Abstract
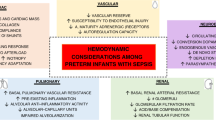
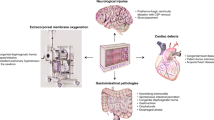
Continuous, reliable and real-time assessment of major determinants of cardiovascular function in preterm and term neonates has long been an elusive aim in neonatal medicine. Accordingly, aside from continuous assessment of heart rate, blood pressure and arterial oxygen saturation, bedside monitoring of major determinants of cardiovascular function of significant clinical relevance such as cardiac output, systemic vascular resistance, organ blood flow distribution and tissue oxygen delivery and coupling has only recently become available. Without obtaining reliable information on the changes in and interactions among these parameters in the neonatal patient population during postnatal transition and later in the neonatal period, development of effective and less harmful treatment approaches to cardiovascular compromise is not possible. This paper briefly reviews the recent advances in our understanding of developmental cardiovascular physiology and discusses the methods of bedside assessment of cardiovascular function in general and organ perfusion, tissue oxygen delivery and brain function in particular in preterm and term neonates. The importance of real-time data collection and the need for meticulous validation of the methods recently introduced in the assessment of neonatal cardiovascular function such as echocardiography, electrical impedance cardiometry, near infrared spectroscopy, visible light and laser-Doppler technology are emphasized. A clear understanding of the accuracy, feasibility, reliability and limitations of these methods through thorough validation will result in the most appropriate usage of these methods in clinical research and patient care.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Noori S, Seri I . Etiology, pathophysiology and phases of neonatal shock. In: Kleinman C, Seri I (eds). Neonatology Questions and Controversies: Hemodynamics and Cardiology. Saunders/Elsevier: Philadelphia, 2008, pp 3–18.
Noori S, Stavroudis TA, Seri I . Systemic and cerebral hemodynamics during the transitional period after premature birth. Clin Perinatol 2009; 36: 723–736.
Evans N, Seri I . Cardiovascular compromise in the newborn infant. In: Taeusch HW, Ballard RA, Gleason CA (eds). Avery's Diseases of the Newborn, 8th edn, WB Saunders: Philadelphia, 2004, pp 398–409.
Miall-Allen VM, De Vries LS, Whitelaw AGL . Mean arterial blood pressure and neonatal cerebral lesions. Arch Dis Child 1987; 62: 1068–1069.
Watkins AM, West CR, Cooke RW . Blood pressure and cerebral hemorrhage and ischemia in very low birth weight infants. Early Hum Dev 1989; 19: 103–110.
Bada HS, Korones SB, Perry EH, Arheart KL, Ray JD, Pourcyrous M et al. Mean arterial blood pressure changes in premature infants and those at risk for intraventricular hemorrhage. J Pediatr 1990; 117: 607–614.
Goldstein RF, Thompson RJ, Oehler JM, Brazy JE . Influence of acidosis, hypoxaemia, and hypotension on neurodevelopmental outcome in very low birth weight infants. Pediatrics 1995; 95: 238–243.
Kluckow M, Evans N . Low superior vena cava flow and intraventricular hemorrhage in preterm infants. Arch Dis Child Fetal Neonatal Ed 2000; 82: F188–F194.
Hunt RW, Evans N, Rieger I, Kluckow M . Low superior vena cava flow and neurodevelopment at 3 years in very preterm infants. J Pediatr 2004; 145: 588–592.
Fanaroff JM, Wilson-Costello DE, Newman NS, Montpetite MM, Fanaroff AA . Treated hypotension is associated with neonatal morbidity and hearing loss in extremely low birth weight infants. Pediatrics 2006; 117: 1131–1135.
Pellicer A, del Carmen Bravo M, Madero R, Salas S, Quero J, Cabañas F . Early systemic hypotension and vasopressor support in low birth weight infants: impact on neurodevelopment. Pediatrics 2009; 123: 1369–1376.
Greisen G . Use of organ blood flow assessment in the diagnosis of neonatal shock. In: Kleinman C, Seri I (eds). Neonatology Questions and Controversies: Hemodynamics and Cardiology. Saunders/Elsevier: Philadelphia, 2008, pp 69–82.
Kluckow M, Seri I, Evans N . Functional echocardiography—an emerging clinical tool for the neonatologist. Medical Progress Article J Pediatr 2007; 150: 125–130.
