Abstract
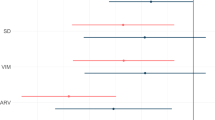
The 2004 UK Quality and Outcomes Framework (QOF) remunerates general practitioners for achieving a target blood pressure (BP) of ⩽150/90 mm Hg for patients with ischaemic heart disease, stroke and hypertension. Using the DIN-LINK GP database, we investigated whether introducing the target altered BP recording. We extracted 3 164 189 BP measurements from 236 467 patients, with the above diagnoses from 2000 to 2005. Treatment was assessed by Read codes indicating prescriptions for antihypertensive drugs. Over this period, recorded systolic BP (SBP) fell: 36% had an SBP >150 mm Hg in 2000–2001, and only 19% in 2004–2005. However, there was a trend towards recording systolic values just below, rather than just above the 150 cut-off. In 2000–2001, 2.3% of patients had 148–149 recorded and 1.8% had 151–152. In 2004–2005, the figures were 4.2 and 1.3%, respectively. By smoothing the distribution we estimate that the true percentage of patients with SBP>150 mm Hg in 2004–2005 was 23%, rather than the 19% recorded. Moreover, patients with a recorded SBP=148–149 were more likely to have a recorded diastolic BP⩽90 (93%) than patients with SBP=151–152 (78%). However, patients just below the 150 mm Hg cut-off received more antihypertensive treatment than those just above it (odds ratio=1.20, 95% confidence interval 1.01–1.41). We conclude that blood pressure levels in UK primary care have continued to fall through the introduction of QOF, offering significant public health benefits in the future. This fall has been exaggerated due to values being clustered just below the QOF target, but there is no evidence of adverse effects of this on clinical management.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Department of Health, London UK. General Medical Services Contract. http://www.dh.gov.uk/en/Healthcare/Primarycare/Primarycarecontracting/GMS/DH_4125637, Last accessed: 11/7/08.
Shekelle P . New contract for general practitioners. BMJ 2003; 326: 457–458.
Graham I, Atar D, Borch-Johnsen K, Boysen G, Burell G, Cifkova R et al. European guidelines on cardiovascular disease prevention in clinical practice: executive summary. Eur Heart J 2007; 28: 2375–2414.
Wingfield D, Cooke J, Thijs L, Staessen JA, Fletcher AE, Fagard R et al. Terminal digit preference and single-number preference in the Syst-Eur trial: influence of quality control. Blood Press Monit 2002; 7: 169–177.
Carey IM, DeWilde S, Harris T, Whincup PH, Cook DG . Spurious trends in coronary heart disease incidence: unintended consequences of the new GP contract? Br J Gen Pract 2007; 57: 486–489.
Heath I, Hippisley-Cox J, Smeeth L . Measuring performance and missing the point? BMJ 2007; 335: 1075–1076.
Primatesta P, Brookes M, Poulter NR . Improved hypertension management and control: results from the health survey for England 1998. Hypertension 2001; 38: 827–832.
Carey IM, Cook DG, De Wilde S, Bremner SA, Richards N, Caine S et al. Developing a large electronic primary care database (Doctors’ Independent Network) for research. Int J Med Inform 2004; 73: 443–453.
Lusignan S, Sismanidis C, Carey IM, DeWilde S, Richards N, Cook DG . Trends in the prevalence and management of diagnosed type 2 diabetes 1994–2001 in England and Wales. BMC Fam Pract 2005; 6: 13.
DeWilde S, Carey IM, Emmas C, Richards N, Cook DG . Trends in the prevalence of diagnosed atrial fibrillation, its treatment with anticoagulation and predictors of such treatment in UK primary care. Heart 2006; 92: 1064–1070.
De Wilde S, Carey IM, Bremner SA, Richards N, Hilton SR, Strachan DP et al. A comparison of the recording of 30 common childhood conditions in the Doctor's Independent Network and General Practice Research Databases. Health Stat Q 2004; 22: 21–31.
Health Survey for England. Trends in blood pressure levels. http://www.heartstats.org/datapage.asp?id=1000, Last accessed: 11/7/08.
DeWilde S, Carey IM, Richards N, Whincup PH, Cook DG . Trends in secondary prevention of ischaemic heart disease in the UK 1994–2005: use of individual and combination treatment. Heart 2008; 94: 83–88.
Ashworth M, Medina J, Morgan M . Effect of social deprivation on blood pressure monitoring and control in England: a survey of data from the quality and outcomes framework. BMJ 2008; 337: a2030.
De Lusignan S, Belsey J, Hague N, Dzregah B . End-digit preference in blood pressure recordings of patients with ischaemic heart disease in primary care. J Hum Hypertens 2004; 18: 261–265.
Beales D . How accurate are automated blood pressure monitors? Br J Community Nurs 2005; 10: 334–338.
McManus RJ, Mant J, Hull MR, Hobbs FD . Does changing from mercury to electronic blood pressure measurement influence recorded blood pressure? An observational study. Br J Gen Pract 2003; 53: 953–956.
Harrison WN, Lancashire RJ, Marshall TP . Variation in recorded blood pressure terminal digit bias in general practice. J Hum Hypertens 2008; 22 (3): 163–167.
Manning G, Brooks A, Slinn B, Millar-Craig MW, Donnelly R . Assessing blood pressure control in patients treated for hypertension: comparing different measurements and targets. Br J Gen Pract 2006; 56: 375–377.
Wingfield D, Freeman GK, Bulpitt CJ . Selective recording in blood pressure readings may increase subsequent mortality. QJM 2002; 95: 571–577.
Nietert PJ, Wessell AM, Feifer C, Ornstein SM . Effect of terminal digit preference on blood pressure measurement and treatment in primary care. Am J Hypertens 2006; 19: 147–152.
Acknowledgements
We acknowledge with gratitude the general practitioners who provided the data to the DIN-LINK. We are grateful to Cegedim Strategic Data (Woking, Surrey, UK) for their technical assistance with DIN-LINK database and for their helpful support. IMC and SDW were funded by a grant from the BUPA Foundation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Carey, I., Nightingale, C., DeWilde, S. et al. Blood pressure recording bias during a period when the Quality and Outcomes Framework was introduced. J Hum Hypertens 23, 764–770 (2009). https://doi.org/10.1038/jhh.2009.18
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhh.2009.18
Keywords
This article is cited by
-
Calculating Total Health Service Utilisation and Costs from Routinely Collected Electronic Health Records Using the Example of Patients with Irritable Bowel Syndrome Before and After Their First Gastroenterology Appointment
PharmacoEconomics (2016)
-
Glucose, blood pressure and cholesterol levels and their relationships to clinical outcomes in type 2 diabetes: a retrospective cohort study
Diabetologia (2015)
-
Pay-for-Performance: Impact on Diabetes
Current Diabetes Reports (2013)