Abstract
Background/Objectives:
Antibiotics are commonly prescribed for children. Use of antibiotics early in life has been linked to weight gain but there are no large-scale, population-based, longitudinal studies of the full age range among mainly healthy children.
Subjects/Methods:
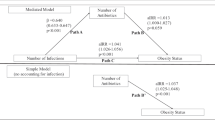
We used electronic health record data on 163 820 children aged 3–18 years and mixed effects linear regression to model associations of antibiotic orders with growth curve trajectories of annual body mass index (BMI) controlling for confounders. Models evaluated three kinds of antibiotic associations—reversible (time-varying indicator for an order in year before each BMI), persistent (time-varying cumulative orders up to BMIj) and progressive (cumulative orders up to prior BMI (BMIj-1))—and whether these varied by age.
Results:
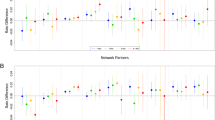
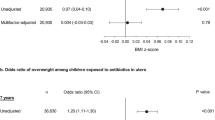
Among 142 824 children under care in the prior year, a reversible association was observed and this short-term BMI gain was modified by age (P<0.001); effect size peaked in mid-teen years. A persistent association was observed and this association was stronger with increasing age (P<0.001). The addition of the progressive association among children with at least three BMIs (n=79 752) revealed that higher cumulative orders were associated with progressive weight gain; this did not vary by age. Among children with an antibiotic order in the prior year and at least seven lifetime orders, antibiotics (all classes combined) were associated with an average weight gain of approximately 1.4 kg at age 15 years. When antibiotic classes were evaluated separately, the largest weight gain at 15 years was associated with macrolide use.
Conclusions:
We found evidence of reversible, persistent and progressive effects of antibiotic use on BMI trajectories, with different effects by age, among mainly healthy children. The results suggest that antibiotic use may influence weight gain throughout childhood and not just during the earliest years as has been the primary focus of most prior studies.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Moore PR, Evenson A, Luckey TD, McCoy E, Elvehjem CA, Hart EB . Use of sulfasuxidine, streptothricin, and streptomycin in nutritional studies with the chick. J Biol Chem 1946; 165: 437–441.
Stokstad ELR, Jukes TH, Pierce J, Page J, Franklin AC . AL. The multiple nature of the animal protein factor. J Biol Chem 1949; 180: 647–654.
Jukes TH . Antibiotics in animal feeds and animal production. Bioscience 1972; 22: 526.
Kiser JS . Perspective on use of antibiotics in animal feeds. J Anim Sci 1976; 42: 1058–1071.
Butaye P, Devriese LA, Haesebrouck F . Antimicrobial growth promoters used in animal feed: effects of less well known antibiotics on gram-positive bacteria. Clin Microbiol Rev 2003; 16: 175–188.
Turnbaugh PJ, Hamady M, Yatsunenko T, Cantarel BL, Duncan A, Ley RE et al. A core gut microbiome in obese and lean twins. Nature 2009; 457: 480–484.
Ley RE, Turnbaugh PJ, Klein S, Gordon JI . Microbial ecology: human gut microbes associated with obesity. Nature 2006; 444: 1022–1023.
Santacruz A, Marcos A, Warnberg J, Marti A, Martin-Matillas M, Campoy C et al. Interplay between weight loss and gut microbiota composition in overweight adolescents. Obesity (Silver Spring) 2009; 17: 1906–1915.
Zhang H, DiBaise JK, Zuccolo A, Kudrna D, Braidotti M, Yu Y et al. Human gut microbiota in obesity and after gastric bypass. Proc Natl Acad Sci USA 2009; 106: 2365–2370.
Angelakis E, Merhej V, Raoult D . Related actions of probiotics and antibiotics on gut microbiota and weight modification. Lancet Infect Dis 2013; 13: 889–899.
Schwiertz A, Taras D, Schafer K, Beijer S, Bos NA, Donus C et al. