Abstract
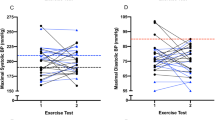
The aim of this prospective cohort study was to identify which blood pressure measurement during exercise is the best predictor of future hypertension. Further we aimed to create a risk chart to facilitate the evaluation of blood pressure reaction during exercise testing. A number (n=1047) of exercise tests by bicycle ergometry, performed in 1996 and 1997 were analysed. In 2007–2008, 606 patients without hypertension at the time of the exercise test were sent a questionnaire aimed to identify current hypertension. The response rate was 58% (n=352). During the 10–12 years between exercise test and questionnaire, 23% developed hypertension. The strongest predictors of future hypertension were systolic blood pressure (SBP) before exercise (odds ratios (OR) 1.63 (1.31–2.01) for 10 mm Hg difference) in combination with the increase of SBP over time during exercise testing (OR 1.12 (1.01–1.24) steeper increase for every 1 mm Hg min−1). A high SBP before exercise and a steep rise in SBP over time represented a higher risk of developing hypertension. A risk chart based on SBP before exercise, increase of SBP over time and body mass index was created. SBP before exercise, maximal SBP during exercise and SBP at 100 W were significant single predictors of future hypertension and the prediction by maximal SBP was improved by adjusting for time/power at which SBP max was reached during exercise testing. Recovery ratio (maximal SBP/SBP 4 min after exercise) was not predictive of future hypertension.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Ezzati M, Lopez AD, Rodgers A, Vander Hoorn S, Murray CJ . Selected major risk factors and global and regional burden of disease. Lancet 2002; 360 (9343): 1347–1360.
Weinehall L, Ohgren B, Persson M, Stegmayr B, Boman K, Hallmans G et al. High remaining risk in poorly treated hypertension: the ‘rule of halves’ still exists. J Hypertens 2002; 20 (10): 2081–2088.
D’Agostino Sr RB, Grundy S, Sullivan LM, Wilson P . Validation of the Framingham coronary heart disease prediction scores: results of a multiple ethnic groups investigation. JAMA 2001; 286 (2): 180–187.
Conroy RM, Pyorala K, Fitzgerald AP, Sans S, Menotti A, De Backer G et al. Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. Eur Heart J 2003; 24 (11): 987–1003.
Benbassat J, Froom P . Blood pressure response to exercise as a predictor of hypertension. Arch Intern Med 1986; 146 (10): 2053–2055.
Miyai N, Arita M, Morioka I, Miyashita K, Nishio I, Takeda S . Exercise BP response in subjects with high-normal BP: exaggerated blood pressure response to exercise and risk of future hypertension in subjects with high-normal blood pressure. J Am Coll Cardiol 2000; 36 (5): 1626–1631.
Manolio TA, Burke GL, Savage PJ, Sidney S, Gardin JM, Oberman A . Exercise blood pressure response and 5-year risk of elevated blood pressure in a cohort of young adults: The CARDIA study. Am J Hypertens 1994; 7 (3): 234–241.
Singh JP, Larson MG, Manolio TA, O’Donnell CJ, Lauer M, Evans JC et al. Blood pressure response during treadmill testing as a risk factor for new-onset hypertension. The Framingham Heart Study. Circulation 1999; 99 (14): 1831–1836.
Tsumura K, Hayashi T, Hamada C, Endo G, Fujii S, Okada K . Blood pressure response after two-step exercise as a powerful predictor of hypertension: the Osaka Health Survey. J Hypertens 2002; 20 (8): 1507–1512.
Kjeldsen SE, Mundal R, Sandvik L, Erikssen G, Thaulow E, Erikssen J . Exercise blood pressure predicts cardiovascular death and myocardial infarction. Blood Press Monit 1997; 2 (3): 147–153.
Kjeldsen SE, Mundal R, Sandvik L, Erikssen G, Thaulow E, Erikssen J . Supine and exercise systolic blood pressure predict cardiovascular death in middle-aged men. J Hypertens 2001; 19 (8): 1343–1348.
Dlin RA, Hanne N, Silverberg DS, Bar-Or O . Follow-up of normotensive men with exaggerated blood pressure response to exercise. Am Heart J 1983; 106 (2): 316–320.
Lauer MS, Levy D, Anderson KM, Plehn JF . Is there a relationship between exercise systolic blood pressure response and left ventricular mass? The Framingham Heart Study. Ann Intern Med 1992; 116 (3): 203–210.
