Abstract
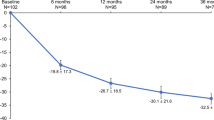
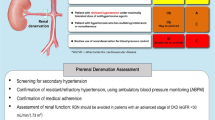
Reports detailing the response of hypertensive patients to renal denervation (RDN) in Asian patients are limited. We evaluated 6- and 12-month outcomes after RDN in an Asian population and compared outcomes to a primarily Caucasian population. The Global SYMPLICITY Registry (GSR) is a prospective, all-comer, worldwide registry that evaluates the safety and effectiveness of RDN and includes the Korean registry substudy (GSR Korea) and a Caucasian subset (GSR Caucasian). Given differences in baseline characteristics among GSR Korea (n=93) as compared with GSR Caucasian (n=169) patients, including lower baseline office systolic blood pressure (SBP), lower body mass index and differences in medications, propensity score adjustment was performed when comparing the change in SBP between subsets. The 6- and 12-month change in SBP in GSR Korea was −19.4±17.2 and −27.2±18.1 mm Hg, respectively (P<0.001 for both vs baseline). GSR Caucasian had a SBP change similar to GSR Korea at 6 months (−20.9±21.4 mm Hg, unadjusted P=0.547, adjusted P=0.998), whereas at 12 months the change was significantly less pronounced (−20.1±23.9 mm Hg, unadjusted P=0.004, adjusted P=0.002). There were no protocol-defined procedure-related adverse events and no chronic adverse events associated with the device in an Asian population. RDN provided a significant reduction in 6- and 12-month office SBP among Asian patients, with a favorable safety profile. The 12-month SBP reduction was larger than that observed in Caucasian patients.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Bertog SC, Sobotka PA, Sievert H . Renal denervation for hypertension. JACC Cardiovasc Interv 2012; 5 (3): 249–258.
Bohm M, Linz D, Urban D, Mahfoud F, Ukena C . Renal sympathetic denervation: applications in hypertension and beyond. Nat Rev Cardiol 2013; 10 (8): 465–476.
Krum H, Schlaich M, Whitbourn R, Sobotka PA, Sadowski J, Bartus K et al. Catheter-based renal sympathetic denervation for resistant hypertension: a multicentre safety and proof-of-principle cohort study. Lancet 2009; 373 (9671): 1275–1281.
Krum H, Schlaich MP, Sobotka PA, Bohm M, Mahfoud F, Rocha-Singh K et al. Percutaneous renal denervation in patients with treatment-resistant hypertension: final 3-year report of the Symplicity HTN-1 study. Lancet 2014; 383 (9917): 622–629.
Symplicity HTN-1 Investigators. Catheter-based renal sympathetic denervation for resistant hypertension: durability of blood pressure reduction out to 24 months. Hypertension 2011; 57 (5): 911–917.
Esler MD, Bohm M, Sievert H, Rump CL, Schmieder RE, Krum H et al. Catheter-based renal denervation for treatment of patients with treatment-resistant hypertension: 36 month results from the SYMPLICITY HTN-2 randomized clinical trial. Eur Heart J 2014; 35 (26): 1752–1759.
Esler MD, Krum H, Schlaich M, Schmieder RE, Bohm M, Sobotka PA et al. Renal sympathetic denervation for treatment of drug-resistant hypertension: one-year results from the Symplicity HTN-2 randomized, controlled trial. Circulation 2012; 126 (25): 2976–2982.
Symplicity HTN-2 Investigators, Esler MD, Krum H, Sobotka PA, Schlaich MP, Schmieder RE et al. Renal sympathetic denervation in patients with treatment-resistant hypertension (The Symplicity HTN-2 Trial): a randomised controlled trial. Lancet 2010; 376 (9756): 1903–1909.
Bhatt DL, Kandzari DE, O'Neill WW, D'Agostino R, Flack JM, Katzen BT et al. A controlled trial of renal denervation for resistant hypertension. N Engl J Med 2014; 370 (15): 1393–1401.
Kandzari DE, Bhatt DL, Brar S, Devireddy CM, Esler M, Fahy M et al. Predictors of blood pressure response in the SYMPLICITY HTN-3 trial. Eur Heart J 2015; 36 (4): 219–227.
Choo V . WHO reassesses appropriate body-mass index for Asian populations. Lancet 2002; 360 (9328): 235.
WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004; 363 (9403): 157–163.
Wang J, Thornton JC, Russell M, Burastero S, Heymsfield S, Pierson RN Jr . Asians have lower body mass index (BMI) but higher percent body fat than do whites: comparisons of anthropometric measurements. Am J Clin Nutr 1994; 60 (1): 23–28.
