Abstract
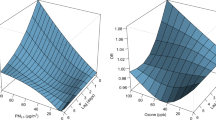
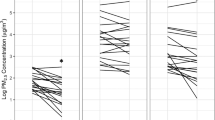
Particulate matter with aerodynamic diameter <2.5 μm (PM2.5) is associated with asthma exacerbation. In the Children’s Air Pollution Asthma Study, we investigated the longitudinal association of PM2.5 and its components from indoor and outdoor sources with cough and wheeze symptoms in 36 asthmatic children. The sulfur tracer method was used to estimate infiltration factors. Mixed proportional odds models for an ordinal response were used to relate daily cough and wheeze scores to PM2.5 exposures. The odds ratio associated with being above a given symptom score for a SD increase in PM2.5 from indoor sources (PMIS) was 1.24 (95% confidence interval: 0.92–1.68) for cough and 1.63 (1.11–2.39) for wheeze. Ozone was associated with wheeze (1.82, 1.19–2.80), and cough was associated with indoor PM2.5 components from outdoor sources (denoted with subscript “OS”) bromine (BrOS: 1.32, 1.05–1.67), chlorine (ClOS: 1.27, 1.02–1.59) and pyrolyzed organic carbon (OPOS: 1.49, 1.12–1.99). The highest effects were seen in the winter for cough with sulfur (SOS: 2.28, 1.01–5.16) and wheeze with organic carbon fraction 2 (OC2OS: 7.46, 1.19–46.60). Our results indicate that exposure to components originating from outdoor sources of photochemistry, diesel and fuel oil combustion is associated with symptom’s exacerbation, especially in the winter. PM2.5 mass of indoor origin was more strongly associated with wheeze than with cough.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Abbreviations
- PM2.5:
-
particulate matter with aerodynamic diameter ≤2.5 μm
- PMIN:
-
indoor PM2.5 concentration
- PMIS:
-
indoor PM2.5 from indoor sources
- PMOS:
-
indoor PM2.5 from outdoor sources
- PMOUT:
-
outdoor PM2.5 concentration
References
Patel MM, Miller RL . Air pollution and childhood asthma: recent advances and future directions. Curr Opin Pediatr 2009; 21: 235–242.
Silverman RA, Ito K . Age-related association of fine particles and ozone with severe acute asthma in New York city. J Allergy Clin Immunol 2010; 125: 367–373.
Patel MM, Quinn JW, Jung KH, Hoepner L, Diaz D, Perzanowski M et al. Traffic density and stationary sources of air pollution associated with wheeze, asthma, and immunoglobulin E from birth to age 5 years among New York City children. Environ Res 2011; 111: 1222–1229.
Samoli E, Nastos PT, Paliatsos AG, Katsouyanni K, Priftis KN . Acute effects of air pollution on pediatric asthma exacerbation: evidence of association and effect modification. Environ Res 2011; 111: 418–424.
Delfino R, Zeiger R, Seltzer J, Street D, mclaren C . Association of asthma symptoms with peak particulate air pollution and effect modification by anti-inflammatory medication use. Environ Health Perspect 2002; 110: A607–A617.
Kelly FJ, Fussell JC . Size, source and chemical composition as determinants of toxicity attributable to ambient particulate matter. Atmos Environ 2012; 60: 504–526.
Schwartz J, Sarnat JA, Coull BA, Wilson WE . Effects of exposure measurement error on particle matter epidemiology: a simulation using data from a panel study in Baltimore, MD. J Expo Sci Environ Epidemiol 2007; 17: S2–S10.
Delfino R . Epidemiologic evidence for asthma and exposure to air toxics: linkages between occupational, indoor, and community air pollution research. Environ Health Perspect 2002; 110: 573–589.
Delfino R, Gong H, Linn W, Hu Y, Pellizzari E . Respiratory symptoms and peak expiratory flow in children with asthma in relation to volatile organic compounds in exhaled breath and ambient air. J Expo Anal Environ Epidemiol 2003; 13: 348–363.
