Abstract
Objective:
To identify factors associated with complications necessitating unplanned removal of peripherally inserted central venous catheters (PICCs) in neonates.
Study Design:
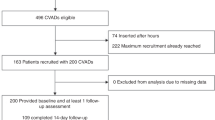
A before-and-after comparison following the exclusion of heparin from continuous infusions through PICCs placed by a designated team. Duration of use was assessed during epochs immediately preceding and following the practice change. Multivariable logistic regression was performed to identify independent risk factors associated with unplanned catheter removal.
Result:
We analyzed 189 PICC placements with heparin (epoch 1) and 188 with no heparin (epoch 2) added to infusions. Rates of complication (23.7 vs 17.2 per 1000 catheter days) and median durations of use (7 vs 8 days) did not differ significantly between the epochs. Non-central position of the catheter tip, use of dual lumen catheters and placement through the cephalic vein were independently associated with complications (each P<0.05).
Conclusion:
In neonates requiring short-term intravenous access, heparin may be safely omitted from continuous infusions without compromising catheter usability.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Linck DA, Donze A, Hamvas A . Neonatal peripherally inserted central catheter team: evolution and outcomes of a bedside-nurse-designed program. Adv Neonatal Care 2007; 7 (1): 22–29.
Evans M, Lentsch D . Percutaneously inserted polyurethane central catheters in the NICU: one unit's experience. Neonatal Netw 1999; 18 (6): 37–46.
Birch P, Ogden S, Hewson M . A randomized, controlled trial of heparin in total parenteral nutrition to prevent sepsis associated with neonatal long lines: the heparin in long line total parenteral nutrition (HILLTOP) trial. Arch Dis Child Fetal Neonatal Ed 2010; 95: F252–F257.
Uslu S, Ozdemir H, Comert S, Bolat F, Nuhoglu A . The effect of low-dose heparin on maintaining peripherally inserted percutaneous central venous catheters in neonates. J Perinatol 2010; 30 (12): 794–799.
Shah PS, Kalyn A, Satodia P, Dunn MS, Parvez B, Daneman A et al. A randomized, controlled trial of heparin versus placebo infusion to prolong the usability of peripherally placed percutaneous central venous catheters (PCVCs) in neonates: the HIP (heparin infusion for PVCV) study. Pediatrics 2007; 119: 284–291.
Kamala F, Boo NY, Cheah FC, Birinder K . Randomized controlled trial of heparin for prevention of blockage of peripherally inserted central catheters in neonates. Acta Paediatr 2002; 91: 1350–1356.
Klenner AF, Fusch C, Rakow A, Kadow I, Beyersdorff E, Eichler P et al. Benefit and risk of heparin for maintaining peripheral venous catheters in neonates: a placebo-controlled trial. J Peds 2003; 143: 741–745.
Shah PS, Shah VS . Continuous heparin infusion to prevent thrombosis and catheter occlusion in neonates with peripherally placed percutaneous central venous catheters. Cochrane Database Syst Rev 2008; (2): CD002772.
Mandrack M . Heparin errors continue despite prior, high-profile, fatal events. From the 17 July 2008 issue; 2008. Available at: http://www.ismp.org/newsletters/acutecare/articles/20080717.asp (accessed 04 November 2011).
Lesko SM, Mitchell AA, Epstien MF, Louik C, Giacoia GP, Shapiro S . Heparin use as a risk factor for intraventricular hemorrhage in low-birth-weight-infants. NEJM 1986; 314: 1156–1160.
Martchenke J, Boshkov L . Heparin-induced thrombocytopenia in neonates. Neonatal Netw 2005; 24: 33–37.
Hostetter MK . The iC3b receptor of Candida albicans and its roles in pathogenesis. Vaccine 2008; 26S: 1108–1112.
Ojala TH, Lehtonen L . A preliminary report – heparin counteracts indomethacin effect on ductus arteriosus in very low birthweight infants. Pediatr Crit Care Med 2007; 8 (3): 258–260.
Arimua J, Poole RL, Jeng M, Rhine W, Sharek P . Neonatal heparin overdose – a multidisciplinary team approach to medication error prevention. J Pediatr Pharmacol Ther 2008; 13 (2): 96–98.
Breaux CW, Duke D, Georgeson KE, Mestre JR . Calcium phosphate crystal occlusion of central venous catheters used for total parenteral nutrition in infants and children: prevention and treatment. J Pediatr Surg 1987; 22 (9): 829–832.
Racadio JM, Doellman DA, Johnson ND, Bean JA, Jacobs BR . Pediatric peripherally inserted central catheters: complication rates related to catheter tip location. Pediatrics 2001; 107 (2): e28.
Shanks RM, Donegan NP, Graber ML, Buckingham SE, Zegans ME, Cheung AL et al. Heparin stimulates Staphylococcus aureus biofilm formation. Infect Immun 2005; 73: 4596–4606.
Miller MR, Griswold M, Harris JM, Yenokyan G, Huskins C, Moss M et al. Decreasing PICU catheter-associated bloodstream infections: NACHRI's quality transformation efforts. Pediatrics 2010; 125: 206–213.
Curry S, Honeycutt M, Goins G, Gilliam C . Catheter-associated bloodstream infections in the NICU: getting to zero. Neonatal Netw 2009; 28 (3): 151–155.
Hsu J, Tsai M, Huang H, Lien R, Chu S, Huang C . Risk factors of catheter-related bloodstream infection with percutaneously inserted central venous catheters in very low birth weight infants: a center's experience in Taiwan. Pediatr Neonatol 2010; 51 (6): 336–342.
Acknowledgements
We would like to acknowledge the staff of the Department of Pharmacy at the UC Health University Hospital for their support. We gratefully acknowledge the assistance of Drs Steven Hoath and Eric Mueller in reviewing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Isemann, B., Sorrels, R. & Akinbi, H. Effect of heparin and other factors associated with complications of peripherally inserted central venous catheters in neonates. J Perinatol 32, 856–860 (2012). https://doi.org/10.1038/jp.2011.205
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2011.205
Keywords
This article is cited by
-
A nurse-inserted peripherally inserted central catheter program in general pediatrics: a single-center experience
BMC Pediatrics (2023)
-
Charakteristika und klinische Manifestation katheterassoziierter Thrombosen bei Frühgeborenen
Monatsschrift Kinderheilkunde (2022)
-
Strategies to prevent drug incompatibility during simultaneous multi-drug infusion in intensive care units: a literature review
European Journal of Clinical Pharmacology (2021)
-
Dwell times and risk of non-elective removal of 1-French peripherally inserted central catheters according to catheter tip position in very preterm infants
European Journal of Pediatrics (2017)
-
Peripherally inserted central catheter tip position and risk of associated complications in neonates
Journal of Perinatology (2013)