Abstract
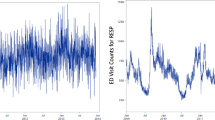
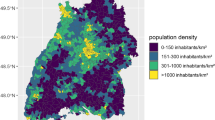
Various temporal metrics of daily pollution levels have been used to examine the relationships between air pollutants and acute health outcomes. However, daily metrics of the same pollutant have rarely been systematically compared within a study. In this analysis, we describe the variability of effect estimates attributable to the use of different temporal metrics of daily pollution levels. We obtained hourly measurements of ambient particulate matter (PM2.5), carbon monoxide (CO), nitrogen dioxide (NO2), and ozone (O3) from air monitoring networks in 20-county Atlanta for the time period 1993–2004. For each pollutant, we created (1) a daily 1-h maximum; (2) a 24-h average; (3) a commute average; (4) a daytime average; (5) a nighttime average; and (6) a daily 8-h maximum (only for O3). Using Poisson generalized linear models, we examined associations between daily counts of respiratory emergency department visits and the previous day's pollutant metrics. Variability was greatest across O3 metrics, with the 8-h maximum, 1-h maximum, and daytime metrics yielding strong positive associations and the nighttime O3 metric yielding a negative association (likely reflecting confounding by air pollutants oxidized by O3). With the exception of daytime metric, all of the CO and NO2 metrics were positively associated with respiratory emergency department visits. Differences in observed associations with respiratory emergency room visits among temporal metrics of the same pollutant were influenced by the diurnal patterns of the pollutant, spatial representativeness of the metrics, and correlation between each metric and copollutant concentrations. Overall, the use of metrics based on the US National Ambient Air Quality Standards (for example, the use of a daily 8-h maximum O3 as opposed to a 24-h average metric) was supported by this analysis. Comparative analysis of temporal metrics also provided insight into underlying relationships between specific air pollutants and respiratory health.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Bell M.L., Hobbs B.F., and Ellis H. Metrics matter: conflicting air quality rankings from different indices of air pollution. J Air Waste Manag Assoc 2005: 55 (1): 97–106.
Delfino R.J., Zeiger R.S., Seltzer J.M., and Street D.H. Symptoms in pediatric asthmatics and air pollution: differences in effects by symptom severity, anti-inflammatory medication use and particulate averaging time. Environ Health Perspect 1998: 106 (11): 751–761.
Delfino R.J., Zeiger R.S., Seltzer J.M., Street D.H., and McLaren C.E. Association of asthma symptoms with peak particulate air pollution and effect modification by anti-inflammatory medication use. Environ Health Perspect 2002: 110 (10): A607–A617.
Hansen D.A., Edgerton E., Hartsell B., Jansen J., Burge H., Koutrakis P., Rogers C., Suh H., Chow J., Zielinska B., McMurry P., Mulholland J., Russell A., and Rasmussen R. Air quality measurements for the aerosol research and inhalation epidemiology study. J Air Waste Manag Assoc 2006: 56 (10): 1445–1458.
Ito K., Thurston G.D., Nadas A., and Lippmann M. Monito-to-monitor temporal correlation of air pollution and weather variables in the North-Central US. J Expo Sci Environ Epidemiol 2001: 11 (1): 21–32.
Lokken R.P., Wellenius G.A., Coull B.A., Burger M.R., Schlaug G., Suh H.H., and Mittleman M.A. Air pollution and risk of stroke: underestimation of effect due to misclassification of time of event onset. Epidemiology 2009: 20 (1): 137–142.
Lu Y., and Zeger S.L. On the equivalence of case-crossover and time series methods in environmental epidemiology. Biostatistics 2007: 8 (2): 337–344.
Metzger K.B., Tolbert P.E., Klein M., Peel J.L., Flanders W.D., Todd K., Mulholland J.A., Ryan P.B., and Frumkin H. Ambient air pollution and cardiovascular emergency department visits. Epidemiology 2004: 15 (1): 46–56.
Ostro B., Lipsett M., Mann J., Braxton-Owens H., and White M. Air pollution and exacerbation of asthma in African-American children in Los Angeles. Epidemiology 2001: 12 (2): 200–208.
Peel J.L., Tolbert P.E., Klein M., Metzger K.B., Flanders W.D., Todd K., Mulholland J.A., Ryan P.B., and Frumkin H. Ambient air pollution and respiratory emergency department visits. Epidemiology 2005: 16 (2): 164–174.
