Abstract
Background:
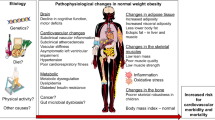
A proportion of obese subjects appear metabolically healthy (MHO) but little is known about the natural history of MHO and factors predicting its future conversion to metabolically unhealthy obese (MUO).
Objectives:
The aim was to determine prospectively the frequency of conversion of MHO to MUO and the clinical variables that independently predicted this conversion, with a particular focus on the role of body composition.
Methods:
We identified 85 Japanese Americans with MHO (56 men, 29 women), aged 34–73 years (mean age 49.8 years) who were followed at 2.5, 5 and 10 years after enrollment with measurements of metabolic characteristics, lifestyle and abdominal and thigh fat areas measured by computed tomography. Obesity was defined using the Asian body mass index criterion of ⩾25 kg m−2. Metabolically healthy was defined as the presence of ⩽2 of 5 metabolic syndrome components proposed by the National Cholesterol Education Program Adult Treatment Panel III, while metabolically unhealthy was defined as ⩾3 components.
Results:
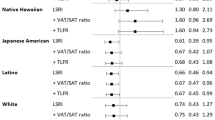
Over 10 years of follow-up, 55 MHO individuals (64.7%) converted to MUO. Statistically significant univariate predictors of conversion included dyslipidemia, greater insulin resistance and greater visceral abdominal (VAT) and subcutaneous abdominal fat area (SAT). In multivariate analysis, VAT (odds ratio per 1-s.d. increment (95% confidence interval) 2.04 (1.11–3.72), P=0.021), high-density lipoprotein (HDL) cholesterol (0.24 (0.11–0.53), P<0.001), fasting plasma insulin (2.45 (1.07–5.62), P=0.034) and female sex (5.37 (1.14–25.27), P=0.033) were significantly associated with future conversion to MUO. However, SAT was not an independent predictor for future conversion to MUO.
Conclusions:
In this population, MHO was a transient state, with nearly two-thirds developing MUO over 10 years, with higher conversion to MUO independently associated with VAT, female sex, higher fasting insulin level and lower baseline HDL cholesterol level.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Bauer UE, Briss PA, Goodman RA, Bowman BA . Prevention of chronic disease in the 21st century: elimination of the leading preventable causes of premature death and disability in the USA. Lancet 2014; 384: 45–52.
Stefan N, Kantartzis K, Machann J, Schick F, Thamer C, Rittig K et al. Identification and characterization of metabolically benign obesity in humans. Arch Intern Med 2008; 168: 1609–1616.
Wildman RP, Muntner P, Reynolds K, McGinn AP, Rajpathak S, Wylie-Rosett J et al. The obese without cardiometabolic risk factor clustering and the normal weight with cardiometabolic risk factor clustering: prevalence and correlates of 2 phenotypes among the US population (NHANES 1999–2004). Arch Intern Med 2008; 168: 1617–1624.
Blüher M . Are there still healthy obese patients? Curr Opin Endocrinol Diabetes Obes 2012; 19: 341–346.
Phillips CM . Metabolically healthy obesity: definitions, determinants and clinical implications. Rev Endocr Metab Disord 2013; 14: 219–227.
Primeau V, Coderre L, Karelis AD, Brochu M, Lavoie ME, Messier V et al. Characterizing the profile of obese patients who are metabolically healthy. Int J Obes (Lond) 2011; 35: 971–981.
Appleton SL, Seaborn CJ, Visvanathan R, Hill CL, Gill TK, Taylor AW et al. Diabetes and cardiovascular disease outcomes in the metabolically healthy obese phenotype: a cohort study. Diabetes Care 2013; 36: 2388–2394.
Kramer CK, Zinman B, Retnakaran R . Are metabolically healthy overweight and obesity benign conditions? A systematic review and meta-analysis. Ann Intern Med 2013; 159: 758–769.
Fujimoto WY, Leonetti DL, Kinyoun JL, Shuman WP, Stolov WC, Wahl PW . Prevalence of complications among second-generation Japanese-American men with diabetes, impaired glucose tolerance, or normal glucose tolerance. Diabetes 1987; 36: 730–739.
Fujimoto WY, Bergstrom RW, Leonetti DL, Newell-Morris LL, Shuman WP, Wahl PW . Metabolic and adipose risk factors for NIDDM and coronary disease in third-generation Japanese-American men and women with impaired glucose tolerance. Diabetologia 1994; 37: 524–532.
Paffenbarger RS, Wing AL, Hyde RT . Physical activity as an index of heart attack risk in college alumni. Am J Epidemiol 1978; 108: 161–175.
Tsunehara CH, Leonetti DL, Fujimoto WY . Diet of second-generation Japanese-American men with and without non-insulin-dependent diabetes. Am J Clin Nutr 1990; 52: 731–738.
Bergstrom RW, Leonetti DL, Newell-Morris LL, Shuman WP, Wahl PW, Fujimoto WY . Association of plasma triglyceride and C-peptide with coronary heart disease in Japanese-American men with a high prevalence of glucose intolerance. Diabetologia 1990; 33: 489–496.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC . Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985; 28: 412–419.
Shuman WP, Morris LL, Leonetti DL, Wahl PW, Moceri WM, Moss AA et al. Abnormal body fat distribution detected by computed tomography in diabetic men. Invest Radiol 1986; 21: 483–487.
Grundy SM, Brewer HB Jr, Cleeman JI, Smith SC Jr, Lenfant C, American Heart Association: National Heart, Lung, and Blood Institute. Definition of metabolic syndrome: Report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation 2004; 109: 433–438.
