Abstract
Objective:
To investigate the association between the number of prenatal visits (PNVs) and pregnancy outcomes in women with gestational diabetes (GDM) and Type 2 diabetes mellitus (DM).
Study Design:
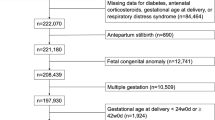
A 4-year prospective cohort study of women with GDM and DM and was conducted. Patients ⩾75th percentile for number of PNVs were compared with those ⩽25th percentile. The primary outcomes were large for gestational age (LGA) with birth weight >90% and neonatal intensive care unit (NICU) admission for >24 h. Secondary neonatal outcomes included severe LGA (>95%), shoulder dystocia, hyperbilirubinemia requiring phototherapy, neonatal hypoglycemia, low 5 min APGAR score (<7) and preterm birth (prior to 37 weeks). Secondary maternal outcomes included mean third trimester fasting blood glucose, hemoglobin A1c (Hgb A1c) in labor, preeclampsia, gestational weight gain over Institute of Medicine recommendations, mode of delivery and maternal readmission within 30 days. Logistic regression was used to adjust for maternal race, nulliparity and body mass index.
Results:
Of the 305 women, 4 were excluded for unknown number of PNVs. Among the 301 included, the average number of visits was 12. Rates of LGA were similar between the high (28%) compared with low (18%) utilization groups (adjusted odds ratio (aOR) 1.69; 95% confidence interval (CI) 0.81–3.54). The high utilization group was 85% less likely to deliver an infant requiring NICU admission (aOR 0.15; 95% CI 0.04–0.53) and 59% less likely to have a preterm birth (aOR 0.41; 95% CI 0.21–0.80). A time-to-event analysis to account for the fact that patients who delivered earlier had fewer weeks to experience PNVs showed that the risk for NICU admission was still significantly lower in the high PNV utilization group (hazard ratio 0.15; 95% CI 0.04–0.51) after adjusting for confounders in a Cox proportional hazard model. The mean Hgb A1c at the time of delivery was significantly better in the high (6.4%) compared with low (6.9%) utilization groups (P=0.01). There were no differences in other maternal outcomes based on prenatal care utilization.
Conclusions:
Diabetic women with high PNV utilization have better glycemic control in the 3 months prior to delivery and are significantly less likely to deliver preterm infants or infants requiring NICU admission. There may be innovative ways to provide prenatal care for GDM and DM to optimize maternal and neonatal outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Albrecht SS, Kuklina EV, Bansil P, Jamieson DJ, Whiteman MK, Kourtis AP et al. Diabetes trends among delivery hospitalizations in the U.S., 1994–2004. Diabetes Care 2010; 33 (4): 768–773.
Committee on Practice Bulletin—Obstetrics. Practice Bulletin No. 137: gestational diabetes mellitus. Obstet Gynecol 2013; 122 (2 Pt 1): 406–416.
American Academy of Pediatrics, American College of Obstetricians and Gynecologists. Guidelines for perinatal care. 7th edn. Elk Grove Village (IL): AAP; American College of Obstetricians and Gynecologists: Washington, DC, 2012, p. 106.
Landon MB, Spong CY, Thom E, Carpenter MW, Ramin SM, Casey B et al. A multicenter, randomized trial of treatment for mild gestational diabetes. N Engl J Med 2009; 361 (14): 1339–1348.
Crowther CA, Hiller JE, Moss JR, McPhee AJ, Jeffries WS, Robinson JS . Effect of treatment of gestational diabetes mellitus on pregnancy outcomes. N Engl J Med 2005; 352 (24): 2477–2486.
Poolsup N, Suksomboon N, Amin M . Effect of treatment of gestational diabetes mellitus: a systematic review and meta-analysis. PLoS One 2014; 9 (3): e92485.
Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care 2003; 26 (Suppl 1): S5–S20.
Alexander GR, Himes JH, Kaufman RB, Mor J, Kogan M . A United States National reference for fetal growth. Obstet Gynecol 1996; 87 (2 I): 163–168.
American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 101: ultrasonography in pregnancy. Obstet Gynecol 2009; 113 (2, Part 1): 451–461.
