Abstract
Background:
Iron delocalization or misregulation of iron metabolism may play a critical role in the pathology of hypoxic ischemic encephalopathy (HIE).
Objective:
To study iron metabolism and lipid peroxidation in newborn infants and to correlate non-protein-bound iron (NPBI) concentration with the severity of the post-asphyxial injury and subsequent short-term outcomes.
Study Design:
Concentrations of NPBI and malondialdehyde (MDA) in the serum and in the cerebrospinal fluid (CSF) were measured in eight healthy newborn infants and nine newborn infants suffering from moderately severe HIE. Short-term outcomes (death, survival with or without neurological abnormality) were noted at hospital discharge.
Result:
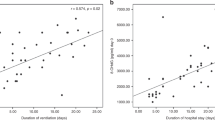
Serum and CSF concentrations of both NPBI and MDA were significantly increased in HIE infants when compared to controls. Serum iron was significantly increased and total iron binding capacity was significantly decreased in HIE infants compared to controls. Out of the nine HIE infants, four infants died and two infants survived with abnormal neurological findings at hospital discharge. These six infants with clinical sequels had significantly increased concentrations of NPBI in the serum and in the CSF; and increased concentrations of MDA in the CSF when compared to the other three who survived without short-term abnormalities.
Conclusion:
We conclude that hypoxia ischemia alters iron metabolism and lipid peroxidation in newborn infants; and that NPBI and MDA in the CSF are increased in infants with HIE. This study supports a role for iron in oxidative injury to the central nervous system after hypoxic ischemic insults.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Freeman JM, Nelson KB . Intrapartum asphyxia and cerebral palsy. Pediatrics 1988; 82: 240–249.
Volpe JJ . Neurology of the Newborn. 3rd ed WB Saunders: Philadelphia, 1995; pp 211–369.
Saugstad OD . Oxygen toxicity in the neonatal period. Acta Paediatr 1990; 79: 881–892.
Traystman RJ, Kirch JR, Koehler RC . Oxygen radical mechanisms of brain injury following ischemia and reperfusion. J Appl Physiol 1991; 71: 1185–1195.
Halliwell B . Reactive oxygen species and the central nervous system. J Neurochem 1992; 59: 1609–1623.
McCord J, Roy R, Schaffer S . Oxygen-derived free radicals in post-ischemic tissue injury. N Engl J Med 1985; 312: 159–163.
Reif DWX, Simmons RD . Nitric oxide mediates iron release from ferritin. Arch Biochem 1990; 283: 537–541.
Henry Y, Lepoivre M, Drapier JC, Ducrocq C, Boucher JL, Guissani A . EPR characterization of molecular targets for NO in mammalian cells and organelles. FASEB J 1993; 7: 1124–1134.
Anggard E . Nitric oxide: mediator, murderer, and medicine. Lancet 1994; 343: 1199–1206.
Dorrepaal CA, Berger HM, Benders MJ, van Zoeren-Grobben D, van de Bor M, van Bel F . Non-protein-bound iron in post-asphyxial reperfusion injury of the newborn. Pediatrics 1996; 98: 883–889.
Dorrepaal CA, van Bel F, Moison RM, Shadid M, van de Bor M, Steendijk P et al. Oxidative stress during post-hypoxic-ischemic reperfusion in the newborn lamb: the effect of nitric oxide synthesis inhibition. Pediatric Res 1997; 41: 321–326.
van Bel F, Shadid M, Moison RM, Dorrepaal CA, Fontijn J, Monteiro L et al. Effect of allopurinol on post-asphyxial free radical formation, cerebral hemodynamics, and electrical brain activity. Pediatrics 1998; 101: 185–193.
Yu T, Kui LQ, Ming QZ . Effect of asphyxia on non-protein-bound iron and lipid peroxidation in newborn infants. Dev Med Child Neurol 2003; 45: 24–27.
Georgieff MK . Iron in the brain: its role in development and injury. Neoreviews 2006; 6: 344–352.
Palmer C, Roberts RL, Bero C . Desferoxamine post treatment reduces ischemic brain injury in neonatal rats. Stroke 1994; 25: 1039–1045.