Victor S, Weindling M . Near infrared spectroscopy and its use for the assessment of tissue perfusion in the neonate. In: Kleinman C, Seri I (eds). Neonatology Questions and Controversies: Hemodynamics and Cardiology. Saunders/Elsevier: Philadelphia, 2008, pp 110–132.
Barrington KJ, Dempsey EM . Cardiovascular support in the preterm: treatments in search of indications. J Pediatr 2006; 148: 289–291.
Hernandez MJ, Hawkins RA, Brennan RW . Sympathetic control of regional cerebral blood flow in the asphyxiated newborn dog. In: Heistad DD, Marcus ML (eds). Cerebral Blood Flow, Effects of Nerves and Neurotransmitters. Elsevier: New York, 1982, pp 359–366.
Ashwal S, Dale PS, Longo LD . Regional cerebral blood flow: studies in the fetal lamb during hypoxia, hypercapnia, acidosis, and hypotension. Pediatr Res 1984; 18: 1309–1316.
Brown DW, Picot PA, Naeini JG, Springett R, Delpy DT, Lee TY . Quantitative near infrared spectroscopy measurement of cerebral hemodynamics in newborn piglets. Pediatr Res 2002; 51: 564–570.
Müller T, Löhle M, Schubert H, Bauer R, Wicher C, Antonow-Schlorke I et al. Developmental changes in cerebral autoregulatory capacity in the fetal sheep parietal cortex. J Physiol 2002; 539 (Part 3): 957–967.
Tibby SM, Ian A, Murdoch IA . Measurement of cardiac output and tissue perfusion. Cur Opinion Pediatr 2002; 14: 303–309.
Dempsey EM, Alhazzani F, Barrington KJ . Permissive hypotension in the extremely low birth weight infant with signs of good perfusion. Arch Dis Child Fetal Neonatal Ed 2009; 94: F241–F244.
Seri I . Circulatory support of the sick newborn infant. Semin Neonatol 2001; 6: 85–95.
Nagdyman N, Ewert P, Peters BRN, Miera O, Fleck T, Berger F . Comparison of different near-infrared spectroscopic cerebral oxygenation indices with central venous and jugular venous oxygenation saturation in children. Pediatr Anesth 2008; 18: 160–166.
van Bel F, Lemmers P, Naulaers G . Monitoring neonatal regional cerebral oxygen saturation in clinical practice: value and pitfalls. Neonatology 2008; 94: 237–244.
Wong FY, Barfield CP, Horne RSC, Walker AM . Dopamine therapy promotes cerebral flow-metabolism coupling in preterm infants. Intensive Care Med 2009; 35: 1777–1782.
Krimer LS, Muly EC, Williams GV, Goldman-Rakic PS . Dopaminergic regulation of cerebral cortical microcirculation. Nat Neurosci 1998; 1: 286–289.
Kissack CM, Garr R, Wardle SP, Weindling AM . Postnatal changes in cerebral oxygen extraction in the preterm infant are associated with intraventricular hemorrhage and hemorrhagic parenchymal infarction but not periventricular leukomalacia. Pediatr Res 2004; 56: 111–116.
Meek JH, Tyszczuk L, Elwell CE, Wyatt JS . Low cerebral blood flow is a risk factor for severe intraventricular hemorrhage. Arch Dis Child Fetal Neonatal Ed 1999; 81: F15–F18.
Greisen G . Autoregulation of vital and non-vital organ blood flow in the preterm and term neonate. In: Kleinman C, Seri I (eds). Neonatology Questions and Controversies: Hemodynamics and Cardiology. Saunders/Elsevier: Philadelphia, 2008, pp 19–38.
Borzage TM, Nelson M, Seri I, Blüml S . Simultaneous BOLD and NIRS signal correlation during hypoxia. Annual PAS/SPR Meeting 2010; Vancouver, Abstract.
Noori S, Drabu B, Seri I . Continuous non-invasive cardiac output measurements in the neonate by electrical cardiometry: a comparison with echocardiography. Annual PAS/SPR Meeting 2010; Vancouver, Abstract.
Soleymani S, Cayabyab R, Borzage TM, Seri I . Comparison between charted and continuously recorded vital signs and hemodynamic data. Annual PAS/SPR Meeting 2010; Vancouver, Abstract.
