Abstract
Objective:
To investigate the accuracy of electrical cardiometry (EC) to measure stroke volume (SV) and cardiac output (CO) and to provide gestational age (GA) and birth weight (BW)-based reference data for SV and CO in hemodynamically stable preterm neonates.
Study Design:
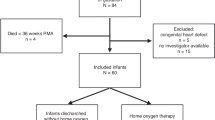
Prospective observational blinded study. Paired measurements of SV and CO on stable preterm infants without any hemodynamic compromise were carried out using EC (SVEC) and echocardiography (SVECHO).
Results:
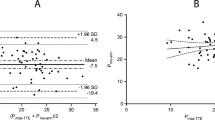
Seventy-nine preterm neonates (mean GA: 31±3.2 weeks) were enrolled. A good correlation was found for SV (r=0.743; P<0.0001) and CO (r=0.7; P<0.0001) measured by EC and echocardiography. These correlations remained significant after adjusting for GA, patent ductus arteriosus and type of respiratory support (SV: St.β=0.48, P<0.0001 and CO: St.β=0.69, P<0.0001). Mean biases (and variabilities) were −1.1 (from 0.7 to −2.9) ml and −0.21 (from 0.15 to −0.55) l min−1 for SV and CO, respectively. Local regression shows a tendency for EC to overestimate SV and CO especially at higher values (at about >2 ml and >0.4 l min−1, respectively). Coefficient of variation of SV was 48.9% and 52%, for EC and echocardiography. SV and CO rose with increasing GA and BW following an exponential equation (R2>0.8).
Conclusion:
Measuring SV and CO with EC in hemodynamically stable preterm infants shows good correlation and variability similar to that of echocardiography. A trend to overestimation exists at highest values, but it is unlikely to be clinically significant. Reference GA and BW-based nomograms for SV and CO are provided.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Kubicek WG, Karnegis JN, Patterson RP, Witsoe DA, Mattson RH . Development and evaluation of an impedance cardiac output system. Aerosp Med 1966; 37: 1208–1212.
Osypka MJ, Bernstein DP . Electrophysiologic principles and theory of stroke volume determination by thoracic electrical bioimpedance. AACN Clin Issues 1999; 10: 385–399.
Bernstein DP, Lemmens HJ . Stroke volume equation for impedance cardiography. Med Biol Eng Comput 2005; 43: 443–450.
Osthaus WA, Huber D, Beck C, Winterhalter M, Boethig D, Wessel A et al. Comparison of electrical velocimetry and transpulmonary thermodilution for measuring cardiac output in piglets. Paediatr Anaesth 2007; 17: 749–755.
Norozi K, Beck C, Osthaus WA, Wille I, Wessel A, Bertram H . Electrical velocimetry for measuring cardiac output in children with congenital heart disease. Br J Anaesth 2008; 100: 88–94.
Schubert S, Schmitz T, Weiss M, Nagdyman N, Huebler M, Alexi-Meskishvili V et al. Continuous, non-invasive techniques to determine cardiac output in children after cardiac surgery: evaluation of transesophageal Doppler and electric velocimetry. J Clin Monit Comput 2008; 22: 299–307.
Tomaske M, Knirsch W, Kretschmar O, Balmer C, Woitzek K, Schmitz A et al. Evaluation of the Aesculon cardiac output monitor by subxiphoidal Doppler flow measurement in children with congenital heart defects. Eur J Anaesthesiol 2009; 26: 412–415.
Mekis D, Kamenik M, Starc V, Jeretin S . Cardiac output measurements with electrical velocimetry in patients undergoing CABG surgery: a comparison with intermittent thermodilution. Eur J Anaesthesiol 2008; 25: 237–242.
Schmidt C, Theilmeier G, Van Aken H, Korsmeier P, Wirtz SP, Berendes E et al. Comparison of electrical velocimetry and transoesophageal Doppler echocardiography for measuring stroke volume and cardiac output. Br J Anaesth 2005; 95: 603–610.
Grollmuss O, Demontoux S, Capderou A, Serraf A, Belli E . Electrical velocimetry as a tool for measuring cardiac output in small infants after heart surgery. Intensive Care Med 2012; 38: 1032–1039.