Gent JF, Koutrakis P, Belanger K, Triche E, Holford TR, Bracken MB et al. Symptoms and medication use in children with asthma and traffic-related sources of fine particle pollution. Environ Health Perspect 2009; 117: 1168–1174.
Zeger S, Thomas D, Dominici F, Samet J, Schwartz J, Dockery D et al. Exposure measurement error in time-series studies of air pollution: concepts and consequences. Environ Health Perspect 2000; 108: 419–426.
Leaderer B, Naeher L, Jankun T, Balenger K, Holford T, Toth C et al. Indoor, outdoor, and regional summer and winter concentrations of PM10, PM2.5, SO42-, H+, NH4+, NO3-, NH3, and nitrous acid in homes with and without kerosene space heaters. Environ Health Perspect 1999; 107: 223–231.
Sarnat J, Long C, Koutrakis P, Coull B, Schwartz J, Suh H . Using sulfur as a tracer of outdoor fine particulate matter. Environ Sci Technol 2002; 36: 5305–5314.
Wallace L, Williams R . Use of personal-indoor-outdoor sulfur concentrations to estimate the infiltration factor and outdoor exposure factor for individual homes and persons. Environ Sci Technol 2005; 39: 1707–1714.
New York State Department of Health Asthma Emergency Department (ED) Visits—Rate per 10,000 Population, Age 5–14. 2011; Available at http://www.health.ny.gov/statistics/ny_asthma/ed/asthmaed1.htm Accessed 15 August 2012.
Kattan M, Gergen PJ, Eggleston P, Visness CM, Mitchell HE . Health effects of indoor nitrogen dioxide and passive smoking on urban asthmatic children. J Allergy Clin Immunol 2007; 120: 618–624.
Demokritou P, Kavouras I, Ferguson S, Koutrakis P . Development and laboratory performance evaluation of a personal multipollutant sampler for simultaneous measurements of particulate and gaseous pollutants. Aerosol Sci Technol 2001; 35: 741–752.
Liu L, Box M, Kalman D, Kaufman J, Koenig J, Larson T et al. Exposure assessment of particulate matter for susceptible populations in Seattle. Environ Health Perspect 2003; 111: 909–918.
Sarnat J, Brown K, Schwartz J, Coull B, Koutrakis P . Ambient gas concentrations and personal particulate matter exposures - Implications for studying the health effects of particles. Epidemiology 2005; 16: 385–395.
Yanosky J, Williams P, macintosh D . A comparison of two direct-reading aerosol monitors with the federal reference method for PM2.5 in indoor air. Atmos Environ 2002; 36: 107–113.
Demokritou P, Kavouras I, Harrison D, Koutrakis P . Development and evaluation of an impactor for a PM2.5 speciation sampler. J Air Waste Manage Assoc 2001; 51: 514–523.
Chow J, Watson J, Pritchett L, Pierson W, Frazier C, Purcell R . The dri thermal optical reflectance carbon analysis system—description, evaluation and applications in united-states air-quality studies. Atmos Environ Part A Gen Top 1993; 27: 1185–1201.
Sahu M, Hu S, Ryan PH, Le Masters G, Grinshpun SA, Chow JC et al. Chemical compositions and source identification of PM2.5 aerosols for estimation of a diesel source surrogate. Sci Total Environ 2011; 409: 2642–2651.
Allen R, Larson T, Sheppard L, Wallace L, Liu L . Use of real-time light scattering data to estimate the contribution of infiltrated and indoor-generated particles to indoor air. Environ Sci Technol 2003; 37: 3484–3492.
Sarnat J, Koutrakis P, Suh H . Assessing the relationship between personal particulate and gaseous exposures of senior citizens living in Baltimore, MD. J Air Waste Manage Assoc 2000; 50: 1184–1198.
SAS Institute Inc NC, USA. SAS.
R Development Core Team R 2.14.0 2011.
Qin Y, Kim E, Hopke PK . The concentrations and sources of PM2.5 in metropolitan New York city. Atmos Environ 2006; 40: S312–S332.
