Abstract
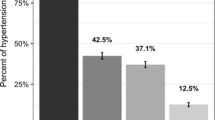
This study investigates socioeconomic differences in prevalence, awareness, control and self-management of hypertension in rural China. A cross-sectional survey was conducted among four ethnic minority groups in Yunnan Province: Na Xi, Li Shu, Dai and Jing Po. Approximately 5532 consenting individuals aged ⩾35 years (48.4% of whom were male) were selected to participate in the study using a stratified, multistage sampling technique. Information about participants’ demographic characteristics and hypertension awareness, treatment, control and self-management practices was obtained using a standard questionnaire. The age-standardised prevalence of hypertension in the study population was 33.6%. In hypertensive subjects, the overall levels of awareness, treatment and control of hypertension were 42.1%, 28.5% and 6.7%, respectively. Approximately 58.7% of hypertensive patients regularly self-monitored blood pressure (BP), 64.7% adhered to their physician-prescribed anti-hypertensive drugs, and 88.0% took at least one measure to control BP. Hypertensive patients of Jing Po ethnicity had the lowest rates of awareness, treatment, control and self-management of hypertension among the four ethnic minority groups studied. Individuals with lower levels of education were more likely to be hypertensive. Further, individuals with lower levels of education had a lower probability of awareness of their hypertensive status and of treatment with antihypertensive medication. Access to medical services was positively associated with awareness of suffering from hypertension, being treated with antihypertensive medication, and compliance with antihypertensive drug treatment. This study suggests that effective strategies to enhance awareness, treatment and management of hypertension should focus on individuals with low levels of education and poor access to medical services.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Olsen MH, Spencer S . A global perspective on hypertension: a Lancet Commission. Lancet 2015; 386: 637–638.
People’s Republic of China- United States Cardiovascular and Cardiopulmonary Epidemiology Research Group. An Epidemiological Study of Cardiovascular and Cardiopulmonary Disease Risk Factors in Four Populations in the People’s Republic of China: Baseline Report from the P.R.C.-U.S.A. Collaborative Study. Circulation 1992; 85: 1083–1096.
Chinese Center for Disease Control and Prevention. Report on chronic disease risk factor surveillance in China 2010. Military Medical Science Press: Beijing, China, 2012.
Van Grieken RA, Kirkenier AC, Koeter MW, Schene AH . Helpful self-management strategies to cope with enduring depression from the patients' point of view: a conceptmap study. BMC Psychiatry 2014; 14: 331.
Han HR, Song HJ, Nguyen Y, Kim MT . Measuring self-care in patients with hypertension: a systematic review of literature. J Cardiovasc Nurs 2014; 29: 55–67.
Booth HP, Prevost AT, Gulliford MC . Severity of obesity and management of hypertension, hypercholesterolaemia and smoking in primary care: population-based cohort study. J Hum Hypertens 2016; 30: 40–45.
Gupta R, Khedar RS, Panwar RB . Strategies for better hypertension control in India and other lower middle income countries. J Assoc Physicians India 2016; 64 (9): 58–64.
Li G, Wang H, Wang K, Wang W, Dong F, Qian Y et al. Prevalence, awareness, treatment, control and risk factors related to hypertension among urban adults in Inner Mongolia 2014: differences between Mongolian and Han populations. BMC Public Health 2016; 16: 294.
Fang L, Song J, Ma Z, Zhang L, Jing C, Chen D . Prevalence and characteristics of hypertension in mainland Chinese adults over decades: a systematic review. J Hum Hypertens 2014; 28: 649–656.
Camara A, Baldé NM, Diakité M, Sylla D, Baldé EH, Kengne AP et al. High prevalence, low awareness, treatment and control rates of hypertension in Guinea: results from a population-based STEPS survey. J Hum Hypertens 2016; 30: 237–244.
Li G, Hu H, Dong Z, Xie J, Zhou Y . Urban and suburban differences in hypertension trends and self-care: three population-based cross-sectional studies from 2005–2011. PLOS One 2015; 10: e0117999.
Gu J, Zhang XJ, Wang TH, Zhang Y, Chen Q . Hypertension knowledge, awareness, and self-management behaviors affect hypertension control: a community-based study in Xuhui District, Shanghai, China. Cardiology 2014; 127: 96–104.
Leng B, Jin Y, Li G, Chen L, Jin N . Socioeconomic status and hypertension: a meta-analysis. J Hypertens 2015; 33: 221–229.
Fan AZ, Strasser SM, Zhang X, Fang J, Crawford CG . State socioeconomic indicators and self-reported hypertension among US adults, 2011 behavioral risk factor surveillance system. Prev Chronic Dis 2015; 12: E27.
Vellakkal S, Millett C, Basu S, Khan Z, Aitsi-Selmi A, Stuckler D et al. Are estimates of socioeconomic inequalities in chronic disease artefactually narrowed by self-reported measures of prevalence in low-income and middle-income countries? Findings from the WHO-SAGE survey. J Epidemiol Community Health 2015; 69: 218–225.