Bohm M, Mahfoud F, Ukena C, Bauer A, Fleck E, Hoppe UC et al. Rationale and design of a large registry on renal denervation: the Global SYMPLICITY registry. EuroIntervention 2013; 9 (4): 484–492.
Bohm M, Mahfoud F, Ukena C, Hoppe UC, Narkiewicz K, Negoita M et al. First report of the Global SYMPLICITY Registry on the effect of renal artery denervation in patients with uncontrolled hypertension. Hypertension 2015; 65 (4): 766–774.
Levey AS, Coresh J, Greene T, Stevens LA, Zhang YL, Hendriksen S et al. Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann Intern Med 2006; 145 (4): 247–254.
Mahfoud F, Cremers B, Janker J, Link B, Vonend O, Ukena C et al. Renal hemodynamics and renal function after catheter-based renal sympathetic denervation in patients with resistant hypertension. Hypertension 2012; 60 (2): 419–424.
Mahfoud F, Ukena C, Schmieder RE, Cremers B, Rump LC, Vonend O et al. Ambulatory blood pressure changes after renal sympathetic denervation in patients with resistant hypertension. Circulation 2013; 128 (2): 132–140.
Vogel B, Kirchberger M, Zeier M, Stoll F, Meder B, Saure D et al. Renal sympathetic denervation therapy in the real world: results from the Heidelberg registry. Clin Res Cardiol 2014; 103 (2): 117–124.
Praditpornsilpa K, Townamchai N, Chaiwatanarat T, Tiranathanagul K, Katawatin P, Susantitaphong P et al. The need for robust validation for MDRD-based glomerular filtration rate estimation in various CKD populations. Nephrol Dial Transplant 2011; 26 (9): 2780–2785.
Lee CS, Cha RH, Lim YH, Kim H, Song KH, Gu N et al. Ethnic coefficients for glomerular filtration rate estimation by the Modification of Diet in Renal Disease study equations in the Korean population. J Korean Med Sci 2010; 25 (11): 1616–1625.
Ma YC, Zuo L, Zhang CL, Wang M, Wang RF, Wang HY . Comparison of 99mTc-DTPA renal dynamic imaging with modified MDRD equation for glomerular filtration rate estimation in Chinese patients in different stages of chronic kidney disease. Nephrol Dial Transplant 2007; 22 (2): 417–423.
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis 2009; 53 (6): 982–992.
Sasayama S . Heart disease in Asia. Circulation 2008; 118 (25): 2669–2671.
Lawes CM, Rodgers A, Bennett DA, Parag V, Suh I, Ueshima H et al. Blood pressure and cardiovascular disease in the Asia Pacific region. J Hypertens 2003; 21 (4): 707–716.
Acknowledgements
We thank JiSun Yun and Marianne Wanten for study management, Nicole Brilakis, Colleen Gilbert and Sidney A Cohen for editorial assistance, and Martin Fahy and Minglei Liu for statistical analysis oversight (all from Medtronic, Inc.). This study was sponsored by Medtronic, Inc. Trial Registration: clinicaltrials.gov Identifier: NCT01534299.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
M Böhm received research support and speaker fees from Medtronic, Inc., and St Jude Medical. F Mahfoud received speaker honoraria from Medtronic, Inc., St Jude Medical and Boston Scientific, and is supported by the Deutsche Hochdruckliga and Deutsche Gesellschaft für Kardiologie. G Mancia is a consultant for Medtronic, Inc. M Esler received research support, honoraria and travel support from Medtronic, Inc. All other authors have no conflict of interest to declare.
Rights and permissions
About this article
Cite this article
Kim, BK., Böhm, M., Mahfoud, F. et al. Renal denervation for treatment of uncontrolled hypertension in an Asian population: results from the Global SYMPLICITY Registry in South Korea (GSR Korea). J Hum Hypertens 30, 315–321 (2016). https://doi.org/10.1038/jhh.2015.77
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhh.2015.77
This article is cited by
-
Update on Hypertension Research in 2021
Hypertension Research (2022)
-
Patient preference for renal denervation therapy in hypertension: A cross-sectional survey in Chengdu, China
Hypertension Research (2022)
-
Latest hypertension research to inform clinical practice in Asia
Hypertension Research (2022)
-
Perspectives of renal denervation from hypertension to heart failure in Asia
Hypertension Research (2022)
-
Long-term outcomes after renal denervation in an Asian population: results from the Global SYMPLICITY Registry in South Korea (GSR Korea)
Hypertension Research (2021)