Abstract
Objective:
To compare feeding tolerance, nutrient intake and growth in preterm infants (⩽32 weeks, ⩽1750 g) fed either a standard nonhydrolyzed whey–casein (nHWC) or a partially hydrolyzed whey (pHW) preterm infant formula.
Study Design:
In this double-blind randomized controlled trial infants were fed either formula for at least 3 weeks. Intake was monitored daily, serum chemistries and growth weekly. Data were analyzed using analysis of covariance.
Result:
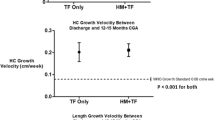
A total of 80 infants were enrolled, 72 completed the study. No differences were noted in demographic characteristics. No differences were detected in feeding tolerance, intakes (118±21 vs 119±14; nHWC vs pHW) or growth weight, 28±1.5 vs 28±1.6 g per day; length, 1.0±0.7 vs 1.0±0.6 cm per week; head circumference, 0.9±0.4 vs 1.0±0.44 cm per week). At the end of study, blood urea nitrogen (5.2±3.1 <6.7±2.3 mg per 100 ml, nHWC<pHW), total serum proteins (4.7±0.4 >4.4±0.5 g per 100 ml) and albumin (2.7±0.3 >2.6±0.4 g per 100 ml) differed.
Conclusion:
A pHW preterm infant formula was not associated with improved feeding tolerance, enteral intake or growth but differences in serum chemistries. These are unlikely to be clinically relevant because values were well within normal limits for preterm infants, whereas growth was identical in both groups and paralleled that ‘in utero’.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Embleton NE, Pang N, Cooke RJ . Postnatal malnutrition and growth retardation: an inevitable consequence of current recommendations in preterm infants? Pediatrics 2001; 107 (2): 270–273.
Mihatsch WA, Hogel J, Pohlandt F . Hydrolysed protein accelerates the gastrointestinal transport of formula in preterm infants. Acta Paediatr 2001; 90 (2): 196–198.
Mihatsch WA, Franz AR, Hogel J, Pohlandt F . Hydrolyzed protein accelerates feeding advancement in very low birth weight infants. Pediatrics 2002; 110 (6): 1199–1203.
Rigo J, Salle B, Picaud JC, Putet G, Senterre J . Nutritional evaluation of protein hydrolysate formulas. Eur J Clin Nutr 1995; 49: S26–S38.
Picaud JC, Rigo J, Normand S, Lapillonne A, Reygrobellet B, Claris O et al. Nutritional efficacy of preterm formula with a partially hydrolyzed protein source: a randomized pilot study. J Pediatr Gastroenterol Nutr 2001; 32 (5): 555–561.
Szajewska H, Mrukowicz JZ, Stoinska B, Prochowska A . Extensively and partially hydrolysed preterm formulas in the prevention of allergic diseases in preterm infants: a randomized, double-blind trial. Acta Paediatr 2004; 93 (9): 1159–1165.
Maggio L, Zuppa AA, Sawatzki G, Valsasina R, Schubert W, Tortorolo G . Higher urinary excretion of essential amino acids in preterm infants fed protein hydrolysates. Acta Paediatr 2005; 94 (1): 75–84.
Cooke R, Embleton N, Rigo J, Carrie A, Haschke F, Ziegler E . High protein pre-term infant formula: effect on nutrient balance, metabolic status and growth. Pediatr Res 2006; 59 (2): 265–270.
Cooke RJ, Watson D, Werkman S, Conner C . Effects of type of dietary protein on acid–base status, protein nutritional status, plasma levels of amino acids, and nutrient balance in the very low birth weight infant. J Pediatr 1992; 121 (3): 444–451.
Rigo J, Senterre J . Nutritional needs of premature infants: current issues. J Pediatr 2006; 149 (5 Suppl): S80–S88.
Lacroix M, Bos C, Leonil J, Airinei G, Luengo C, Dare S et al. Compared with casein or total milk protein, digestion of milk soluble proteins is too rapid to sustain the anabolic postprandial amino acid requirement. Am J Clin Nutr 2006; 84 (5): 1070–1079.
Beaufrere B . Protein turnover in low-birth-weight (LBW) infants. Acta Paediatr Suppl 1994; 405: 86–92.
Van Goudoever JB, Sulkers EJ, Halliday D, Degenhart HJ, Carnielli VP, Wattimena JL et al. Whole-body protein turnover in preterm appropriate for gestational age and small for gestational age infants: comparison of [15N]glycine and [1-(13)C]leucine administered simultaneously. Pediatr Res 1995; 37 (4 Part 1): 381–388.
Kalhan SC, Iben S . Protein metabolism in the extremely low-birth weight infant [review] [154 refs]. Clin Perinatol 2000; 27 (1): 23–56.
Cooke RJ . Adjustable fortification of human milk fed to preterm infants. J Perinatol 2006; 26: 591–592.
Kanakoudi F, Drossou V, Tzimouli V, Diamanti E, Konstantinidis T, Germenis A et al. Serum concentrations of 10 acute-phase proteins in healthy term and preterm infants from birth to age 6 months. Clin Chem 1995; 41 (4): 605–608.
Hammond KB . Interpretation of biochemical values. In: Hathaway WE, Groothuis JR, Hay WW (eds). Current Pediatric Diagnosis and Treatment. Los Angeles CA: Lange Medical Publishers, 1991 pp 1099–1107.
Mabry CC, Tietz NW . Reference ranges for laboratory tests. In: Behrman RE, Kliegman RM (eds). Nelson Textbook of Pediatrics. Philadelphia PA: Saunders, 1992 pp 1827–1860.
Meites S . Clinical Chemistry. 3rd edn. AACC Press: Washington, DC, 1989.
Robertson J, Shilkofski N . The Harriett Lane Handbook. 17th edn. St Louis, Elsevier Mosby, 2005.
Zlotkin SH, Casselman CW . Percentile estimates of reference values for total protein and albumin in sera of premature infants (less than 37 weeks of gestation). Clin Chem 1987; 33 (3): 411–413.
Zuppa AA, Visintini F, Cota F, Maggio L, Romagnoli C, Tortorolo G . Hydrolysed milk in preterm infants: an open problem. Acta Paediatr Suppl 2005; 94 (449): 84–86.
Acknowledgements
We thank the nursing and medical staff at the Newborn Center, University of Tennessee Center for Health Sciences, Memphis, TN for their support in this study. We also thank Dr C Hager, Nestec Ltd., Vevey, Switzerland for statistical expertise in analyzing the data. This study was supported by a grant from Nestec Ltd., Vevey, Switzerland. This study was supported by a grant from Nestec Ltd., Vevey, Switzerland.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Florendo, K., Bellflower, B., van Zwol, A. et al. Growth in preterm infants fed either a partially hydrolyzed whey or an intact casein/whey preterm infant formula. J Perinatol 29, 106–111 (2009). https://doi.org/10.1038/jp.2008.124
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2008.124
Keywords
This article is cited by
-
Specific formulas for preterm infants, how and when
Italian Journal of Pediatrics (2015)