Wilson MF, Sung BH, Pincomb GA, Lovallo WR . Exaggerated pressure response to exercise in men at risk for systemic hypertension. Am J Cardiol 1990; 66 (7): 731–736.
Zanettini JO, Pisani Zanettini J, Zanettini MT, Fuchs FD . Correction of the hypertensive response in the treadmill testing by the work performance improves the prediction of hypertension by ambulatory blood pressure monitoring and incidence of cardiac abnormalities by echocardiography: results of an eight year follow-up study. Int J Cardiol 2010; 141 (3): 243–249.
Laukkanen JA, Kurl S, Salonen R, Lakka TA, Rauramaa R, Salonen JT . Systolic blood pressure during recovery from exercise and the risk of acute myocardial infarction in middle-aged men. Hypertension 2004; 44 (6): 820–825.
Bruce RA, Hornsten TR . Exercise stress testing in evaluation of patients with ischemic heart disease. Prog Cardiovasc Dis 1969; 11 (5): 371–390.
Nordenfelt I, Adolfsson L, Nilsson JE, Olsson S . Reference values for exercise tests with continuous increase in load. Clin Physiol 1985; 5 (2): 161–172.
Franklin SS, Gustin Wt, Wong ND, Larson MG, Weber MA, Kannel WB et al. Hemodynamic patterns of age-related changes in blood pressure. The Framingham Heart Study. Circulation 1997; 96 (1): 308–315.
Mundal R, Kjeldsen SE, Sandvik L, Erikssen G, Thaulow E, Erikssen J . Predictors of 7-year changes in exercise blood pressure: effects of smoking, physical fitness and pulmonary function. J Hypertens 1997; 15: 245–249.
Everson SA, Kaplan GA, Goldberg DE, Salonen JT . Anticipatory blood pressure response to exercise predicts future high blood pressure in middle-aged men. Hypertension 1996; 27 (5): 1059–1064.
Smith EE, Guyton AC, Manning RD, White RJ . Integrated mechanisms of cardiovascular response and control during exercise in the normal human. Prog Cardiovasc Dis 1976; 18 (6): 421–444.
Kurl S, Laukkanen JA, Rauramaa R, Lakka TA, Sivenius J, Salonen JT . Systolic blood pressure response to exercise stress test and risk of stroke. Stroke 2001; 32 (9): 2036–2041.
Laukkanen JA, Kurl S, Rauramaa R, Lakka TA, Venalainen JM, Salonen JT . Systolic blood pressure response to exercise testing is related to the risk of acute myocardial infarction in middle-aged men. Eur J Cardiovasc Prev Rehabil 2006; 13 (3): 421–428.
Yosefy C, Jafari J, Klainman E, Brodkin B, Handschumacher MD, Vaturi M . The prognostic value of post-exercise blood pressure reduction in patients with hypertensive response during exercise stress test. Int J Cardiol 2006; 111 (3): 352–357.
Huang CL, Su TC, Chen WJ, Lin LY, Wang WL, Feng MH et al. Usefulness of paradoxical systolic blood pressure increase after exercise as a predictor of cardiovascular mortality. Am J Cardiol 2008; 102 (5): 518–523.
Welin C, Wilhelmsen L, Welin L, Johansson S, Rosengren A . Perceived health in 50-year-old women and men and the correlation with risk factors, disease and symptoms. Gend Med 2011; 8 (2): 139–149.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Holmqvist, L., Mortensen, L., Kanckos, C. et al. Exercise blood pressure and the risk of future hypertension. J Hum Hypertens 26, 691–695 (2012). https://doi.org/10.1038/jhh.2011.99
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhh.2011.99
Keywords
This article is cited by
-
Reliability of blood pressure responses used to define an exaggerated blood pressure response to exercise in young healthy adults
Journal of Human Hypertension (2023)
-
Association of Morning Surge and Postexercise Heart Rate and Blood Pressure Recovery
High Blood Pressure & Cardiovascular Prevention (2022)
-
Relationship Between Cardiorespiratory Fitness, Baseline Blood Pressure and Hypertensive Response to Exercise in the Ferrari Corporate Population
High Blood Pressure & Cardiovascular Prevention (2022)
-
Cardiopulmonary Exercise Testing in Athletes: Expect the Unexpected
Current Treatment Options in Cardiovascular Medicine (2021)
-
Value of myocardial work for assessment of myocardial adaptation to increased afterload in patients with high blood pressure at peak exercise
The International Journal of Cardiovascular Imaging (2020)