Sarnat JA, Brown KW, Bartell SM, Sarnat SE, Wheeler AJ, Suh HH et al. The relationship between averaged sulfate exposures and concentrations: results from exposure assessment panel studies in four US cities. Environ Sci Technol 2009; 43: 5028–5034.
Habre R, Coull B, Moshier E, Godbold J, Grunin A, Nath A et al. Sources of indoor air pollution in New York City residences of asthmatic children. J Expo Sci Environ Epidemiol 2013 advance online publication, 30 October 2013 doi:10.1038/jes.2013.74.
Mccormack MC, Breysse PN, Hansel NN, Matsui EC, Tonorezos ES, Curtin-Brosnan J et al. Common household activities are associated with elevated particulate matter concentrations in bedrooms of inner-city Baltimore pre-school children. Environ Res 2008; 106: 148–155.
Breysse P, Buckley T, Williams D, Beck C, Jo S, Merriman B et al. Indoor exposures to air pollutants and allergens in the homes of asthmatic children in inner-city Baltimore. Environ Res 2005; 98: 167–176.
Wallace L, Mitchell H, O'Connor G, Neas L, Lippmann M, Kattan M et al. Particle concentrations in inner-city homes of children with asthma: the effect of smoking, cooking, and outdoor pollution. Environ Health Perspect 2003; 111: 1265–1272.
Keeler G, Dvonch J, Yip F, Parker E, Israel B, Marsik F et al. Assessment of personal and community-level exposures to particulate matter among children with asthma in Detroit, Michigan, as part of Community Action Against Asthma (CAAA). Environ Health Perspect 2002; 110: 173–181.
Meng Q, Turpin B, Korn L, Weisel C, Morandi M, Colome S et al. Influence of ambient (outdoor) sources on residential indoor and personal PM2.5 concentrations: analyses of RIOPA data. J Expo Anal Environ Epidemiol 2005; 15: 17–28.
Patel MM, Hoepner L, Garfinkel R, Chillrud S, Reyes A, Quinn JW et al. Ambient metals, elemental carbon, and wheeze and cough in New York city children through 24 months of age. Am J Respir Crit Care Med 2009; 180: 1107–1113.
Lee SL, Wong WHS, Lau YL . Association between air pollution and asthma admission among children in Hong Kong. Clin Exp Allergy 2006; 36: 1138–1146.
Gent J, Triche E, Holford T, Belanger K, Bracken M, Beckett W et al. Association of low-level ozone and fine particles with respiratory symptoms in children with asthma. JAMA 2003; 290: 1859–1867.
Delfino R, Quintana P, Floro J, Gastanaga V, Samimi B, Kleinman M et al. Association of FEV1 in asthmatic children with personal and microenvironmental exposure to airborne particulate matter. Environ Health Perspect 2004; 112: 932–941.
Koenig J, Mar T, Allen R, Jansen K, Lumley T, Sullivan J et al. Pulmonary effects of indoor- and outdoor-generated particles in children with asthma. Environ Health Perspect 2005; 113: 499–503.
Goldstein I . Weather patterns and asthma epidemics in New-York-city and New-Orleans, USA. Int J Biometeorol 1980; 24: 329–339.
Ormstad H . Suspended particulate matter in indoor air: adjuvants and allergen carriers. Toxicology 2000; 152: 53–68.
Loymans RJB, ter Riet G, Sterk PJ . Definitions of asthma exacerbations. Curr Opin Allergy Clin Immunol 2011; 11: 181–186.
Busse WW, Morgan WJ, Gergen PJ, Mitchell HE, Gern JE, Liu AH et al. Randomized trial of omalizumab (anti-ige) for asthma in inner-city children. N Engl J Med 2011; 364: 1005–1015.
Kloepfer KM, Gern JE . Virus/allergen interactions and exacerbations of asthma. Immunol Allergy Clin North Am 2010; 30: 553–563.
Miyazaki Y, Kondo Y, Han S, Koike M, Kodama D, Komazaki Y et al. Chemical characteristics of water-soluble organic carbon in the Asian outflow. J Geophys Res Atmos 2007; 112: D22S30.