Zoremba N, Bickenbach J, Krauss B, Rossaint R, Kuhlen R, Schälte G . Comparison of electrical velocimetry and thermodilution techniques for the measurement of cardiac output. Acta Anaesthesiol Scand 2007; 51: 1314–1319.
Archer TL, Conrad BE, Suresh P, Tarsa M . Electrical velocimetry demonstrates the increase in cardiac output and decrease in systemic vascular resistance accompanying cesarean delivery and oxytocin administration. J Clin Anesth 2012; 24: 79–82.
Rauch R, Welisch E, Lansdell N, Burrill E, Jones J, Robinson T et al. Non-invasive measurement of cardiac output in obese children and adolescents: comparison of electrical cardiometry and transthoracic Doppler echocardiography. J Clin Monit Comput 2013; 27: 187–193.
Blohm M, Obrecht D, Hartwich J, Mueller G, Kersten J, Weil J et al. Impedance cardiography (electrical velocimetry) and transthoracic echocardiography for non-invasive cardiac output monitoring in pediatric intensive care patients: a prospective single-center observational study. Crit Care 2014; 18 (6): 603.
Noori S, Drabu B, Soleymani S, Seri I. Continuous non-invasive cardiac output measurements in the neonate by electrical velocimetry: a comparison with echocardiography. Arch Dis Child Fetal Neonatal Ed 2012; 97: F340–F343.
Grollmuss O, Gonzalez P . Non-invasive cardiac output measurement in low and very low birth weight infants: a method comparison. Front Pediatr 2014; 2: 16.
Lien R, Hsu KH, Chu JJ, Chang YS . Hemodynamic alterations recorded by electrical cardiometry during ligation of ductus arteriosus in preterm infants. Eur J Pediatr 2014; 174 (4): 543–550.
Goldstein B, Giroir B, Randolph A, International Consensus Conference on Pediatric Sepsis. International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in paediatrics. Pediatr Crit Care Med 2005; 6: 2–8.
Bland JM, Altman DG . Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986; 1: 307–310.
Norusis M . SPSS 13.0 Advanced Statistical Procedures Companion. Prentice Hall Inc.: Upper Saddle River, NJ, USA, 2004.
Cleveland WS . Robust locally weighted regression and smoothing scatterplots. J Am Stat Assoc 1979; 74: 829–836.
De Luca D, Zecca E, Corsello M, Tiberi E, Semeraro C, Romagnoli C . Attempt to improve transcutaneous bilirubinometry: a double-blind study of Medick BiliMed versus Respironics BiliCheck. Arch Dis Child Fetal Neonatal Ed 2008; 93: F135–F139.
Cameron AC, Windmeijer FAG . An R-squared measure of goodness of fit for some common nonlinear regression models. J Econom 1997; 77: 329–342.
Song R, Rich W, Kim JH, Finer NN, Katheria AC . The use of electrical cardiometry for continuous cardiac output monitoring in preterm neonates: a validation study. Am J Perinatol 2014; 31 (12): 1105–1110.
Cecconi M, Rhodes A, Poloniecki J, Della Rocca G, Grounds RM . Bench-to-bedside review: the importance of the precision of the reference technique in method comparison studies—with specific reference to the measurement of cardiac output. Crit Care 2009; 13 (1): 201.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Boet, A., Jourdain, G., Demontoux, S. et al. Stroke volume and cardiac output evaluation by electrical cardiometry: accuracy and reference nomograms in hemodynamically stable preterm neonates. J Perinatol 36, 748–752 (2016). https://doi.org/10.1038/jp.2016.65
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2016.65
This article is cited by
-
Electrical Cardiometry during transition and short-term outcome in very preterm infants: a prospective observational study
European Journal of Pediatrics (2024)
-
Assessing fluid responsiveness with ultrasound in the neonatal intensive care setting: the mini-fluid challenge
European Journal of Pediatrics (2024)
-
Hemodynamic evaluation in preterm infants using ultrasonic cardiac output monitor (USCOM)
European Journal of Pediatrics (2024)
-
Effect of assessing velocity time integral at different locations across ventricular outflow tracts when calculating cardiac output in neonates
European Journal of Pediatrics (2023)
-
Impact of patent ductus arteriosus on non-invasive assessments of lung fluids in very preterm infants during the transitional period
European Journal of Pediatrics (2023)