Abstract
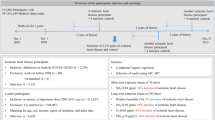
We evaluated the association between short-term exposure to ambient ozone air pollution and stroke hospital admissions among adult residents of South Carolina (SC). Data on all incident stroke hospitalizations from 2002 to 2006 were obtained from the SC Office of Research and Statistics. Ozone exposure data were obtained from the US Environmental Protection Agency’s Hierarchical Bayesian Model. A semi-symmetric bidirectional case-crossover design was used to examine the association between ozone exposure on lag days 0–2 (0 to 2 days before admission) and stroke hospitalization. Conditional logistic regression was used to estimate odds ratios (ORs) and 95% confidence intervals (CIs). No significant associations were observed between short-term ozone exposure and hospitalization for all stroke (e.g., lag day 0: OR=0.98; 95% CI=0.96, 1.00) or ischemic stroke (lag day 0: OR=0.98; 95% CI=0.96, 1.01). Risk of hospitalization for hemorrhagic stroke appeared to be higher among African Americans than European Americans; however, the majority of these associations did not reach statistical significance. Among adults in SC from 2002 to 2006, there was no evidence of an association between ozone exposure and risk of hospitalization for all stroke or ischemic stroke; however, African Americans may have an increased risk of hemorrhagic stroke.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ et al. Heart disease and stroke statistics—2014 update: a report from the American Heart Association. Circulation 2014; 129: e28–e292.
Andersen ZJ, Olsen TS, Andersen KK, Loft S, Ketzel M, Raaschou-Nielsen O . Association between short-term exposure to ultrafine particles and hospital admissions for stroke in Copenhagen, Denmark. Eur Heart J 2010; 31: 2034–2040.
Bedada GB, Smith CJ, Tyrrell PJ, Hirst AA, Agius R . Short-term effects of ambient particulates and gaseous pollutants on the incidence of transient ischaemic attack and minor stroke: a case-crossover study. Environ Health 2012; 11: 77.
Wellenius GA, Burger MR, Coull BA, Schwartz J, Suh HH, Koutrakis P et al. Ambient air pollution and the risk of acute ischemic stroke. Arch Intern Med 2012; 172: 229–234.
Ljungman PL, Mittleman MA . Ambient air pollution and stroke. Stroke 2014; 45: 3734–3741.
WHO. Burden of disease from ambient air pollution for 2012: World Health Organization; 2014. Available at http://www.who.int/phe/health_topics/outdoorair/databases/AAP_BoD_results_March2014.pdf (cited 12 May 2014).
Cesaroni G, Forastiere F, Stafoggia M, Andersen ZJ, Badaloni C, Beelen R et al. Long term exposure to ambient air pollution and incidence of acute coronary events: prospective cohort study and meta-analysis in 11 European cohorts from the ESCAPE Project. BMJ 2014; 348: f7412.
Chang CC, Kuo CC, Liou SH, Yang CY . Fine particulate air pollution and hospital admissions for myocardial infarction in a subtropical city: Taipei, Taiwan. J Toxicol Environ Health A 2013; 76: 440–448.
Madrigano J, Kloog I, Goldberg R, Coull BA, Mittleman MA, Schwartz J . Long-term exposure to PM2.5 and incidence of acute myocardial infarction. Environ Health Perspect 2013; 121: 192–196.
Corea F, Silvestrelli G, Baccarelli A, Giua A, Previdi P, Siliprandi G et al. Airborne pollutants and lacunar stroke: a case cross-over analysis on stroke unit admissions. Neurol Int 2012; 4: e11.
Oudin A, Stromberg U, Jakobsson K, Stroh E, Bjork J . Estimation of short-term effects of air pollution on stroke hospital admissions in southern Sweden. Neuroepidemiology 2010; 34: 131–142.
Tsai SS, Goggins WB, Chiu HF, Yang CY . Evidence for an association between air pollution and daily stroke admissions in Kaohsiung, Taiwan. Stroke 2003; 34: 2612–2616.
