Abstract
Objective:
To determine the effects of a postural support protocol on the physiological and behavioral stability of preterm infants while undergoing a diaper change.
Study Design:
Forty-seven newborns having a birth weight ⩽2000 g and gestational age ⩽35 weeks were included in this randomized, crossover clinical trial in a Neonatology Intensive Care Unit. The infants were observed as his or her own control and evaluated with and without the use of the proposed intervention, which was positioning the baby in a nest produced with rolled-up towels. During the observations, as control, the care model used by the unit was considered.
Result:
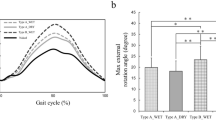
All babies displayed increased distress and pain scores during diaper changes. This was significantly less for babies nested compared with non-nested babies (P<0.0001).
Conclusion:
Diaper change is a distressing procedure for preterm infants. Providing postural support during diaper changes reduces the signs of distress and pain.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Als H, Lawhon G, Brown E, Gibes R, Duffy FH, McAnulty G et al. Individualized behavioral and environmental care for the very low birth weight preterm infant at high risk for bronchopulmonary dysplasia: neonatal intensive care unit and developmental outcome. Pediatrics 1986; 78 (6): 1123–1132.
Comaru T, Miura E . Postural Support in newborn preterm infants. Pediatr Crit Care 2007; 8: A334.
Als H . Neurobehavioral development of the preterm infant. In: Fanaroff AA, Martin RJ (eds). Neonatal-Perinatal Medicine. (vol2), Mosby Co: St Louis (MO), 1997, pp 964–989.
Liu WF, Laudert S, Perkins B, MacMillian-York E, Martin S, Graven S . The development of potentially better practices to support the neurodevelopment of infants in the NICU. J Perinatol 2007; 27 (Suppl 2): S48–S74.
Sizun J, Ansquer H, Browne J, Tordjman S, Morin JF . Developmental care decreases physiologic and behavioral pain expression in preterm neonates. J Pain 2002; 3 (6): 446–450.
Stevens B, Gibbins S . Clinical utility and clinical significance in the assessment and management of pain in vulnerable infants. Clin Perinatol 2002; 29 (3): 459–468.
Symington A, Pinelli J . Developmental care for promoting development and preventing morbidity in preterm infants (Cochrane Review). In: The Cochrane Library, Issue 4, 2008. Oxford: update software, available in www.cochrane.org.
Ministério da Saúde. Secretaria de Políticas de Saúde, Brasil, Ministério da Saúde, Manual do Curso. Atenção Humanizada ao Recém-Nascido de Baixo Peso—Método Canguru/Secretaria de Políticas da Saúde, Área Técnica da Saúde da Criança: Brasília,, 2001.
Holsti L, Grunau RE, Oberlander TF, Whitfiels MF . Specific newborn individualized developmental care and assessment program movements are associated with acute pain in preterm infants in the neonatal intensive care unit. Pediatrics 2004; 114 (1): 65–72.
Grunau RE, Oberlander T, Holsti L, Whitfield MF . Bedside application of the neonatal facial coding system in pain assessment of premature neonates. Pain 1998; 76 (3): 277–286.
Guinsburg RBR, Xavier RC . Are behavioral scales suitable for preterm and term neonatal pain assessment? Pediatr Res 1996; 119: 417–423.
Altman DG . Practical Statistics for Medical Research. Chapman and Hall: London (UK), 1994, pp 426–471.
Sweeney JK, Gutierrez T . Musculoskeletal implications of preterm infant positioning in the NICU. J Perinat Neonat Nurs 2002; 16 (1): 58–70.
Slevin M, Murphy JF, Daly L, O'Keefe M . Retinopathy of prematurity screening, stress related responses, the role of nesting. Br J Ophtalmol 1997; 81: 762–764.
Acknowledgements
This work was financially supported by the Research Support Fund (FIPE) of the Hospital de Clínicas in Porto Alegre and by a CNPq Scholarship.
Author information
Authors and Affiliations
Corresponding author
Additional information
The study was registered by no. 03279 in the Institutional Review Board IRB0000921.
Rights and permissions
About this article
Cite this article
Comaru, T., Miura, E. Postural support improves distress and pain during diaper change in preterm infants. J Perinatol 29, 504–507 (2009). https://doi.org/10.1038/jp.2009.13
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2009.13