Abstract
Objective:
To examine the effect of regionalization of care on outcomes of neonates with congenital diaphragmatic hernia (CDH).
Study Design:
We analyzed the National Inpatient Sample and the ‘Kids’ database for the years 1997 to 2004. Infants with CDH were grouped based on whether they underwent surgical repair at the hospital of birth, or at another facility. Groups were compared using chi-square, t-test and logistic regression.
Result:
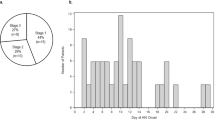
A total of 2140 infants were included: 41% were females, 42% were Caucasians, 48% were transported, 20% reported the use of extracorporeal membrane oxygenation (ECMO)and 33% died. Only 79% underwent operative repair, in which 85% survived after surgery. Survival among operated patients who used ECMO was 40%. Transported infants used more ECMO than non-transported ones (25 vs 15%; adjusted odds ratio (OR) 1.46; confidence interval 1.1 to 1.9, P=0.007), and had higher mortality after surgery (16 vs 13%; adjusted OR 1.46; confidence interval 1.1 to 2, P=0.02).
Conclusion:
The utilization of neonatal transport of CDH patients is associated with increased mortality and increased need for ECMO. This study supports the need for regionalization of care, and favors maternal transport before delivery of CDH newborns.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Doyle NM, Lally KP . The CDH Study Group and advances in the clinical care of the patient with congenital diaphragmatic hernia. Semin Perinatol 2004; 28: 174–184.
Chen C, Jeruss S, Chapman JS, Terrin N, Tighiouart H, Glassman E et al. Long-term functional impact of congenital diaphragmatic hernia repair in children. Pediatr Surg 2007; 42: 657–665.
Javid PJ, Jaksic T, Skasgard ED, Lee S, Canadian Neonatal Network. Survival rate in congenital diaphragmatic hernia: the experience in Canadian Neonatal Network. J Pediatr Surg 2004; 39: 657–660.
Boloker J, Bateman DA, Wung JT, Stolar CJ . Congenital diaphragmatic hernia in 120 infants treated consecutively with permissive hypercapnea/ spontaneous respiration/elective repair. J Pediatr Surg 2002; 3: 357–366.
Bagolan P, Casaccia G, Crescenzi F, Nahom A, Trucchi A, Giorlandino C . Impact of current treatment protocol on outcome of high-risk congenital diaphragmatic hernia. J Pediatr Surg 2004; 39: 313–318.
Sakai H, Tamura M, Hosokowa Y, Bryan AC, Barker GA, Bohn DJ . Effect of surgical repair on respiratory mechanics in congenital diaphragmatic hernia. J Pediatr 1987; 111: 432–438.
Nakayama DK, Motoyama EK, Tagge EM . Effect of preoperative stabilization on respiratory system compliance and outcome in newborn infants with congenital diaphragmatic hernia. J Pediatr 1991; 118: 793–799.
Wung JT, Sahni R, Moffitt St, lipsitz E, Stolar CJ . Congenital diaphragmatic hernia: survival treated with very delayed surgery, spontaneous respiration, and no chest tube. J Pediatr Surg 1995; 30: 406–409.
Heiss K, Manning P, Oldham KT, Coran Ag, Polley Jr TZ, Wesley JR et al. Reversal of mortality for congenital diaphragmatic hernia with ECMO. Ann Surg 1989; 209: 225–230.
vd Staak FHJM, de Haan AFJ, Geven WB, Doesburg WH, Festen C . Improving survival for patients with high-risk congenital diaphragmatic hernia by using extracorporeal membrane oxygenation. J Pediatr Surg 1995; 30: 1463–1467.
McGahren ED, Mallik K, Rodgers B . Neurological outcome is diminished in survivors of congenital diaphragmatic hernia requiring extracorporeal membrane oxygenation. J Pediatr Surg 1997; 32: 1216–1220.
Bennett CC, Johnson A, Field DJ, Elbourne D, UK Collaborative ECMO Trial Group. UK collaborative randomized trial of neonatal extracorporeal membrane oxygenation: follow up to age 4 years. Lancet 2001; 357: 1094–1096.
Rasheed A, Tindall S, Cueny DL, Klein MD, Delaney-Black V . Neurodevelopmental outcome after congenital diaphragmatic hernia: extracorporeal membrane oxygenation before and after surgery. J Pediatr Surg 2001; 36: 539–544.
Phibbs CS, Baker LC, Caughey AB, Danielsen B, Schmitt SK, Phibbs RH . Level and volume of neonatal intensive care and mortality in very-low-birth-weight infants. N Engl J Med 2007; 356: 2165–2175.
Paneth N, Kiely JL, Susser M . Age at death used to assess the effect of interhospital transfer of newborns. Pediatrics 1984; 73: 854–861.
Logan JW, Rice HE, Goldberg RN, Cotton CM . Congenital diaphragmatic hernia: a systematic review and summary of best-evidence practice strategies. J Perinatol 2007; 27: 535–549.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Aly, H., Bianco-Batlles, D., Mohamed, M. et al. Mortality in infants with congenital diaphragmatic hernia: a study of the United States National Database. J Perinatol 30, 553–557 (2010). https://doi.org/10.1038/jp.2009.194
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2009.194
Keywords
This article is cited by
-
Survival of infants with congenital diaphragmatic hernia in California: impact of hospital, clinical, and sociodemographic factors
Journal of Perinatology (2020)
-
Survival trends and outcomes among preterm infants with congenital diaphragmatic hernia
Journal of Perinatology (2020)
-
Congenital diaphragmatic hernia: current management strategies from antenatal diagnosis to long-term follow-up
Pediatric Surgery International (2020)
-
Relationship between volume and outcome for congenital diaphragmatic hernia: a systematic review protocol
Systematic Reviews (2018)
-
Response to pulmonary vasodilators in infants with congenital diaphragmatic hernia
Pediatric Surgery International (2018)