Sarnat J.A., Marmur A., Klein M., Kim E., Russell A.G., Sarnat S.E., Mulholland J.A., Hopke P.K., and Tolbert P.E. Fine particle sources and cardiorespiratory morbidity: an application of chemical mass balance and factor analytical source-apportionment methods. Environ Health Perspect 2008: 116 (4): 459–466.
Sarnat J.A., Schwartz J., Catalano P.J., and Suh H.H. Gaseous pollutants in particulate matter epidemiology: confounders or surrogates? Environ Health Perspect 2001: 109 (10): 1053–1061.
Sarnat S.E., Klein M., Sarnat J.A., Mulholland J., Flanders W.D., Waller L.A., Russell A.G., and Tolbert P.E. An examination of exposure measurement error from air pollutant spatial variability in time-series studies. J Expo Sci Environ Epidemiol, advance online publication, March 11, 2009; doi:10.1038/jes.2009.10.
Schwartz J. The effects of particulate air pollution on daily deaths: a multi-city case crossover analysis. Occup Environ Med 2004: 61 (12): 956–961.
Schwartz J. How sensitive is the association between ozone and daily deaths to control for temperature? Am J Respir Crit Care Med 2005: 171 (6): 627–631.
Sunyer J., Spix C., Quénel P., Ponce-de-León A., Pönka A., Barumandzadeh T., Touloumi G., Bacharova L., Wojtyniak B., Vonk J., Bisanti L., Schwartz J., and Katsouyanni K. Urban air pollution and emergency admissions for asthma in four European cities: the APHEA Project. Thorax 1997: 52 (9): 760–765.
Tolbert P.E., Klein M., Peel J.L., Sarnat S.E., and Sarnat J.A. Multipollutant modeling issues in a study of ambient air quality and emergency department visits in Atlanta. J Expo Sci Environ Epidemiol 2007: 17 (Suppl 2): S29–S35.
Van Loy M., Bahadori T., Wyzga R., Hartsell B., and Edgerton E. Aerosol Research and Inhalation Epidemiology Study (ARIES): PM2.5 mass and aerosol component concentrations and sampler intercomparisons. J Air Waste Manage Assoc 2000: 50: 1446–1458.
Wade K.S., Mulholland J.A., Marmur A., Russell A.G., Hartsell E.E., Edgerton E., Klein M., Waller L., Peel J.L., and Tolbert P.E. Effect of instrument precision and spatial variability on the assessment of the temporal variation of ambient air pollution in Atlanta, Georgia. J Air Waste Manage Assoc 2006: 56: 876–888.
Zanobetti A., and Schwartz J. Air pollution and emergency admissions in Boston, MA. J Epidemiol Community Health 2006: 60 (10): 890–895.
Zmirou D., Schwartz J., Saez M., Zanobetti A., Wojtyniak B., Touloumi G., Spix C., Ponce de León A., Le Moullec Y., Bacharova L., Schouten J., Pönkä A., and Katsouyanni K. Time-series analysis of air pollution and cause-specific mortality. Epidemiology 1998: 9 (5): 495–503.
Acknowledgements
This work was supported by grants from the Electric Power Research Institute (EP-P27723/C13172), the US Environmental Protection Agency (CR-83407301-0, RD833626, R82921301-0), and the National Institute of Environmental Health Sciences (R01ES11294).
Author information
Authors and Affiliations
Corresponding author
Additional information
Supplementary Information accompanies the paper on the Journal of Exposure Science and Environmental Epidemiology website
Supplementary information
Rights and permissions
About this article
Cite this article
Darrow, L., Klein, M., Sarnat, J. et al. The use of alternative pollutant metrics in time-series studies of ambient air pollution and respiratory emergency department visits. J Expo Sci Environ Epidemiol 21, 10–19 (2011). https://doi.org/10.1038/jes.2009.49
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jes.2009.49
Keywords
This article is cited by
-
Effect modification by high-concentration duration in the association between particulate matters and stroke hospital admissions among hypertension patients in Beijing, China
Air Quality, Atmosphere & Health (2023)
-
Short-term effects of multiple ozone metrics on outpatient visits for urticaria in Lanzhou, China
Stochastic Environmental Research and Risk Assessment (2022)
-
Relationship between different air pollutants and total and cause-specific emergency ambulance dispatches in Shanghai, China
International Archives of Occupational and Environmental Health (2021)
-
Ambient air pollution and emergency department visits for asthma in Erie County, New York 2007–2012
International Archives of Occupational and Environmental Health (2018)
-
Short-term effects of multiple ozone metrics on daily mortality in a megacity of China
Environmental Science and Pollution Research (2015)