Abstract
Objective:
To identify women who are most likely to benefit from primary prevention strategies for postpartum hemorrhage (PPH).
Study Design:
In a retrospective patient cohort, we applied recursive partitioning algorithms to identify the most discriminant risk factors and their interactions, and calculated the ‘number needed to treat’ to prevent a single case of PPH (estimated blood loss >1000 ml).
Result:
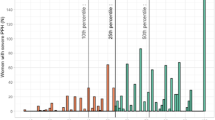
By delivery category, the highest risk groups with ‘number needed to treat’ ranging from 4 to 7 were: (1) vaginal delivery (PPH=0.7% of 16 218)—macrosomia with gestational diabetes and manual removal of the placenta; (2) primary cesarean (PPH=18.7% of 2696)—macrosomia and multiparity; and (3) repeat cesarean (PPH=16.0% of 1832)—uterine incision other than low transverse and failed vaginal birth after cesarean.
Conclusion:
Clinical profiles that identify women at risk for PPH can provide a foundation for the development of primary prevention strategies.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Chang J, Elam-Evans LD, Berg CJ, Herndon J, Flowers L, Seed KA et al. Pregnancy-related mortality surveillance—United States, 1991–1999. MMWR Surveill Summ 2003; 52: 1–8.
Gilstrap III LC, Ramin SM . Postpartum hemorrhage. Clin Obstet Gynecol 1994; 37 (4): 824–830.
Bonnar J . Massive obstetric haemorrhage. Baillieres Best Pract Res Clin Obstet Gynaecol 2000; 14: 1–18.
Prendiville WJ, Elbourne D, McDonald S . Active versus expectant management in the third stage of labour. Cochrane Database Syst Rev 2000; (3): CD000007. doi:10.1002/14651858.CD000007.
Gülmezoglu AM, Forna F, Villar J, Hofmeyr GJ . Prostaglandins for prevention of postpartum haemorrhage. Cochrane Database Syst Rev 2007; (3): CD000494. doi:10.1002/14651858.CD000494.pub3.
McDonald S, Abbott JM, Higgins SP . Prophylactic ergometrine-oxytocin versus oxytocin for the third stage of labour. Cochrane Database Syst Rev 2004; (1): CD000201. doi:10.1002/14651858.CD000201.pub2.
Burtelow M, Riley E, Druzin M, Fontaine M, Viele M, Goodnough LT . How we treat: management of life-threatening primary postpartum hemorrhage with a standardized massive transfusion protocol. Transfusion 2007; 47 (9): 1564–1572.
Mousa HA, Walkinshaw S . Major postpartum haemorrhage. Curr Opin Obstet Gynecol 2001; 13 (6): 595–603.
World Health Organization. The prevention and management of postpartum haemorrhage. WHO report of technical working group. World Health Organization: Geneva, 1990 Report No. WHO/MCH/90.7.
Technical Working Group. Care in normal birth: a practical guide. World Health Organization: Geneva, 1996 pp 31.
Technical Working Group, Department of Making Pregnancy Safer. WHO Recommendations for the Prevention of Postpartum Haemorrhage. World Health Organization: Geneva, 2007 pp 17.
Burchell RC . Postpartum haemorrhage. In: Quilligan ES (ed). Curr Ther Obstet Gynaecol. WB Saunders: Philadelphia, PA, 1980.
American College of Obstetricians and Gynecologists. ACOG Practice Bulletin: Clinical Management Guidelines for Obstetrician–Gynecologists Number 76, October 2006: postpartum hemorrhage. Obstet Gynecol 2006; 108: 1039–1047.
Waterstone M, Bewley S, Wolfe C . Incidence and predictors of severe obstetric morbidity: case-control study. BMJ 2001; 322: 1089–1094.
American College of Obstetricians and Gynecologists. Operative Vaginal Delivery. American College of Obstetricians and Gynecologists: Washington, DC, 2000 ACOG practice bulletin no. 17.
Gregory KD, Curtin SC, Taffel SM, Notzon FC . Changes in indications for cesarean delivery: United States, 1985 and 1994. Am J Public Health 1998; 88 (9): 1384–1387.
Breiman L, Friedman JH, Olshen RA, Stone CJ . Classification and Regression Trees. Wadsworth International Group: Belmont, CA, 1984.
Sands K, Vineyard G, Livingston J, Christiansen C, Platt R . Efficient identification of post-discharge surgical site infections; use of automated pharmacy dispensing information, administrative data, and medical record information. J Infect Dis 1999; 179: 434–441.
Friedman EA . Labor. Clinical evaluation and management. Appleton-Century-Crofts: New York, 1967.
Lavender T, Alfirevic A, Walkinshaw S . Effect of different partogram action lines on birth outcomes: a randomized controlled trial. Obstet Gynecol 2006; 108: 295–302.
Lavender T, Alfirevic A, Walkinshaw S . Partogram action line study: a randomized trial. Br J Obstet Gynecol 1998; 105: 976–980.
Acknowledgements
Financial support for this work was provided by the California Department of Health Services Maternal and Child Health Branch (Contract No. 01-15166).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lu, M., Korst, L., Fridman, M. et al. Identifying women most likely to benefit from prevention strategies for postpartum hemorrhage. J Perinatol 29, 422–427 (2009). https://doi.org/10.1038/jp.2009.2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2009.2
Keywords
This article is cited by
-
Intrapartum cesarean delivery in nulliparas: risk factors compared by two analytical approaches
Journal of Perinatology (2015)