Kim E, Hopke P . Improving source apportionment of fine particles in the eastern United States utilizing temperature-resolved carbon fractions. J Air Waste Manage Assoc 2005; 55: 1456–1463.
Delfino RJ, Staimer N, Tjoa T, Arhami M, Polidori A, Gillen DL et al. Associations of primary and secondary organic aerosols with airway and systemic inflammation in an Elderly Panel Cohort. Epidemiology 2010; 21: 892–902.
Delfino RJ, Staimer N, Tjoa T, Gillen DL, Schauer JJ, Shafer MM . Airway inflammation and oxidative potential of air pollutant particles in a pediatric asthma panel. J Expo Sci Environ Epidemiol 2013; 23: 466–473.
Rohr A, Habre R, Godbold J, Moshier E, Schachter N, Kattan M et al. Asthma exacerbation is associated with particulate matter source factors in children in New York city. Air Qual Atmos Health, advance online publication, 4 January 2014 doi:10.1007/s11869-013-0230-y.
Sarnat JA, Marmur A, Klein M, Kim E, Russell AG, Sarnat SE et al. Fine particle sources and cardiorespiratory morbidity: an application of chemical mass balance and factor analytical source-apportionment methods. Environ Health Perspect 2008; 116: 459–466.
EPA Speciate database: Bromine. Available at http://cfpub.epa.gov/si/speciate/ehpa_speciate_browse.cfm?Ptype=P&pollutant=3072013.
Peltier RE, Lippmann M . Residual oil combustion: 2. Distributions of airborne nickel and vanadium within New York City. J Expo Sci Environ Epidemiol 2010; 20: 342–350.
Saldiva P, Clarke R, Coull B, Stearns R, Lawrence J, Murthy G et al. Lung inflammation induced by concentrated ambient air particles is related to particle composition. Am J Respir Crit Care Med 2002; 165: 1610–1617.
Hirshon JM, Shardell M, Alles S, Powell JL, Squibb K, Ondov J et al. Elevated ambient air zinc increases pediatric asthma morbidity. Environ Health Perspect 2008; 116: 826–831.
Acknowledgements
This study was supported by the Electric Power Research Institute (EP-P15909/C7932). R Habre was supported by the Harvard School of Public Health Dean’s Scholarship. We thank Tom Gentile, George O’Connor and Lance Wallace, members of the CAPAS study scientific advisory committee, for their guidance in all phases of the study. Stephen Ferguson and Mike Wolfson are also acknowledged for designing the air sampling monitors and conducting laboratory analyses. We also thank all the individuals who participated in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
AR is employed by the Electric Power Research Institute, which is primarily supported by the electric industry in the United States and abroad. EPRI is an independent non-profit 501(c)(3) organization that funds external research at a number of universities and institutes worldwide. All the other authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Journal of Exposure Science and Environmental Epidemiology website
Supplementary information
Rights and permissions
About this article
Cite this article
Habre, R., Moshier, E., Castro, W. et al. The effects of PM2.5 and its components from indoor and outdoor sources on cough and wheeze symptoms in asthmatic children. J Expo Sci Environ Epidemiol 24, 380–387 (2014). https://doi.org/10.1038/jes.2014.21
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jes.2014.21
Keywords
This article is cited by
-
Differential patterns of association between PM1 and PM2.5 with symptoms of attention deficit hyperactivity disorder
Nature Mental Health (2023)
-
An assessment of four decades atmospheric PM2.5 trends in urban locations over Southern Africa using MERRA-2 reanalysis
Air Quality, Atmosphere & Health (2023)
-
Lias overexpression alleviates pulmonary injury induced by fine particulate matter in mice
Environmental Geochemistry and Health (2023)
-
Fine particulate matter constituents associated with emergency room visits for pediatric asthma: a time-stratified case–crossover study in an urban area
BMC Public Health (2021)
-
Respiratory function declines in children with asthma associated with chemical species of fine particulate matter (PM2.5) in Nagasaki, Japan
Environmental Health (2021)