Xu X, Sun Y, Ha S, Talbott EO, Lissaker CT . Association between ozone exposure and onset of stroke in Allegheny County, Pennsylvania, USA, 1994-2000. Neuroepidemiology 2013; 41: 2–6.
Tankersley CG, Georgakopoulos D, Tang WY, Abston E, Bierman A, Sborz N . Effects of ozone and particulate matter on cardiac mechanics: role of the atrial natriuretic peptide gene. Toxicol Sci 2013; 131: 95–107.
Kodavanti UP, Thomas R, Ledbetter AD, Schladweiler MC, Shannahan JH, Wallenborn JG et al. Vascular and cardiac impairments in rats inhaling ozone and diesel exhaust particles. Environ Health Perspect 2011; 119: 312–318.
Brook RD, Brook JR, Urch B, Vincent R, Rajagopalan S, Silverman F . Inhalation of fine particulate air pollution and ozone causes acute arterial vasoconstriction in healthy adults. Circulation 2002; 105: 1534–1536.
Brook RD, Franklin B, Cascio W, Hong Y, Howard G, Lipsett M et al. Air pollution and cardiovascular disease: a statement for healthcare professionals from the Expert Panel on Population and Prevention Science of the American Heart Association. Circulation 2004; 109: 2655–2671.
Lackland DT, Roccella EJ, Deutsch AF, Fornage M, George MG, Howard G et al. Factors influencing the decline in stroke mortality: a statement from the American Heart Association/American Stroke Association. Stroke 2014; 45: 315–353.
Henrotin JB, Besancenot JP, Bejot Y, Giroud M . Short-term effects of ozone air pollution on ischaemic stroke occurrence: a case-crossover analysis from a 10-year population-based study in Dijon, France. Occup Environ Med 2007; 64: 439–445.
Mechtouff L, Canoui-Poitrine F, Schott AM, Nighoghossian N, Trouillas P, Termoz A et al. Lack of association between air pollutant exposure and short-term risk of ischaemic stroke in Lyon, France. Int J Stroke 2012; 7: 669–674.
Suissa L, Fortier M, Lachaud S, Staccini P, Mahagne MH . Ozone air pollution and ischaemic stroke occurrence: a case-crossover study in Nice, France. BMJ 2013; 3: e004060.
Gillum RF, Ingram DD . Relation between residence in the southeast region of the United States and stroke incidence. The NHANES I Epidemiologic Followup Study. Am J Epidemiol 1996; 144: 665–673.
Lackland DT, Bachman DL, Carter TD, Barker DL, Timms S, Kohli H . The geographic variation in stroke incidence in two areas of the southeastern stroke belt: the Anderson and Pee Dee Stroke Study. Stroke 1998; 29: 2061–2068.
EPA. Green book downloads: nonattainment areas: Environmental Protection Agency; 2014. Available at http://epa.gov/airquality/greenbook/data_download.html (cited 15 August 2014).
Kokotailo RA, Hill MD . Coding of stroke and stroke risk factors using international classification of diseases, revisions 9 and 10. Stroke 2005; 36: 1776–1781.
Dimmick F, Hall E, Tikvart J . Hierarchical Bayesian Model (HBM)-derived Estimates of Air Quality for 2001: Annual Report. US Environmental Protection Agency: : Durham, NC. 2010.
EPA. Technology Transfer Network Air Quality System (AQS): Environmental Protection Agency; 2013. Available at http://www.epa.gov/ttn/airs/airsaqs/detaildata/downloadaqsdata.htm (cited 31 March 2013).
Navidi W, Weinhandl E . Risk set sampling for case-crossover designs. Epidemiology 2002; 13: 100–105.
Wang SV, Coull BA, Schwartz J, Mittleman MA, Wellenius GA . Potential for bias in case-crossover studies with shared exposures analyzed using SAS. Am J Epidemiol 2011; 174: 118–124.
Summary File 3, Summary File 4. US Census, Bureau, Washington, DC, 2000.
