Abstract
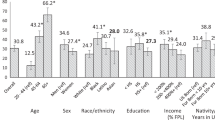
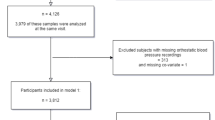
Age, sex, hypertension and dietary sodium are proposed to affect plasma and urinary catecholamines. Yet no prior study has examined the simultaneous effects of these factors within the same study population. So results may have been confounded by factors not determined. We investigate, for the first time, the impact of simultaneously determined predictors of plasma and urinary catecholamines and the relationship of catecholamines with the diagnosis of hypertension. Hypertensive and normotensive subjects (n=308) were studied off antihypertensives in liberal and low sodium balance. 24 h urinary catecholamines (norepinephrine and epinephrine) were measured. Plasma catecholamines were measured supine after overnight fast. Repeated measures multivariate linear regression models examined the effect of sex, race, age, body mass index (BMI), dietary salt (liberal salt vs low salt), hypertension status and mean arterial pressure (MAP) on plasma and urinary catecholamines. Logistic regression determined the relationship of catecholamines with diagnosis of hypertension. Dietary sodium restriction and increasing age predicted increased plasma and urinary norepinephrine, with sodium restriction having the greatest effect. Female sex predicted lower urinary and plasma epinephrine. Neither plasma nor urinary catecholamines predicted the diagnosis of hypertension. In summary, specific demographic factors variably impact catecholamines and should be considered when assessing catecholamines in research and clinical settings.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Young WF Jr . Endocrine hypertension. In: Melmed S, Williams RH (eds). Williams Textbook of Endocrinology 12th ed Chapter 15. Elsevier/Saunders: Philadelphia, 505, (2011).
Goldstein DS . Plasma catecholamines in clinical studies of cardiovascular diseases. Acta Physiol Scand Suppl 1984; 527: 39–41.
Boldt J, Menges T, Kuhn D, Diridis C, Hempelmann G . Alterations in circulating vasoactive substances in the critically ill-a comparison between survivors and non-survivors. Intensive Care Med 1995; 21: 218–225.
Anand IS, Fisher LD, Chiang YT, Latini R, Masson S, Maggioni AP et al. Changes in brain natriuretic peptide and norepinephrine over time and mortality and morbidity in the Valsartan Heart Failure Trial (Val-HeFT). Circulation 2003; 107 (9): 1278–1283.
Benedict CR, Shelton B, Johnstone DE, Francis G, Greenberg B, Konstam M et al. Prognostic significance of plasma norepinephrine in patients with asymptomatic left ventricular dysfunction. SOLVD Investigators. Circulation 1996; 94 (4): 690–697.
McEwen BS . Protective and damaging effects of stress mediators. N Engl J Med 1998; 338: 171–179.
Christensen NJ, Schultz-Larsen K . Resting venous plasma adrenalin in 70-year-old men correlated positively to survival in a population study: the significance of the physical working capacity. J Intern Med 1994; 235: 229–232.
Goldstein DS, Lake CR, Chernow B, Ziegler MG, Coleman MD, Taylor AA et al. Age-dependence of hypertensive-normotensive differences in plasma norepinephrine. Hypertension 1983; 5: 100–104.
Gonzalez-Trapaga JL, Nelesen RA, Dimsdale JE, Mills PJ, Kennedy B, Parmer RJ et al. Plasma epinephrine levels in hypertension and across gender and ethnicity. Life Sci 2000; 66: 2383–2392.
Taylor AA, Pool JL, Lake CR, Ziegler MG, Rosen RA, Rollins DE et al. Plasma norepinephrine concentrations: no differences among normal volunteers and low, high or normal renin hypertensive patients. Life Sci 1978; 22: 1499–1510.
Campese VM, Romoff MS, Levitan D, Saglikes Y, Friedler RM, Massry SG . Abnormal relationship between sodium intake and sympathetic nervous system activity in salt-sensitive patients with essential hypertension. Kidney Int 1982; 21: 371–378.
Conlin PR, Braley LM, Menachery AI, Hollenberg NK, Williams GH . Abnormal norepinephrine and aldosterone responses to upright posture in nonmodulating hypertension. J Clin Endocrinol Metab 1992; 75: 1017–1021.
Luft FC, Rankin LI, Henry DP, Bloch R, Grim CE, Weyman AE et al. Plasma and urinary norepinephrine values at extremes of sodium intake in normal man. Hypertension 1979; 1: 261–266.