Busingye D, Arabshahi S, Subasinghe AK, Evans RG, Riddell MA, Thrift AG . Do the socioeconomic and hypertension gradients in rural populations of low- and middle-income countries differ by geographical region? A systematic review and meta-analysis. Int J Epidemiol 2014; 43: 1563–1577.
Su D, Hu R, Fang L, Zhang J, Wang H, He Q et al. The association between socioeconomic status and blood pressure control in diagnosed hypertension patients. Zhonghua Yu Fang Yi Xue Za Zhi 2015; 49: 424–428.
Ljungman C, Kahan T, Schiöler L, Hjerpe P, Wettermark B, Boström KB et al. Antihypertensive treatment and control according to gender, education, country of birth and psychiatric disorder: the Swedish Primary Care Cardiovascular Database (SPCCD). J Hum Hypertens 2015; 29: 385–393.
Yang S, Liu S, Wang Y, Wan H, Zhao D, Li Y et al. High blood pressure in Chinese ethnic minorities: report from rural Yunnan province. Am J Hypertens 2011; 24: 1209–1214.
Gu H, Li W, Yang J, Wang Y, Bo J, Liu L . Hypertension prevalence, awareness, treatment and control among Han and four ethnic minorities (Uygur, Hui, Mongolian and Dai) in China. J Hum Hypertens 2015; 29: 555–560.
Morisky DE, Ang A, Krousel-Wood M, Ward HJ . Predictive validity of a medication adherence measure for hypertension control. J Clin Hypertens (Greenwich) 2008; 10: 348–354.
Perloff D, Grim C, Flack J, Frohlich ED, Hill M, McDonald M et al. Human blood pressure determination by sphygmomanometry. Circulation 1993; 88: 2460–2470.
Hense HW, Koivisto AM, Kuulasmaa K, Zaborskis A, Kupsc W, Tuomilehto J . Assessment of blood pressure measurement quality in the baseline surveys of the WHO MONICA project. J Hum Hypertens 1995; 9: 935–946.
James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J et al. 2014 evidence-based guideline for the management of high blood pressure in adults: Report from the panel members appointed to the Eight Joint National Committee (JNC 8). J Am Med Assoc 2014; 311: 507–520.
WHO/LASA/IOTF. The Asia Pacific Perspective: Redefining obesity and its treatment. Health Communications Australia Pty Ltd: Melbourne, Australia, 2000.
R Development Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing: Vienna, Austria, 2006.
Sun Z, Zheng L, Zhang X, Li J, Hu D, Sun Y . Ethnic differences in the incidence of hypertension among rural Chinese adults: results from Liaoning Province. PLoS ONE 2014; 9: e86867.
Black ML, Wise CA, Wang W, Bittles AH . Combining genetics and population history in the study of ethnic diversity in the People's Republic of China. Hum Biol 2006; 78: 277–293.
Xu T, Liu J, Zhu G, Liu J, Han S . Prevalence of prehypertension and associated risk factors among Chinese adults from a large-scale multi-ethnic population survey. BMC Public Health 2016; 16: 775.
Premkumar R, Pothen J, Rima J, Arole S . Prevalence of hypertension and prehypertension in a community-based primary health care program villages at central India. Indian Heart J 2016; 68: 270–277.
Guo J, Zhu YC, Chen YP, Hu Y, Tang XW, Zhang B . The dynamics of hypertension prevalence, awareness, treatment, control and associated factors in Chinese adults: results from CHNS 1991–2011. J Hypertens 2015; 33: 1688–1696.
McNaughton CD, Jacobson TA, Kripalani S . Low literacy is associated with uncontrolled blood pressure in primary care patients with hypertension and heart disease. Patient Educ Couns 2014; 96: 165–170.
Moser KA, Agrawal S, Davey Smith G, Ebrahim S . Socio-demographic inequalities in the prevalence, diagnosis and management of hypertension in India: analysis of nationally-representative survey data. PLoS ONE 2014; 9: e86043.
Yu B, Meng Q, Collins C, Tolhurst R, Tang S, Yan F et al. How does the New Cooperative Medical Scheme influence health service utilization? A study in two provinces in rural China. BMC Health Serv Res 2010; 10: 116–121.
Acknowledgements
The study was supported by grants from the National Natural Science Foundation of China (Grant numbers: 71263032, 81611130077), Major Specific Project Foundation of Yunnan Provincial Department of Education (Grant number: ZD2014005), Major Achievement Cultivation Project Foundation of Kunming Medical University (Grant number: CGPY201503) and Major Union Specific Project Foundation of Yunnan Provincial Science and Technology Department and Kunming Medical University (2016).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Cai, L., Dong, J., Cui, W. et al. Socioeconomic differences in prevalence, awareness, control and self-management of hypertension among four minority ethnic groups, Na Xi, Li Shu, Dai and Jing Po, in rural southwest China. J Hum Hypertens 31, 388–394 (2017). https://doi.org/10.1038/jhh.2016.87
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhh.2016.87