Abstract
Objective:
The objective of this study was to determine changes in neutrophil volume conductivity scatter (VCS) parameters and their distribution widths (DW) in neonatal sepsis and to estimate their optimal cutoff levels using receiver operating characteristic (ROC) curves.
Study Design:
In a cohort of neonates evaluated for sepsis, blood counts and blood culture were performed initially, with repeat counts and C-reactive protein (CRP) done after 24 to 48 h. Neutrophil VCS parameters from both the initial and repeat blood counts were analyzed. Babies were classified as having blood culture-positive sepsis, probable sepsis (clinical course consistent with sepsis and CRP-positive, but culture-negative) and no sepsis (clinical course not compatible with sepsis, culture- and CRP-negative).
Results:
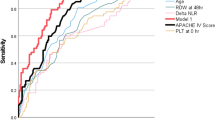
A total of 600 babies were included: 240 (40%) babies in the sepsis group and 360 (60%) babies in the control group. All the neutrophil VCS parameters and their DWs (except for low angle light scatter in the repeat counts) were significantly different between the two groups, with an area under curve in the ROC curve of >0.6 for most parameters. The five most significant VCS parameters (mean neutrophil volume (MNV), median angle light scatter (MALS), lower median angle light scatter (LMALS), MNV-DW and ALL-DW) had around 65 to 75% sensitivity and specificity. A combination of leukopenia, thrombocytopenia, MNV and LMALS had a likelihood ratio (LR)+ of 15.3 and LR− of 0.17. With a pre-test probability of 40%, post-test probability increased to 91% for a positive test and decreased to 10% for a negative test. A prospective validation study was performed recruiting an additional 60 babies, which showed similar results, assuring that the cutoffs were robust.
Conclusion:
Neutrophil VCS parameters cannot be considered as stand-alone tests to diagnose or rule out neonatal sepsis, but can be used in combination with other hematological screening tests to improve the diagnostic accuracy of the neonatal sepsis screen.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Qazi SA, Stoll BJ . Neonatal sepsis: a major global public health challenge. Pediatr Infect Dis J 2009; 28: S1–S2.
Newman TB, Puopolo KM, Wi S, Draper D, Escobar GJ . Interpreting complete blood counts soon after birth in newborns at risk for sepsis. Pediatrics 2010; 126: 903–909.
Yang AP, Liu J, Yue LH, Wang HQ, Yang WJ, Yang GH . Neutrophil CD64 combined with PCT, CRP and WBC improves the sensitivity for the early diagnosis of neonatal sepsis. Clin Chem Lab Med 2015; 54: 345–351.
Hedley BD, Keeney M, Chin-Yee I, Brown W . Initial performance evaluation of the UniCel DxH 800 Coulter cellular analysis system. Int J Lab Hematol 2011; 33: 45–56.
Chaves F, Tierno B, Xu D . Quantitative determination of neutrophil VCS parameters by the Coulter Automated Hematology Analyzer: new and reliable indicators for acute bacterial infection. Am J Clin Pathol 2005; 124: 440–444.
Lee JC, Ahern TP, Chaves FP, Quillen K . Utility of hematologic and volume, conductivity, and scatter parameters from umbilical cord blood in predicting chorioamnionitis. Int J Lab Hematol 2010; 32: 351–359.
Manroe BL, Weinberg AG, Rosenfeld CR, Browne R . The neonatal blood count in health and disease. I. Reference values for neutrophilic cells. J Pediatr 1979; 95: 89–98.
Celik IH, Demirel G, Aksoy HT, Erdeve O, Tuncer E, Biyikli Z et al. Automated determination of neutrophil VCS parameters in diagnosis and treatment efficacy of neonatal sepsis. Pediatr Res 2012; 71: 121–125.
Bhargava M, Saluja S, Sindhuri U, Saraf A, Sharma P . Elevated mean neutrophil volume+ CRP is a highly sensitive and specific predictor of neonatal sepsis. Int J Lab Hematol 2014; 36: e11–e14.
Raimondi F, Ferrara T, Capasso L, Sellitto M, Landolfo F, Romano A et al. Automated determination of neutrophil volume as screening test for late-onset sepsis in very low birth infants. Pediatr Infect Dis J 2010; 29: 288.
Çelik HT, Portakal O, Yigit S, Hascelik G, Korkmaz A, Yurdakok M . Comparison of the efficacy of new leukocyte parameters with serum C-reactive protein, procalcitonin, interleukin-6 levels in the diagnosis of neonatal sepsis. Pediatr Int 2015; 58: 119–125.
Mouzinho A, Rosenfeld CR, Sanchez PJ, Risser R . Revised reference ranges for circulating neutrophils in very-low-birth-weight neonates. Pediatrics 1994; 94: 76–82.
Schmutz N, Henry E, Jopling J, Christensen RD . Expected ranges for blood neutrophil concentrations of neonates: the Manroe and Mouzinho charts revisited. J Perinatol 2008; 28: 275–281.
Fowlie PW, Schmidt B . Diagnostic tests for bacterial infection from birth to 90 days—a systematic review. Arch Dis Child Fetal Neonatal Ed 1998; 78: F92–F98.
Benitz WE, Han MY, Madan A, Ramachandra P . Serial serum C-reactive protein levels in the diagnosis of neonatal infection. Pediatrics 1998; 102: e41–e41.
Acknowledgements
The authors gratefully acknowledge the contribution of Mr. Philips Jesuraj in processing of samples and data acquisition. This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Journal of Perinatology website
Supplementary information
Rights and permissions
About this article
Cite this article
Abiramalatha, T., Santhanam, S., Mammen, J. et al. Utility of neutrophil volume conductivity scatter (VCS) parameter changes as sepsis screen in neonates. J Perinatol 36, 733–738 (2016). https://doi.org/10.1038/jp.2016.69
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2016.69
This article is cited by
-
Neutrophil Volume, conductivity and scatter (VCS) as a screening tool in neonatal sepsis
Scientific Reports (2020)