Abstract
Objective:
Bronchopulmonary dysplasia (BPD) is a pulmonary disease associated with poor neurodevelopmental and medical outcomes. Patients with BPD are medically fragile, at high risk for complications and require interdisciplinary care. We tested the hypothesis that a chronic care approach for BPD would improve neurodevelopmental outcomes relative to the National Institute of Child and Human Development Neonatal Research Network (NICHD NRN) and reduce medical complications.
Study Design:
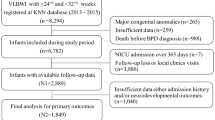
Infants were followed as inpatients and outpatients. Bayley developmental exams were carried out at 18–24 months of age and compared with the NICHD NRN report. Finally, rates of readmission (a proxy for medical complications) were compared before and after implementation of the Comprehensive Center for BPD (CCBPD).
Result:
Developmental scores obtained in 2007 and 2008 show that 12 and 10% of patients with moderate BPD (n=61) had Bayley Scores <70 for mental and motor indices respectively, whereas corresponding national rates were 35 and 26%. For patients with severe BPD (n=46), 15 and 11% of patients within the CCBPD vs 50 and 42% of national patients scored <70 for mental and motor indices, respectively. Finally, readmission rates dropped from 29% in the year before the implementation of the CCPD (n=269) to 5% thereafter (n=866, P<0.0001).
Conclusion:
The encouraging neurodevelopmental outcomes and readmission rates associated with a chronic care approach to BPD suggest these infants may be best served by a comprehensive interdisciplinary approach to care that focuses on neurodevelopment throughout the hospital stay.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Fanaroff AA, Wright LL, Stevenson DK, Shankaran S, Donovan EF, Ehrenkranz RA et al. Very-low-birth-weight outcomes of the National Institute of Child Health and Human Development Neonatal Research Network, May 1991 through December 1992. Am J Obstet Gynecol 1995; 173 (5): 1423–1431.
Stevenson DK, Wright LL, Lemons JA, Oh W, Korones SB, Papile LA et al. Very low birth weight outcomes of the National Institute of Child Health and Human Development Neonatal Research Network, January 1993 through December 1994. Am J Obstet Gynecol 1998; 179 (6 part 1): 1632–1639.
Lemons JA, Bauer CR, Oh W, Korones SB, Papile LA, Stoll BJ et al. Very low birth weight outcomes of the National Institute of Child health and human development neonatal research network, January 1995 through December 1996. NICHD Neonatal Research Network. Pediatr 2001; 107 (1): E1.
Fanaroff AA, Stoll BJ, Wright LL, Carlo WA, Ehrenkranz RA, Stark AR et al. Trends in neonatal morbidity and mortality for very low birthweight infants. Am J Obstet Gynecol 2007; 196 (2): 147. e141-148.
Walsh MC, Szefler S, Davis J, Allen M, Van Marter L, Abman S et al. Summary proceedings from the bronchopulmonary dysplasia group. Pediatr 2006; 117 (3 part 2): S52–S56.
Ehrenkranz RA, Walsh MC, Vohr BR, Jobe AH, Wright LL, Fanaroff AA et al. Validation of the National Institutes of Health consensus definition of bronchopulmonary dysplasia. Pediatr 2005; 116 (6): 1353–1360.
Bhandari A, Bhandari V . Pitfalls, problems, and progress in bronchopulmonary dysplasia. Pediatr 2009; 123 (6): 1562–1573.
Anderson PJ, Doyle LW . Neurodevelopmental outcome of bronchopulmonary dysplasia. Semin Perinatol 2006; 30 (4): 227–232.
Allen J, Zwerdling R, Ehrenkranz R, Gaultier C, Geggel R, Greenough A et al. Statement on the care of the child with chronic lung disease of infancy and childhood. Am J Respir Crit Care Med 2003; 168 (3): 356–396.
Wagner EH . The role of patient care teams in chronic disease management. BMJ 2000; 320: 569–572.
Gracey K, Talbot D, Lankford R, Dodge P . The changing face of bronchopulmonary dysplasia: part 1. Adv Neonatal Care 2002; 2 (6): 327–338.
Jarriel WS, Richardson P, Knapp RD, Hansen TN . A nonlinear regression analysis of nonlinear, passive-deflation flow-volume plots. Pediatric Pulmonol 1993; 15 (3): 175–182.
Hanin M, Susey K, Beck C, Gest A, Shepherd E . Behavioral signs of respiratory instability: the development and administration of a scale to monitor signs of respiratory distress during developmental interventions in infants with bronchopulmonary Dysplasia. Newborn Infant Nurs Rev 2009; 9 (3): 175–181.
Courtney SE, Weber KR, Breakie LA, Malin SW, Bender CV, Guo SM et al. Capillary blood gases in the neonate. A reassessment and review of the literature. Am J Dis Child 1990; 144 (2): 168–172.
Kim EH, Cohen RS, Ramachandran P . Effect of vascular puncture on blood gases in the newborn. Pediatric Pulmonol 1991; 10 (4): 287–290.
Rush MG, Engelhardt B, Parker RA, Hazinski TA . Double-blind, placebo-controlled trial of alternate-day furosemide therapy in infants with chronic bronchopulmonary dysplasia. J Pediatr 1990; 117 (1 part 1): 112–118.
Campbell SK, Kolobe TH, Osten ET, Lenke M, Girolami GL . Construct validity of the test of infant motor performance. Phys Ther 1995; 75 (7): 585–596.
Bayley N . Bayley Scales of Infant and Toddler Development. 3rd edn Harcourt Assessment: San Antonio, TX, 2006.
Bayley N . Bayley Scales of Infant Development. 2nd edn The Psychological Corporation: San Antonio, TX, 1993.
Wagner EH . Chronic disease management: what will it take to improve care for chronic illness? Eff Clin Pract 1998; 1 (1): 2–4.
Wagner EH, Austin BT, Davis C, Hindmarsh M, Schaefer J, Bonomi A . Improving chronic illness care: translating evidence into action. Health Aff (Millwood) 2001; 20 (6): 64–78.
Acknowledgements
We thank George Mandy, MD, Alicia Moise, MD, Rachel Brown, MD, Angela Gross, RN, BSN, Melissa Hanin, OT for their review of this article. We also thank all of the staff members of the inpatient and outpatient areas of the BPD program at Nationwide Children's Hospital for their dedication to the BPD program.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Shepherd, E., Knupp, A., Welty, S. et al. An interdisciplinary bronchopulmonary dysplasia program is associated with improved neurodevelopmental outcomes and fewer rehospitalizations. J Perinatol 32, 33–38 (2012). https://doi.org/10.1038/jp.2011.45
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2011.45
Keywords
This article is cited by
-
Validity and reliability of the behavioral signs of respiratory instability (BSRI) © scale during activity for infants with bronchopulmonary dysplasia
Journal of Perinatology (2023)
-
The Optimal State Scoring Tool: guidance for interdisciplinary care of infants with severe bronchopulmonary dysplasia and its relation to linear growth
Journal of Perinatology (2023)
-
In-hospital outcomes of late referrals for established bronchopulmonary dysplasia
Journal of Perinatology (2021)
-
Established severe BPD: is there a way out? Change of ventilatory paradigms
Pediatric Research (2021)
-
A multidisciplinary quality improvement effort to reduce bronchopulmonary dysplasia incidence
Journal of Perinatology (2020)