Abstract
Objective:
Candida infections cause substantial morbidity and mortality in neonates. Persistent candidemia has not been associated with increased risk of mortality compared with candidemia of shorter duration. This study sought to determine whether persistent candidemia was associated with increased length of hospitalization or mortality in neonates.
Study Design:
A chart review was conducted of neonates with Candida bloodstream infections (n=37). Demographic, laboratory, pharmacy, nutrition and discharge data were abstracted. Contingency table analysis and logistic regression were used to analyze variables associated with persistent candidemia and mortality. The relationship between length of hospitalization and persistent candidemia was assessed with k-sample equality of medians test.
Result:
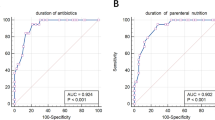
Nine patients (24%) had persistent candidemia. Increased time between blood culture draw and initial antifungal therapy was associated with increased incidence of persistent candidemia (P=0.03). Five patients (14%) died before hospital discharge; however, no deaths were attributed to persistent candidemia. Length of hospitalization was not increased with persistent candidemia. A decrease in the ratio of enteral feeding days to hyperalimentation days before collection of the first positive blood culture was significantly associated with an increase in all-cause mortality (P=0.03) and death attributed to candidemia (P=0.04). The risk of all-cause mortality decreased with a history of receiving any enteral feedings before the first positive blood culture (P=0.04), as did death attributed to candidemia (P=0.02).
Conclusion:
A duration of >1 day between the time of blood culture and the initial dose of systemic antifungal treatment places neonates at increased risk for developing persistent candidemia; however, this is not associated with increased mortality.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Stoll BJ, Hansen N, Fanaroff AA, Wright LL, Carlo WA, Ehrenkranz RA et al. Late-onset sepsis in very low birth weight neonates: the experience of the NICHD Neonatal Research Network. Pediatrics 2002; 110 (2 Part 1): 285–291.
Saiman L, Ludington E, Pfaller M, Rangel-Frausto S, Wiblin RT, Dawson J et al. Risk factors for candidemia in neonatal intensive care Unit patients. The National Epidemiology of Mycosis Survey study group. Pediatr Infect Dis J 2000; 19 (4): 319–324.
Benjamin Jr DK, Stoll BJ, Fanaroff AA, McDonald SA, Oh W, Higgins RD et al. Neonatal candidiasis among extremely low birth weight infants: risk factors, mortality rates, and neurodevelopmental outcomes at 18 to 22 months. Pediatrics 2006; 117 (1): 84–92.
Smith PB, Morgan J, Benjamin JD, Fridkin SK, Sanza LT, Harrison LH et al. Excess costs of hospital care associated with neonatal candidemia. Pediatr Infect Dis J 2007; 26 (3): 197–200.
Levy I, Shalit I, Askenazi S, Klinger G, Sirota L, Linder N . Duration and outcome of persistent candidaemia in newborn infants. Mycoses 2006; 49 (3): 197–201.
Chapman RL, Faix RG . Persistently positive cultures and outcome in invasive neonatal candidiasis. Pediatr Infect Dis J 2000; 19 (9): 822–827.
Natarajan G, Lulic-Botica M, Aranda JV . Refractory neonatal candidemia and high-dose micafungin pharmacotherapy. J Perinatol 2009; 29 (11): 738–743.
Pappas PG, Kauffman CA, Andes D, Benjamin Jr DK, Calandra TF, Edwards Jr JE et al. Clinical practice guidelines for the management of candidiasis: 2009 update by the Infectious Diseases Society of America. Clin Infect Dis 2009; 48 (5): 503–535.
Procianoy RS, Eneas MV, Silveira RC . Empiric guidelines for treatment of Candida infection in high-risk neonates. Eur J Pediatr 2006; 165 (6): 422–423.
Benjamin Jr DK, Stoll BJ, Gantz MG, Walsh MC, Sanchez PJ, Das A et al. Neonatal candidiasis: epidemiology, risk factors, and clinical judgment. Pediatrics 2010; 126 (4): e865–e873.
Weese-Mayer DE, Fondriest DW, Brouillette RT, Shulman ST . Risk factors associated with candidemia in the neonatal intensive care unit: a case-control study. Pediatr Infect Dis J 1987; 6 (2): 190–196.
Acknowledgements
We would like to thank the Wichita Medical Research & Educational Foundation (WMREF) (Wichita, Kansas, USA) for the grant for data collection for this study. WMREF had no role in the study design, data collection, statistical analysis, interpretation of results, manuscript preparation or decision to submit the manuscript for publication. We would also like to thank Jared Shaw and Paula Delmore for assisting with database interrogation and data collection. Thanks to Cari Schmidt for facilitating the IRB and grant applications.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
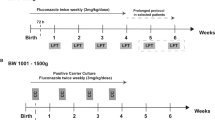
Dr Bloom was a site investigator and Dr Wittler is a contracted follow-up physician for the Duke Clinical Research Institute's Prophylactic Fluconazole Study.
Rights and permissions
About this article
Cite this article
Robinson, J., Pham, H., Bloom, B. et al. Risk factors for persistent candidemia infection in a neonatal intensive care unit and its effect on mortality and length of hospitalization. J Perinatol 32, 621–625 (2012). https://doi.org/10.1038/jp.2011.162
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2011.162
Keywords
This article is cited by
-
Epidemiology, antifungal susceptibility, risk factors, and mortality of persistent candidemia in adult patients in China: a 6-year multicenter retrospective study
BMC Infectious Diseases (2023)
-
Persistent candidemia in very low birth weight neonates: risk factors and clinical significance
BMC Infectious Diseases (2018)