Abstract
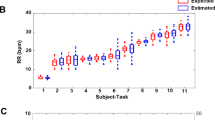
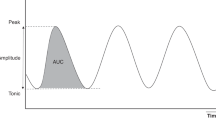
Pneumothorax is usually diagnosed when signs of life-threatening tension pneumothorax develop. The case report describes novel data derived from miniature superficial sensors that continuously monitored the amplitude and symmetry of the chest wall tidal displacement (TDi) in a premature infant that suffered from pneumothorax. Off-line analysis of the TDi revealed slowly progressing asymmetric ventilation that could be detected 38 min before the diagnosis was made. The TDi provides novel and valuable information that can assist in early detection and decision making.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
McIntosh N, Becher JC, Cunningham S, Stenson B, Laing IA, Lyon AJ et al. Clinical diagnosis of pneumothorax is late: use of trend data and decision support might allow preclinical detection. Pediatr Res 2000; 48: 408–415.
Bhatia R, Davis PG, Doyle LW, Wong C, Morley CJ . Identification of pneumothorax in very preterm infants. J Pediatr 2011; 159: 115–120.
Waisman D, Faingersh A, Levy C, Colman-Klotzman I, Rotschild A, Lichtenstein O et al. Transient decrease in PaCO2 and asymmetric chest wall dynamics in early progressing pneumothorax. Intensive Care Med 2013; 39: 137–145.
Waisman D, Levy C, Faingersh A, Klotzman FI, Konyukhov E, Kessel I et al. A new method for continuous monitoring of the chest wall movement to characterize hypoxemic episodes during HFOV. Intensive Care Med 2011; 37: 1174–1181.
Waisman D, Faingersh A, Levy C, Konyukhov E, Klotzman FI, Rotschild A et al. Early detection of deteriorating ventilation by monitoring bilateral chest wall dynamics in the rabbit. Intensive Care Med 2012; 38: 120–127.
Acknowledgements
Chest wall dynamics were measured by the equipment provided by Pneumedicare Ltd.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
DW, SK, AF, ICK and AL are involved in the development of a respiratory function monitor within a collaborative effort between the Technion—Israel Institute of Technology, Clalit Health Services and Pneumedicare Ltd. The remaining authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Waisman, D., Landesberg, A., Kohn, S. et al. Chest dynamics asymmetry facilitates earlier detection of pneumothorax. J Perinatol 36, 157–159 (2016). https://doi.org/10.1038/jp.2015.172
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2015.172