Groenendaal F, Shadid M, Mc Growan JE, Mishra OP, van Bel F . Effects of deferoxamine, a chelator of free iron, on Na+, K+ ATPase activity of cortical brain cell membrane during early reperfusion after hypoxia ischemia in newborn lambs. Pediatr Res 2000; 48: 560–564.
Ogihara T, Hirano K, Ogihara H, Misaki K, Hiroi M, Morinobu T et al. Non-protein-bound transition metals and hydroxyl radical generation in cerebrospinal fluid of newborn infants with hypoxic ischemic encephalopathy. Pediatr Res 2003; 53: 594–599.
Singh S, Hider RC, Porter JB . A simple method for calorimetric quantitation of non-transferrin-bound iron in serum. Biochem Trans 1989; 17: 697–698.
Zhang D, Okada S, Kawabata T, Yasuda T . An improved simple colorimetric method for quantitation of non-transferrin-bound iron in the serum. Biochem Mol Biol Int 1995; 35: 635–641.
Carter P . Spectrophotometric determination of serum iron at the submicrogram level with a new reagent (ferrozine). Anal Biochem 1971; 40: 450–458.
Ramsay WNM . The determination of the total-iron-binding capacity of serum. Clin Chem Acta 1957; 2: 221.
Ozaras R, Tahan V, Turkmen S, Talay E, Besirli K, Aydin S et al. Changes in malondialdehyde levels in bronchoalveolar fluid and serum by the treatment of asthma with inhaled steroid and β2 agonist. Respirology 2000; 5: 289–292.
Bromont C, Marie C, Bralet J . Increased lipid peroxidation in vulnerable brain regions after transient forebrain ischemia in rats. Stroke 1989; 20: 918–924.
Buonocore G, Perrone S, Longini M, Paffetti P, Vezzosi P, Gatti MG et al. Non protein bound iron as early predictive marker of neonatal brain damage. Brain 2003; 126: 1224–1230.
Buonocore G, Zani S, Sargentini I, Gioia D, Signorini C, Bracci R . Hypoxia-induced free iron release in the red cells of newborn infants. Acta Paediatr 1998; 87: 77–81.
Krause GS, Nayini NR, White BC, Hoenher TJ, Garritano AM, O'Neil BJ et al. Natural course of iron delocalization and lipid peroxidation during the first eight hours following a 15-min cardiac arrest in dogs. Ann Emerg Med 1987; 16: 1200–1205.
Chiao JJ, Kirschner RE, Fantini GA . Iron delocalization occurs during ischemia and persists on reoxygenation of skeletal muscle. J Lab Clin Med 1994; 124: 432–438.
Komara JS, Nayini NR, Bialick HA, Indrieri RJ, Evans AT, Garritano AM et al. Brain iron delocalization and lipid peroxidation following cardiac arrest. Ann Emerg Med 1986; 15: 384–389.
Siesjo BK . Acidosis and ischemic brain damage. Neurochem Pathol 1988; 9: 31–88.
Biemond P, Swaak AJ, Beindorff CM, Koster JF . Superoxide-dependent and independent mechanisms of iron mobilization from ferritin by xanthine oxidase. Biochem J 1986; 239: 169–173.
Gutteridqe JM . Ferrous ions detected in cerebrospinal fluid by using bleomycin and DNA damage. Clin Sci (Lond) 1992; 82: 315–320.
Gutteridqe JM . Iron and oxygen radicals in brain. Ann Neurol 1992; 32: S16–S21.
Hirano K, Morinobu T, Kim HS, Hiroi M, Ban R, Ogawa S et al. Blood transfusion increases radical promoting non-transferrin bound iron in preterm infants. Arch Dis Child Fetal Neonatal Ed 2001; 84: F188–F193.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shouman, B., Mesbah, A. & Aly, H. Iron metabolism and lipid peroxidation products in infants with hypoxic ischemic encephalopathy. J Perinatol 28, 487–491 (2008). https://doi.org/10.1038/jp.2008.22
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2008.22