymphoblastic leukemia. Leukemia 2000; 14: 1426–1435.
Pongers Willemse MJ, Verhagen OJ, Tibbe GJ, Wijkhuijs AJ, de Haas V, Roovers E et al. Real-time quantitative PCR for the detection of minimal residual disease in acute lymphoblastic leukemia using junctional region specific TaqMan probes. Leukemia 1998; 12: 2006–2014.
van der Velden VH, Cazzaniga G, Schrauder A, Hancock J, Bader P, Panzer-Grumayer ER et al. Analysis of minimal residual disease by Ig/TCR gene rearrangements: guidelines for interpretation of real-time quantitative PCR data. Leukemia 2007; 21: 604–611.
Fronkova E, Madzo J, Zuna J, Reznickova L, Muzikova K, Hrusak O et al. TEL/AML 1 real-time quantitative reverse transcriptase PCR can complement minimal residual disease assessment in childhood ALL. Leukemia 2005; 19: 1296–1297.
Willemse MJ, Seriu T, Hettinger K, d’Aniello E, Hop WC, Panzer Grumayer ER et al. Detection of minimal residual disease identifies differences in treatment response between T-ALL and precursor B-ALL. Blood 2002; 99: 4386–4393.
Panzer Grumayer ER, Schneider M, Panzer S, Fasching K, Gadner H . Rapid molecular response during early induction chemotherapy predicts a good outcome in childhood acute lymphoblastic leukemia. Blood 2000; 95: 790–794.
Basso G, Gaipa G, Valsecchi MG, Veltroni M, Dworczak M, Ratei R et al. Early evaluation of bone marrow minimal residual disease by flowcytometry on day 15 is feasible on a multicenter basis and bears strong prognostic value in childhood acute lymphoblastic leukemia. The AIEOP-BFM experience. Blood 2007; 110 (11): 426a, abstract [1423].
Mejstrikova E, Fronkova E, Batinic D, Dubravcic K, Kiss F, Kappelmayer J et al. Standardized 4 color flow cytometric minimal residual disease detection failed to overcome regeneration problems but identifies early blast clearence predictive of molecular remission after induction in childhood B lineage leukemia. Blood 2006; 108 (11): 521a–522a, abstract [1842].
Borowitz MJ, Pullen DJ, Shuster JJ, Viswanatha D, Montgomery K, Willman CL et al. Minimal residual disease detection in childhood precursor-B-cell acute lymphoblastic leukemia: relation to other risk factors. A Children's Oncology Group study. Leukemia 2003; 17: 1566–1572.
Madzo J, Zuna J, Muzikova K, Kalinova M, Krejci O, Hrusak O et al. Slower molecular response to treatment predicts poor outcome in patients with TEL/AML1 positive acute lymphoblastic leukemia: prospective real-time quantitative reverse transcriptase-polymerase chain reaction study. Cancer 2003; 97: 105–113.
Trueworthy R, Shuster J, Look T, Crist W, Borowitz M, Carroll A et al. Ploidy of lymphoblasts is the strongest predictor of treatment outcome in B-progenitor cell acute lymphoblastic leukemia of childhood: a Pediatric Oncology Group study. J Clin Oncol 1992; 10: 606–613.
Acknowledgements
This work was supported by MSM0021620813, MZO00064203, MZdNR8269-3/2005, Israel Cancer Association and Children's Cancer Foundation of Hong Kong. We thank the following participating clinical centers for clinical management and sample collection: Czech Republic: Brno (J Sterba), Ceske Budejovice (Y Jabali), Hradec Králové (J Hak), Olomouc (V Mihál), Ostrava (B Blazek), Plzeň (Z Černá), Prague (J Stary), Ústí nad Labem (D Prochazkova); Israel: Afula (H Gavriel), Beer-Sheva (J Kapelushnik), Haifa Bnei-Zion (D Attias), Haifa Rambam (R Elhasid), Holon (A Ballin), Jerusalem Hadassah (M Weintraub), Jerusalem Shaarei Zedek (H Miskin), Petah-Tikva (G Avrahami), Rehovot (D Sthoeger), Tel Aviv (Y Burstein), Tel Hashomer (B Bielorai). We also thank S Bendova for sequencing and A Vrzalova for data management.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fronkova, E., Mejstrikova, E., Avigad, S. et al. Minimal residual disease (MRD) analysis in the non-MRD-based ALL IC-BFM 2002 protocol for childhood ALL: is it possible to avoid MRD testing?. Leukemia 22, 989–997 (2008). https://doi.org/10.1038/leu.2008.22
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/leu.2008.22
Keywords
This article is cited by
-
Measurable residual disease (MRD)-testing in haematological and solid cancers
Leukemia (2024)
-
Lymphocytes from B-acute lymphoblastic leukemia patients present differential regulation of the adenosinergic axis depending on risk stratification
Discover Oncology (2022)
-
Correlation of Day 8 Steroid Response with Bone Marrow Status Measured on Days 14 and 35, in Patients with Acute Lymphoblastic Leukemia Being Treated with BFM Protocol
Indian Journal of Hematology and Blood Transfusion (2019)
-
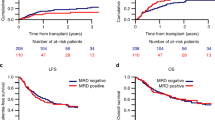
Next-generation sequencing indicates false-positive MRD results and better predicts prognosis after SCT in patients with childhood ALL
Bone Marrow Transplantation (2017)
-
Prediction of outcomes by early treatment responses in childhood T-cell acute lymphoblastic leukemia: a retrospective study in China
BMC Pediatrics (2015)