Abstract
Objective:
Human milk is the best form of nutrition for preterm infants and has been associated with a lower incidence of necrotizing enterocolitis (NEC). Infants that develop NEC have a higher incidence of feeding intolerance and longer hospitalizations. The combination of a donor milk bank and donor milk-derived fortifier has changed feeding practices in neonatal intensive care units (NICU). The purpose of this study is to assess the benefits and cost of an exclusive human milk (EHM) diet in very low birth weight (VLBW) infants in a community level III NICU.
Study Design:
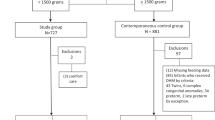
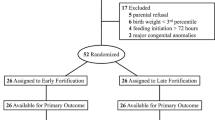
This is a retrospective study including preterm infants ⩽28 weeks and/or VLBW (⩽1500 g) who were enrolled from March 2009 until March 2014. Infants were grouped as follows: group H (entirely human milk based, born March 2012 to 2014), group B (bovine-based fortifier and maternal milk, born March 2009 to 2012), group M (mixed combination of maternal milk, bovine-based fortifier and formula, born March 2009 to 2012) and group F (formula fed infants, born March 2009 to 2012). Baseline characteristics among the four groups were similar.
Result:
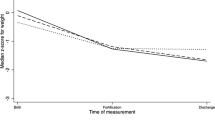
The study included 293 infants between gestational ages 23 to 34 weeks and birth weights between 490 and 1700 g. Feeding intolerance occurred less often (P<0.0001), number of days to full feeds was lower (P<0.001), incidence of NEC was lower (P<0.011), and total hospitalization costs were lower by up to $106,968 per infant (P<0.004) in those fed an EHM diet compared with the other groups. Average weight gain per day was similar among the four groups (18.5 to 20.6 g per day).
Conclusions:
Implementing an EHM diet in our VLBW infants has led to a significant decrease in the incidence of NEC. Other benefits of this diet include: decreased feeding intolerance, shorter time to full feeds, shorter length of stay, and lower hospital and physician charges for extremely premature and VLBW infants.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Viadyanathan G, Hay JW, Kim JH . Cost of necrotizing enterocolitis and cost-effectiveness of exclusively human milk based products in feeding extremely premature infants. Breastfeed Med 2011; 6: 1–9.
Neu J, Walker AW . Necrotizing enterocolitis. N Engl J Med 2011; 364: 255–264.
Simon NP . Follow-up for infants with necrotizing enterocolitis. Clin Perinatol 1994; 21: 411–424.
Tejani A, Dobias B, Nangia BS, Mahadevan R . Growth, health, and development after neonatal gut surgery: a long-term follow-up. Pediatrics 1978; 61: 685–693.
Hintz SR, Kendrick DE, Vohr BR, Poole WK, Higgins RD . Changes in neurodevelopmental outcomes at 18-22 months’ corrected age among infants of less than 25 weeks’ gestational age born in 1993-1999. Pediatrics 2005; 115: 1645–1651.
Schulzke SM, Deshpande GC, Patole SK . Neurodevelopmental outcomes of very low-birth-weight with necrotizing enterocolitis. Arch Pediatr Adolesc Med 2007; 161: 583–590.
Rees CM, Pierro A, Eaton S . Neurodevelopmental outcomes of neonates with medically and surgically treated necrotizing enterocolitis. Arch Dis Child Fetal Neonatal Ed 2007; 92: F193–F198.
Morales Y, Schanler RJ . Human milk and clinical outcomes in VLBW infants: how compelling is the evidence of benefit? Semin Perinatol 2007; 31: 83–88.
Christofalo EA, Schanler RJ, Blanco CL, Sullivan S, Trawoeger R, Kiechl-Kohlendorfer U et al. Randomized trial of exclusive human milk versus preterm formula diets in extremely premature infants. J Pediatr 2013; 163 (6): 1592–1595.