Norozi K, Beck C, Osthaus WA, Wille I, Wessel A, Bertram H . Electrical velocimetry for measuring cardiac output in children with congenital heart disease. Br J Anaesth 2008; 100: 88–94.
Amir G, Ramamoorthy C, Riemer RK, Davis CR, Hanley FL, Reddy VM . Visual light spectroscopy reflects flow-related changes in brain oxygenation during regional low-flow perfusion and deep hypothermic circulatory arrest. J Thorac Cardiovasc Surg 2006; 132: 1307–1313.
Nuntnarumit P, Yang W, Bada-Ellzey HS . Blood pressure measurements in the newborn. Clin Perinatol 1999; 26: 981–996.
Darnall RA . Blood pressure monitoring. In: Brans Y, Hay WJ, (eds). Physiological Monitoring and Instrument Diagnosis in Perinatal and Neonatal Medicine. Cambridge University Press: Cambridge, 1995, pp 246–266.
Engle WD . Definition of normal blood pressure range: the elusive target. In: Kleinman C, Seri I (eds). Neonatology Questions and Controversies: Hemodynamics and Cardiology. Saunders/Elsevier: Philadelphia, 2008, pp 39–68.
Shiao SY, Ou CN . Validation of oxygen saturation monitoring in neonates. Am J Crit Care 2007; 16: 168–178.
Kluckow M, Seri I . Clinical presentations of neonatal shock: the VLBW infant during the first postnatal day. In: Kleinman C, Seri I (eds). Neonatology Questions and Controversies: Hemodynamics and Cardiology. Saunders/Elsevier: Philadelphia, 2008, pp 147–177.
Stark MJ, Clifton VL, Wright IMR . Carbon monoxide is a significant mediator of cardiovascular status following preterm birth. Pediatrics 2009; 124: 277–284.
Hiedl S, Schwepcke A, Weber F, Genzel-Boroviczeny O . Microcirculation in preterm infants: profound effects of patent ductus arteriosus. J Pediatr 2010; 156: 191–196.
Rennie JM, Chorley G, Boylan GB, Pressler R, Nguyen Y, Hooper R . Non-expert use of the cerebral function monitor for neonatal seizure detection. Arch Dis Child Fetal Neonatal Ed 2004; 89: F37–F40.
Toet MC, Lemmers PMA, van Schelven LJ, van Bel F . Cerebral oxygenation and electrical activity after birth asphyxia: their relation to outcome. Pediatrics 2006; 117: 333–339.
West CR, Groves AM, Williams CE, Harding JE, Skinner JR, Kuschel CA et al. Early low cardiac output is associated with compromised electroencephalographic activity in very preterm infants. Pediatr Res 2006; 59: 610–615.
Acknowledgements
Dr Seri was a member of the Scientific Advisory Committee on Surfactant Use at Dey LP (2004–2009) and has received grant support for clinical research from Somanetics (2009–2010). This paper resulted from the Evidence vs Experience in Neonatal Practices conference, 19–20 June 2009, sponsored by Dey LP.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This paper resulted from the Evidence vs Experience in Neonatal Practices conference, 19 to 20 June 2009, sponsored by Dey, LP.
Rights and permissions
About this article
Cite this article
Soleymani, S., Borzage, M. & Seri, I. Hemodynamic monitoring in neonates: advances and challenges. J Perinatol 30 (Suppl 1), S38–S45 (2010). https://doi.org/10.1038/jp.2010.101
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2010.101
Keywords
This article is cited by
-
Inter-observer variability of right ventricular output measurement in newborn infants: an observational study
The International Journal of Cardiovascular Imaging (2024)
-
Echocardiography-directed management of hemodynamically unstable neonates in tertiary care hospitals
Egyptian Pediatric Association Gazette (2023)
-
Intraventricular hemorrhage prediction in premature neonates in the era of hemodynamics monitoring: a prospective cohort study
European Journal of Pediatrics (2022)
-
Bioreactance-derived haemodynamic parameters in the transitional phase in preterm neonates: a longitudinal study
Journal of Clinical Monitoring and Computing (2022)
-
The effect of enteral bolus feeding on regional intestinal oxygen saturation in preterm infants is age-dependent: a longitudinal observational study
BMC Pediatrics (2019)