Institute of Medicine, National Research Council Committee to Reexamine IOMPWGThe National Academies Collection: reports funded by National Institutes of Health. In: Rasmussen KM, Yaktine AL (eds). Weight Gain During Pregnancy: Reexamining the Guidelines. National Academies Press (US), National Academy of Sciences: Washington (DC), USA, 2009.
McDuffie RS Jr, Beck A, Bischoff K, Cross J, Orleans M . Effect of frequency of prenatal care visits on perinatal outcome among low-risk women: a randomized controlled trial. J Am Med Assoc 1996; 275 (11): 847–851.
Carter EB, Tuuli MG, Caughey AB, Odibo AO, Macones GA, Cahill AG . Number of prenatal visits and pregnancy outcomes in low-risk women. J Perinatol 2016; 36 (3): 178–181.
Dowswell T, Carroli G, Duley L, Gates S, Gülmezoglu AM, Khan-Neelofur D et al. Alternative versus standard packages of antenatal care for low-risk pregnancy. Cochrane Database Syst Rev 2010; (10): CD000934.
Yogev Y, Langer O . Spontaneous preterm delivery and gestational diabetes: the impact of glycemic control. Arch Gynecol Obstet 2007; 276 (4): 361–365.
Alexander GR, Kotelchuck M . Assessing the role and effectiveness of prenatal care: history, challenges, and directions for future research. Public Health 2002; 116 (4): 306–316.
Foster DC, Guzick DS, Pulliam RP . The impact of prenatal care on fetal and neonatal death rates for uninsured patients: a 'natural experiment' in West Virginia. Obstet Gynecol 1992; 79 (1): 40–45.
Fisher ES, LoGerfo JP, Daling JR . Prenatal care and pregnancy outcomes during the recession: the Washington State experience. Am J Public Health 1985; 75 (8): 866–869.
Strobino DM, Chase GA, Kim YJ, Crawley BE, Salim JH, Baruffi G . The impact of the Mississippi improved Child Health Project on prenatal care and low birthweight. Am J Public Health 1986; 76 (3): 274–278.
Epstein AM, Newhouse JP . Impact of Medicaid expansion on early prenatal care and health outcomes. Health Care Financ Rev 1998; 19 (4): 85–99.
Peoles MD, Grimson RC, Lacy Daughtry G . Evaluation of the effects of the North Carolina improved pregnancy outcome project: implications for state-level decision-making. Am J Public Health 1984; 74 (6): 547–554.
Nielsen KK, Kapur A, Damm P, de Courten M, Bygbjerg IC . From screening to postpartum follow-up - the determinants and barriers for gestational diabetes mellitus (GDM) services, a systematic review. BMC Pregnancy Childbirth 2014; 14 (1): 41.
Housden L, Wong ST, Dawes M . Effectiveness of group medical visits for improving diabetes care: a systematic review and meta-analysis. CMAJ 2013; 185 (13): E635–E644.
Ickovics JR, Kershaw TS, Westdahl C, Magriples U, Massey Z, Reynolds H et al. Group prenatal care and perinatal outcomes: a randomized controlled trial. Obstet Gynecol 2007; 110 (2 I): 330–339.
Schellinger MM, Abernathy MP, Amerman B, May C, Foxlow LA, Carter AL et al. Improved outcomes for hispanic women with gestational diabetes using the Centering Pregnancy© Group Prenatal Care Model. Matern Child Health J 2016 (e-pub ahead of print 16 July 2016).
Mazzoni SE, Hill PK, Webster KW, Heinrichs GA, Hoffman MC . Group prenatal care for women with gestational diabetes. J Matern Fetal Neonatal Med 2015; 29 (17): 2852–2856.
Acknowledgements
This study was conducted in St Louis, Missouri at the Washington University School of Medicine, Department of Obstetrics and Gynecology, Division of Maternal Fetal Medicine. Dr Carter is supported by an NIH T32 training grant (5T32HD055172-05). This study was funded by R01HD061619-01A1 (PI: Cahill) and a grant from the Thrasher Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Carter, E., Tuuli, M., Odibo, A. et al. Prenatal visit utilization and outcomes in pregnant women with type II and gestational diabetes. J Perinatol 37, 122–126 (2017). https://doi.org/10.1038/jp.2016.175
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2016.175
This article is cited by
-
Perinatal outcomes of frequent attendance in midwifery care in the Netherlands: a retrospective cohort study
BMC Pregnancy and Childbirth (2020)