Abstract
Objective:
To assess the effectiveness of liver length measurement in predicting hemoglobin (Hb) Bart's disease among fetuses at risk at mid-pregnancy.
Study Design:
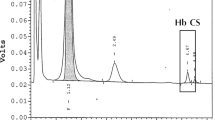
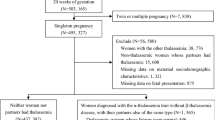
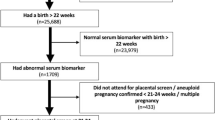
Pregnant women at risk of fetal Hb Bart's disease at 18 to 22 weeks of gestation were enrolled in the study. All of them underwent liver length measurement just before cordocentesis for fetal blood analysis. The final diagnosis used as a gold standard was based on fetal Hb typing using high-performance liquid chromatography.
Result:
A total of 334 pregnant women were recruited into the study. The prevalence of fetal Hb Bart's disease was 26.1% (87 of 334 fetuses). The sensitivity, specificity, as well as positive and negative predictive values of liver length in the prediction of affected fetuses were 71.3, 95.5, 84.9 and 90.4%, respectively. Overall, 24 fetuses (27.6%) had some degree of early hydrops fetalis. Of these, 20 had hepatomegaly as well.
Conclusion:
Liver length measurements at mid-pregnancy may be helpful in predicting affected fetuses among pregnancies at risk. Normal liver length measurement is associated with a very low risk of the disease. This information may help couples decide on whether to opt for either invasive diagnosis or a noninvasive approach, especially when used as an adjunct to other tests.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Ko TM, Hsieh FJ, Hsu PM, Lee TY . Molecular characterization of severe alpha-thalassemias causing hydrops fetalis in Taiwan. Am J Med Genet 1991; 39 (3): 317–320.
Lemmens-Zygulska M, Eigel A, Helbig B, Sanguansermsri T, Horst J, Flatz G . Prevalence of alpha-thalassemias in northern Thailand. Hum Genet 1996; 98 (3): 345–347.
Liang ST, Wong VC, So WW, Ma HK, Chan V, Todd D . Homozygous alpha-thalassaemia: clinical presentation, diagnosis and management. A review of 46 cases. Br J Obstet Gynaecol 1985; 92 (7): 680–684.
Tongsong T, Wanapirak C, Sirichotiyakul S, Chanprapaph P . Sonographic markers of hemoglobin Bart disease at midpregnancy. J Ultrasound Med 2004; 23 (1): 49–55.
Leung KY, Liao C, Li QM, Ma SY, Tang MH, Lee CP et al. A new strategy for prenatal diagnosis of homozygous alpha(0)-thalassemia. Ultrasound Obstet Gynecol 2006; 28 (2): 173–177.
Lam YH, Ghosh A, Tang MH, Lee CP, Sin SY . Second-trimester hydrops fetalis in pregnancies affected by homozygous alpha-thalassaemia-1. Prenat Diagn 1997; 17 (3): 267–269.
Lam YH, Tang MH, Lee CP, Tse HY . Prenatal ultrasonographic prediction of homozygous type 1 alpha-thalassemia at 12 to 13 weeks of gestation. Am J Obstet Gynecol 1999; 180 (1 Part 1): 148–150.
Roberts AB, Mitchell JM, Pattison NS . Fetal liver length in normal and isoimmunized pregnancies. Am J Obstet Gynecol 1989; 161 (1): 42–46.
Vintzileos AM, Campbell WA, Storlazzi E, Mirochnick MH, Escoto DT, Nochimson DJ . Fetal liver ultrasound measurements in isoimmunized pregnancies. Obstet Gynecol 1986; 68 (2): 162–167.
Tongsong T, Wanapirak C, Srisomboon J, Piyamongkol W, Sirichotiyakul S . Antenatal sonographic features of 100 alpha-thalassemia hydrops fetalis fetuses. J Clin Ultrasound 1996; 24 (2): 73–77.
Vintzileos AM, Neckles S, Campbell WA, Andreoli Jr JW, Kaplan BM, Nochimson DJ . Fetal liver ultrasound measurements during normal pregnancy. Obstet Gynecol 1985; 66 (4): 477–480.
Srisupundit K, Piyamongkol W, Tongsong T . Identification of fetuses with hemoglobin Bart's disease using middle cerebral artery peak systolic velocity. Ultrasound Obstet Gynecol 2009; 33 (6): 694–697.
Acknowledgements
We thank the Thailand Research Fund (TRF) and the Commission on Higher Education (CHE) of Thailand, as a part of TRF Senior Research Scholar 2007 for financially supporting the conduct of this research (grant no. RTA5080011).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Luewan, S., Tongprasert, F., Piyamongkol, W. et al. Fetal liver length measurement at mid-pregnancy among fetuses at risk as a predictor of hemoglobin Bart's disease. J Perinatol 31, 157–160 (2011). https://doi.org/10.1038/jp.2010.84
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2010.84