Kennedy BP, Rao F, Botiglieri T, Sharma S, Lillie EO, Ziegler MG et al. Contributions of the sympathetic nervous system, glutathione, body mass and gender to blood pressure increase with normal aging: influence of heredity. J Hum Hypertens 2005; 19: 951–969.
White IR, Brunner EJ, Barron JL . A comparison of overnight and 24 hour collection to measure urinary catecholamines. J Clin Epidemiol 1995; 48: 263–267.
Romoff MS, Keusch G, Campese VM, Wang MS, Friedler RM, Weidmann P et al. Effect of sodium intake on plasma catecholamines in normal subjects. J Clin Endocrinol Metab 1979; 48: 26–31.
Fujita T, Henry WL, Bartter FC, Lake CR, Delea CS . Factors influencing blood pressure in salt-sensitive patients with hypertension. Am J Med 1980; 69: 334–344.
Nicholls MG, Kiowski W, Zweifler AJ, Julius S, Schork MA . Greenhouse J. Plasma norepinephrine variations with dietary sodium intake. Hypertension 1980; 2: 29–32.
Raji A, Williams GH, Jeunemaitre X, Hopkins PN, Hunt SC, Hollenberg NK et al. Insulin resistance in hypertensives: effect of salt sensitivity, renin status and sodium intake. J Hypertens 2001; 19: 99–105.
Yatabe MS, Yatabe J, Yoneda M, Watanabe T, Otsuki M, Felder RA et al. Salt sensitivity is associated with insulin resistance, sympathetic overactivity, and decreased suppression of circulating renin activity in lean patients with essential hypertension. Am J Clin Nutr 2010; 92: 77–82.
Engstrom BE, Karlsson FA, Wide L . Gender differences in diurnal growth hormone and epinephrine values in young adults during ambulation. Clin Chem 1999; 45: 1235–1239.
Hansen AM, Garde AH, Christensen JM, Eller NH, Netterstrom B . Reference intervals and variation for urinary epinephrine, norepinephrine and cortisol in healthy men and women in Denmark. Clin Chem Lab Med 2001; 39: 842–849.
Masi CM, Rickett EM, Hawkley LC, Cacioppo JT . Gender and ethnic differences in urinary stress hormones: the population-based Chicago Health, Aging, and Social Relations Study. J Appl Physiol 2004; 97: 941–947.
Gustafson AB, Kalkhoff RK . Influence of sex and obesity on plasma catecholamine response to isometric exercise. J Clin Endocrinol Metab 1982; 55: 703–708.
Ziegler MC, Lake CR, Wood JH, Ebert MH . Circadian rhythm in cerebrospinal fluid noradrenaline of man and monkey. Nature 1976; 264: 656–658.
Deane R, Chummun H, Prashad D . Differences in urinary stress hormones in male and female nurses at different ages. J Adv Nurs 2002; 37: 304–310.
Gerlo EA, Schoors DF, Dupont AG . Age- and sex-related differences for the urinary excretion of norepinephrine, epinephrine, and dopamine in adults. Clin Chem 1991; 37: 875–878.
Grassi G, Dell'Oro R, Seravalle G, Foglia G, Trevano FQ, Mancia G . Short- and long-term neuroadrenergic effects of moderate dietary sodium restriction in essential hypertension. Circulation 2002; 106: 1957–1961.
Acknowledgements
We thank the fellows, trainees and nursing staff who have contributed to the studies involving the HyperPath cohort. The project was supported in part by the following grants: U54LM008748 from the National Library of Medicine; UL1RR025758, Harvard Clinical and Translational Science Center, from the National Center for Research Resources; M01-RR02635, Brigham and Women’s Hospital, General Clinical Research Center, from the National Center for Research Resources; and National Institute of Health grants HL47651, HL59424, K12HD051959-07 (Harvard BIRCWH Scholars Program, ARS), K24 RR0186-13-01 (EWS), 5 KL2 RR025757 (BC); 12CRP11690012 (BC) from the American Heart Association and the Specialized Center of Research (SCOR) in Molecular Genetics of Hypertension P50HL055000.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Saxena, A., Chamarthi, B., Williams, G. et al. Predictors of plasma and urinary catecholamine levels in normotensive and hypertensive men and women. J Hum Hypertens 28, 292–297 (2014). https://doi.org/10.1038/jhh.2013.112
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhh.2013.112
Keywords
This article is cited by
-
Diazepam as an oral hypnotic increases nocturnal blood pressure in the elderly
Aging Clinical and Experimental Research (2019)