Hermann K, Carroll K . An exclusively human milk diet reduces necrotizing enterocolitis. Breastfeed Med 2014; 9 (4): 184–190.
Bhatia J . Human milk and the premature infant. Ann Nutr Metab 2013; 62 (suppl 3): 8–14.
Walker A . Breast milk as the gold standard for protective nutrients. J Pediatr 2010; 156: S3–S7.
World Health Organization (WHO). Baby-friendly hospital Initiative, 2010. Retrieved from http://www.who.int/nutrition/topics/bfhi/en/index.html.
American Academy of Pediatrics. Policy Statement: Breastfeeding and the use of Human Milk. Section on Breastfeeding. Pediatrics 2012; 129: e827–e841.
Schanler RJ, Lau C, Hurst NM, Smith EO . Randomized trial of donor human milk versus preterm formula as substitutes for mothers’ own milk in the feeding of extremely premature infants. Pediatrics 2005; 116: 400–406.
Sullivan S, Schanler RJ, Kim JH, Patel AL, Trawoger R, Kiechl-Kohlendorfer U et al. An exclusively human milk-based diet is associated with a lower rate of necrotizing enterocolitis than a diet of human milk and bovine milk-based products. J Pediatr 2010; 156: 562–567.
Brownell EA, Lussier MM, Herson VC, Hagadorn JI, Marinelli KA . Donor human milk bank data collection in North America: an assessment of current status and future needs. J Hum Lact 2013; 30: 47–53.
Boyd CA, Quigley MA, Brocklehurst P . Donor breast milk versus infant formula for preterm infants: a systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed 2007; 92: 169–175.
Quigley MA, Henderson G, Anthony MY, McGuire W . Formula milk versus donor breast milk for feeding preterm or low birth weight infants. Cochrane Database Syst Rev 2007; 17: 2971.
Bisquera JA, Cooper TR, Berseth CL . Impact of necrotizing enterocolitis on length of stay and hospital charges in very low birth weight infants. Pediatrics 2002; 109: 423–442.
Bell MJ, Ternberg JL, Feigin RD, Keating JP, Marshall R, Barton L et al. Neonatal necrotizing enterocolitis: therapeutic decisions based upon clinical staging. Ann Surg 1978; 187: 1–7.
Patel AL, Engstrom JL, Meier PP, Jegier BJ, Kimura RE . Calculating postnatal growth velocity in very low birth weight (VLBW) premature infants. J Perinatol 2009; 29 (9): 618–622.
Ghods E, Kreissl A, Brandstetter S, Fuiko R, Widhalm K . Head circumference catch up growth among preterm very low birth weight infants: effect on neurodevelopmental outcome. J Perinat Med 2011; 39 (5): 579–586.
Johnson TJ, Patel AL, Jegier B, Engstrom JL, Meier P . The cost of morbidities in very low birth weight infants. J Pediatr 2013; 162 (2): 243–249.
Carroll K, Hermann KR . The cost of using donor human milk in the nicu to achieve exclusively human milk feeding through 32 weeks postmenstrual age. Breastfeed Med 2013; 8: 286–290.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Assad, M., Elliott, M. & Abraham, J. Decreased cost and improved feeding tolerance in VLBW infants fed an exclusive human milk diet. J Perinatol 36, 216–220 (2016). https://doi.org/10.1038/jp.2015.168
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2015.168
This article is cited by
-
Mothers’ experiences of breast milk expression during separation from their hospitalized infants: a systematic review of qualitative evidence
BMC Pregnancy and Childbirth (2024)
-
Human milk derived fortifiers are associated with glucose, phosphorus, and calcium derangements
Journal of Perinatology (2024)
-
Implementing an exclusive human milk diet for preterm infants: real-world experience in diverse NICUs
BMC Pediatrics (2023)
-
Dilemmas in human milk fortification
Journal of Perinatology (2023)
-
A comparison of tertiary level NICU costs for infants born <1250 g supplemented with human versus bovine milk-based fortifiers
Journal of Perinatology (2023)