Abstract
Objectives:
To compare the degree of hemolysis in a group of direct antiglobulin test (DAT) positive (pos) African-American (AA) infants as measured by carboxyhemoglobin corrected (COHbc) for carbon monoxide in ambient air to a similar group of DAT negative (neg) ABO incompatible infants and a group without blood group incompatibility. To determine if COHbc is a better predictor of significant hyperbilirubinemia than DAT status.
Study Design:
A prospective study of 180 AA infants from the Well-Baby Nursery of an inner city community hospital, all of whose mothers were type O pos. Infants (60) were ABO incompatible DAT pos, 60 were ABO incompatible DAT neg and 60 were type O+. Blood for COHbc was drawn at the time of the infants’ initial bilirubin and the infants’ precise percentile on the Bhutani nomogram was calculated.
Result:
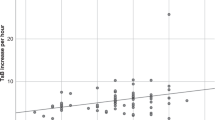
Mean COHbc of type O+ infants was 0.76±0.21 and 0.78±0.24% for ABO incompatible DAT neg infants (P=0.63). Mean CoHbc for the ABO incompatible DAT pos infants was 1.03±0.41% (P<0.0001 compared with both type O and DAT neg infants). Optimal cutoff on the receiver operating characteristic curve for COHbc to determine the risk for being in the Bhutani curve high risk zone was COHbc >0.90% (area under the curve(AUC) 0.8113). This was similar to the AUC of the receiver operating characteristic curve using any titer strength of DAT pos as a cutoff (0.7960).
Conclusion:
Although not greatly superior to the titer strength of DAT pos, COHbc is useful in determining if the etiology of severe hyperbilirubinemia is a hemolytic process.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Slusher TM, Zipursky A, Bhutani VK . A global need for affordable neonatal jaundice technologies. Semin Perinatol 2011; 35: 185–191.
American Academy of Pediatrics Subcommittee on Hyperbilirubinemia. Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics 2004; 114: 297–316.
Bhutani VK, Johnson L, Sivieri EM . Predictive ability of a predischarge hour-specific serum bilirubin for subsequent significant hyperbilirubinemia in healthy term and near-term infants. Pediatrics 1999; 13: 6–14.
Schutzman DL, Sekhon R, Hundalani S . Hour-specific bilirubin nomogram in infants with ABO incompatibility and direct Coombs-positive results. Arch Pediatr Adolesc Med 2010; 164: 1158–1164.
Kaplan M, Hammerman C, Vreman H, Wong RJ, Stevenson DK . Hemolysis and hyperbilirubinemia in antiglobulin positive, direct ABO blood group heterospecific neonates. J Pediatr 2010; 157: 772–777.
Sarici SU, Yurdakok M, Serdar MA, Oran O, Erdem G, Tekinalp G et al. An early (sixth hour) serum bilirubin measurement is useful in predicting the development of significant hyperbilirubuinemia and severe ABO hemolytic disease in a selective high-risk population of newborns with ABO incompatibility. Pediatrics 2002; 109: e53–e58.
Kaplan M, Hammerman C, Vremen HJ, Wong RJ, Stevenson DK . Direct antiglobulin titer strength and hyperbilirubinemia. Pediatrics 2014; 134: e1340–e1344.
Lapierre Y, Rigil D, Adam J, Josef D, Meyer F, Gerber S et al. The gel test: a new way to detect red cell antigen-antibody reactions. Transfusion 1990; 30: 109–113.
Stevenson DK, William A . Silverman lecture. J Perinatol 2014; 34: 1–5.
Herschel M, Karrison T, Wen M, Caldarelli L, Baron B . Evaluation of the direct antiglobulin (Coombs) test for identifying newborns at risk for hemolysis as determined by end-tidal carbon monoxide concentration (ETCOc); and comparison of the Coombs test with ETCOc for detecting significant jaundice. J Perinatol 2002; 22: 341–347.
Vreman HJ, Stevenson DK . Carboxyhemoglobin determined in neonatal blood with a CO-oximeter unaffected by fetal oxyhemoglobin. Clin Chem 1994; 40: 1522–1527.
Stevenson DK, Fanaroff AA, Maisels MJ, Young BWY, Wong RJ, Vreman HJ et al. Prediction of hyperbilirubinemia in near-term and term infants. Pediatrics 2001; 108: 31–39.
Herschel M, Karrsion T, Wen M, Caldarelli L, Baron B . Isoimmunization is unlikely to be the cause of hemolysis in ABO-incompatible but direct antiglobulin test negative neonates. Pediatrics 2002; 110: 127–130.
Cohen RS, Wong RJ, Stevenson DK . End-tidal breath carbon monoxide measurements: current directions. NeoReviews 2012; 13: e486–e490.
Kaplan M, Muroca M, Hammerman C, Rubaltelli FF, Vilei MT, Vreman HJ et al. Imbalance between production and conjugation of bilirubin: a fundamental concept in the mechanism of neonatal jaundice. Pediatrics 2002; 110: e47.
Beutler E, Gelbert T, Demina A . Racial variability in the UDP-glucuronosyl-transferase 1 (UGT1A1) promoter: a balanced polymorphism for regulation of bilirubin metabolism. Proc Natl Acad Sci USA 1998; 81: 505–511.
Bhutani VK, Wong R . Bilirubin induced neurologic dysfunction (BIND). Semin Fetal Neonatal Med 2015; 20: 1.
Acknowledgements
This study was supported in part by a grant from The Albert Einstein Society of the Einstein Healthcare Network.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Schutzman, D., Gatien, E., Ajayi, S. et al. Carboxyhemoglobin levels as a predictor of risk for significant hyperbilirubinemia in African-American DAT+ infants. J Perinatol 36, 386–388 (2016). https://doi.org/10.1038/jp.2015.206
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2015.206
This article is cited by
-
ABO hemolytic disease of the newborn: a need for clarity and consistency in diagnosis
Journal of Perinatology (2023)
-
Comparison of end-tidal carbon monoxide measurements with direct antiglobulin tests in the management of neonatal hyperbilirubinemia
Journal of Perinatology (2020)
-
Heme oxygenase-1 genetic variants and the conundrum of hyperbilirubinemia in African-American newborns
Journal of Perinatology (2018)
-
Effect of genetic variants of bilirubin metabolism on the degree of hyperbilirubinemia in African-American newborns
Journal of Perinatology (2017)