Alberti KG, Zimmet P, Shaw J, IDF Epidemiology Task Force Consensus Group. The metabolic syndrome—a new worldwide definition. Lancet 2005; 366: 1059–1062.
World Health Organization The Asia-Pacific perspective: redefining obesity and its treatment. WHO: Geneva, Switzerland, 2000.
Meigs JB, Wilson PW, Fox CS, Vasan RS, Nathan DM, Sullivan LM et al. Body mass index, metabolic syndrome, and risk of type 2 diabetes or cardiovascular disease. J Clin Endocrinol Metab 2006; 91: 2906–2912.
Hamer M, Stamatakis E . Metabolically healthy obesity and risk of all-cause and cardiovascular disease mortality. J Clin Endocrinol Metab 2012; 97: 2482–2488.
Arnlov J, Ingelsson E, Sundstrom J, Lind L . Impact of body mass index and the metabolic syndrome on the risk of cardiovascular disease and death in middle-aged men. Circulation 2010; 121: 230–236.
Kuk JL, Ardern CI . Are metabolically normal but obese individuals at lower risk for all-cause mortality? Diabetes Care 2009; 32: 2297–2299.
Soriguer F, Gutiérrez-Repiso C, Rubio-Martín E, García-Fuentes E, Almaraz MC, Colomo N et al. Metabolically healthy but obese, a matter of time? Findings from the prospective Pizarra study. J Clin Endocrinol Metab 2013; 98: 2318–2325.
van der A DL, Nooyens AC, van Duijnhoven FJ, Verschuren MM, Boer JM . All-cause mortality risk of metabolically healthy abdominal obese individuals: the EPIC-MORGEN study. Obesity (Silver Spring) 2014; 22: 557–564.
Bell JA, Kivimaki M, Hamer M . Metabolically healthy obesity and risk of incident type 2 diabetes: a meta-analysis of prospective cohort studies. Obes Rev 2014; 15: 504–515.
Koster A, Stenholm S, Alley DE, Kim LJ, Simonsick EM, Kanaya AM et al. Body fat distribution and inflammation among obese older adults with and without metabolic syndrome. Obesity (Silver Spring) 2010; 18: 2354–2361.
Kim TN, Park MS, Yang SJ, Yoo HJ, Kang HJ, Song W et al. Body size phenotypes and low muscle mass: the Korean sarcopenic obesity study (KSOS). J Clin Endocrinol Metab 2013; 98: 811–817.
Snijder MB, Visser M, Dekker JM, Goodpaster BH, Harris TB, Kritchevsky SB et al. Low subcutaneous thigh fat is a risk factor for unfavourable glucose and lipid levels, independently of high abdominal fat. The Health ABC Study. Diabetologia 2005; 48: 301–308.
Fox CS, Massaro JM, Hoffmann U, Pou KM, Maurovich-Horvat P, Liu CY et al. Abdominal visceral and subcutaneous adipose tissue compartments: association with metabolic risk factors in the Framingham Heart Study. Circulation 2007; 116: 39–48.
Ford ES, Giles WH, Dietz WH . Prevalence of the metabolic syndrome among US adults: findings from the third National Health and Nutrition Examination Survey. JAMA 2002; 287: 356–359.
Lear SA, Humphries KH, Kohli S, Chockalingam A, Frohlich JJ, Birmingham CL . Visceral adipose tissue accumulation differs according to ethnic background: results of the Multicultural Community Health Assessment Trial (M-CHAT). Am J Clin Nutr 2007; 86: 353–359.
Golan R, Shelef I, Rudich A, Gepner Y, Shemesh E, Chassidim Y et al. Abdominal superficial subcutaneous fat: a putative distinct protective fat subdepot in type 2 diabetes. Diabetes Care 2012; 35: 640–647.
Acknowledgements
This work was supported by facilities and services provided by the Diabetes Research Center (DK-17047), Clinical Nutrition Research Unit (DK-35816), and the General Clinical Research Center (RR-00037) at the University of Washington. VA Puget Sound Health Care System provided support for Drs Boyko and Kahn’s involvement in this research. We are grateful to the King County Japanese American community for support and cooperation. Funding was through National Institutes of Health grants DK-31170, HL-49293 and DK-017047. The funding entities had no role in the conduct of this study or interpretation of its results.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Hwang, YC., Hayashi, T., Fujimoto, W. et al. Visceral abdominal fat accumulation predicts the conversion of metabolically healthy obese subjects to an unhealthy phenotype. Int J Obes 39, 1365–1370 (2015). https://doi.org/10.1038/ijo.2015.75
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2015.75
This article is cited by
-
Metabolic health's central role in chronic kidney disease progression: a 20-year study of obesity-metabolic phenotype transitions
Scientific Reports (2024)
-
Joint effect of BMI and metabolic status on mortality among adults: a population-based longitudinal study in United States
Scientific Reports (2024)
-
Comprehensive transcriptomics and metabolomics analyses reveal that hyperhomocysteinemia is a high risk factor for coronary artery disease in a chinese obese population aged 40–65: a prospective cross-sectional study
Cardiovascular Diabetology (2023)
-
A novel visceral adiposity index predicts bone loss in female early rheumatoid arthritis patients detected by HR-pQCT
Scientific Reports (2023)
-
Positive Association Between the Chinese Visceral Adiposity Index and Nonalcoholic Fatty Liver Disease in Lean Adults
Digestive Diseases and Sciences (2023)