RHRC. Zip Code RUCA Approximation: University of Washington Rural Health Research Center 2005. Available at http://depts.washington.edu/uwruca/ruca-download.php (cited 1 May 2012).
Rienecker MM, Suarez MJ, Gelaro R, Todling R, Bacmeister J, Liu E et al. MERRA: NASA’s Modern-Era Retrospective Analysis for Research and Applications. J Climate 2011; 24: 3624–3648.
Nascimento LF, Francisco JB, Patto MB, Antunes AM . Environmental pollutants and stroke-related hospital admissions. Cad Saude Publica 2012; 28: 1319–1324.
Warlow CP . Epidemiology of stroke. Lancet 1998; 352 Suppl 3: Siii1–Siii4.
Wellenius GA, Schwartz J, Mittleman MA . Air pollution and hospital admissions for ischemic and hemorrhagic stroke among medicare beneficiaries. Stroke 2005; 36: 2549–2553.
Lisabeth LD, Escobar JD, Dvonch JT, Sanchez BN, Majersik JJ, Brown DL et al. Ambient air pollution and risk for ischemic stroke and transient ischemic attack. Ann Neurol 2008; 64: 53–59.
Yang WS, Wang X, Deng Q, Fan WY, Wang WY . An evidence-based appraisal of global association between air pollution and risk of stroke. Int J Cardiol 2014; 175: 307–313.
Appelros P, Stegmayr B, Terent A . Sex differences in stroke epidemiology: a systematic review. Stroke 2009; 40: 1082–1090.
Labovitz DL, Halim A, Boden-Albala B, Hauser WA, Sacco RL . The incidence of deep and lobar intracerebral hemorrhage in whites, blacks, and Hispanics. Neurology 2005; 65: 518–522.
Chiu HF, Chang CC, Yang CY . Relationship between hemorrhagic stroke hospitalization and exposure to fine particulate air pollution in Taipei, Taiwan. J Toxicol Environ Health A 2014; 77: 1154–1163.
Maheswaran R, Pearson T, Smeeton NC, Beevers SD, Campbell MJ, Wolfe CD . Outdoor air pollution and incidence of ischemic and hemorrhagic stroke: a small-area level ecological study. Stroke 2012; 43: 22–27.
Lokken RP, Wellenius GA, Coull BA, Burger MR, Schlaug G, Suh HH et al. Air pollution and risk of stroke: underestimation of effect due to misclassification of time of event onset. Epidemiology 2009; 20: 137–142.
Acknowledgements
We acknowledge the SC Office of Research and Statistics, now under the SC Revenue and Fiscal Affairs Office, for providing data on stroke hospitalizations. Work by Dr. Mittleman was supported by the US Environmental Protection Agency grant RD 83479801.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Journal of Exposure Science and Environmental Epidemiology website
Rights and permissions
About this article
Cite this article
Montresor-López, J., Yanosky, J., Mittleman, M. et al. Short-term exposure to ambient ozone and stroke hospital admission: A case-crossover analysis. J Expo Sci Environ Epidemiol 26, 162–166 (2016). https://doi.org/10.1038/jes.2015.48
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jes.2015.48
Keywords
This article is cited by
-
Effect of short-term exposure to air pollution on daily cardio- and cerebrovascular hospitalisations in areas with a low level of air pollution
Environmental Science and Pollution Research (2023)
-
Long-term exposure to air pollution and cerebrovascular disease: findings from Beijing Health Management Cohort study
Frontiers of Environmental Science & Engineering (2023)
-
Personalized Spiking Neural Network Models of Clinical and Environmental Factors to Predict Stroke
Cognitive Computation (2022)
-
Associations between ambient air pollution, meteorology, and daily hospital admissions for ischemic stroke: a time-stratified case-crossover study in Beijing
Environmental Science and Pollution Research (2022)
-
Short-term associations of ambient air pollution with hospital admissions for ischemic stroke in 97 Japanese cities
Environmental Science and Pollution Research (2022)