Abstract
Objective:
Health-care leaders place significant focus on reducing the average length of stay (ALOS). We examined the relationships among ALOS, cost and clinical outcomes using a neonatal intensive care unit (NICU) simulation model.
Study Design:
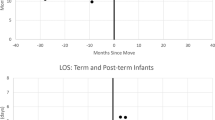
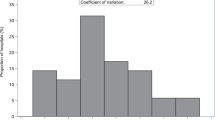
A discrete-event NICU simulation model based on the Duke NICU was created. To identify the relationships among ALOS, cost and clinical outcomes, we replaced the standard probability distributions with composite distributions representing the best and worst outcomes published by the National Institutes of Health Neonatal Research Network.
Result:
Both average cost per patient and average cost per ⩽28 week patient were lower in the best NICU ($16,400 vs $19,700 and $56,800 vs $76,700, respectively), while LOS remained higher (27 vs 24 days).
Conclusion:
Our model demonstrates that reducing LOS does not uniformly reduce hospital resource utilization. These results suggest that health-care leaders should not simply rely on initiatives to reduce LOS without clear line-of-sight on clinical outcomes as well.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Osnabrugge RL, Speir AM, Head SJ, Jones PG, Ailawadi G, Fonner CE et al. Cost, quality, and value in coronary artery bypass grafting. J Thorac Cardiovasc Surg 2014; 148 (6): 2729–2735.
Kaboli PJ, Go JT, Hockenberry J, Glasgow JM, Johnson SR, Rosenthal GE et al. Associations between reduced hospital length of stay and 30- day readmission rate and mortality: 14-year experience in 129 Veterans Affairs hospitals. Ann Intern Med 2012; 157 (12): 837–845.
Stambough JB, Nunley RM, Curry MC, Steger-May K, Clohisy JC . Rapid recovery protocols for primary total hip arthroplasty can safely reduce length of stay without increasing readmissions. J Arthroplasty 2015; 30: 521–526.
Tadros RO, Faries PL, Malik R, Vouyouka AG, Ting W, Dunn A et al. The effect of a hospitalist comanagement service on vascular surgery inpatients. J Vasc Surg 2015; 61: 1550–1555.
Nordstrom P, Gustafson Y, Michaelsson K, Nordstrom A . Length of hospital stay after hip fracture and short term risk of death after discharge: a total cohort study in Sweden. BMJ (Clin Res Ed) 2015; 350: h696.
Hintz SR, Bann CM, Ambalavanan N, Cotten CM, Das A, Higgins RD . Predicting time to hospital discharge for extremely preterm infants. Pediatrics 2010; 125 (1): e146–e154.
Bender G . Neonatal intensive care unit: predictive models for length of stay. J Perinatol. 2013; 33 (2): 147–153.
Lee HC, Bennett MV, Schulman J, Gould JB . Accounting for variation in length of NICU stay for extremely low birth weight infants. J Perinatol 2013; 33 (11): 872–876.
Pepler P, Uys D, Nel D . Predicting mortality and length-of-stay for neonatal admissions to private hospital neonatal intensive care units: a Southern African retrospective study. Afr Health Sci 2012; 12 (2): 166–173.
Bisquera JA, Cooper TR, Berseth CL . Impact of necrotizing enterocolitis on length of stay and hospital charges in very low birth weight infants. Pediatrics 2002; 109 (3): 423–428.
Stoll BJ, Hansen N, Fanaroff AA, Wright LL, Carlo WA, Ehrenkranz RA et al. Late-onset sepsis in very low birth weight neonates: the experience of the NICHD Neonatal Research Network. Pediatrics 2002; 110 (2 Part 1): 285–291.
Rogowski JA, Horbar JD, Plsek PE, Baker LS, Deterding J, Edwards WH et al. Economic implications of neonatal intensive care unit collaborative quality improvement. Pediatrics 2001; 107 (1): 23–29.
Horbar JD, Rogowski J, Plsek PE, Delmore P, Edwards WH, Hocker J et al. Collaborative quality improvement for neonatal intensive care. NIC/Q Project Investigators of the Vermont Oxford Network. Pediatrics 2001; 107 (1): 14–22.
Cotten CM, Oh W, McDonald S, Carlo W, Fanaroff AA, Duara S et al. Prolonged hospital stay for extremely premature infants: risk factors, center differences, and the impact of mortality on selecting a best-performing center. J Perinatol 2005; 25 (10): 650–655.
SAS Institute Inc SAS Simulation Studio 14.1: User’s Guide. SAS Institute: Cary, NC, 2015.
DeRienzo C, Shaw RJ, Meanor P, Lada E, Ferranti MJ, Tanaka D . A simulation tool to support and predict hospital and clinic staffing. Health Informatics J 2016 (e-pub ahead of print 29 February 2016; doi:10.1177/1460458216628314).
DeRienzo C, Tanaka D, Lada E, Meanor P Creating a SimNICU: Using SAS Simulation Studio to Model Staffing Needs in Clinical Environments. Proceedings of the SAS Global Conference, Washington, DC, 2014.
Stoll BJ, Hansen NI, Bell EF, Shankaran S, Laptook AR, Walsh MC et al. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics 2010; 126 (3): 443–456.
SAS Institute Inc JMP Pro 12: User’s Guide. SAS Institute: Cary, NC, 2015.
Russell RB, Green NS, Steiner CA, Meikle S, Howse JL, Poschman K et al. Cost of hospitalization for preterm and low birth weight infants in the United States. Pediatrics 2007; 120 (1): e1–e9.
Johnson TJ, Patel AL, Jegier BJ, Engstrom JL, Meier PP . Cost of morbidities in very low birth weight infants. J Pediatr 2013; 162 (2): 243–249.
Schulman J . Studying determinants of length of hospital stay. J Perinatol 2006; 26: 243–245.
Levit K, Ryan K, Elixhauser A, Stranges E, Kassed C, Coffey R . HCUP Facts and Figures: Statistics on Hospital-based Care in the United States in 2005. Agency for Healthcare Research and Quality: Rockville, MD, 2007. Available at http://www.hcup-us.ahrq.gov/reports.jsp.
Bolisetty S, Dhawan A, Abdel-Latif M, Bajuk B, Stack J . Intraventricular hemorrhage and neurodevelopmental outcomes in extreme preterm infants. Pediatrics 2014; 133 (1): 55–62.
Lee HC, Bennet MV, Schulman J, Gould JB . Accounting for variation in length of NICU stay for extremely low birth weight infants. J Perinatol 2013; 33 (11): 872–876.
St. John E, Nelson K, Cliver S, Bishnoi R, Goldenberg R . Cost of neonatal care according to gestational age at birth and survival status. Am J Obstet Gyncol 2000; 182 (1): 170–175.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
DeRienzo, C., Kohler, J., Lada, E. et al. Demonstrating the relationships of length of stay, cost and clinical outcomes in a simulated NICU. J Perinatol 36, 1128–1131 (2016). https://doi.org/10.1038/jp.2016.128
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2016.128
This article is cited by
-
Regional variation in cost of neonatal intensive care for extremely preterm infants
BMC Pediatrics (2021)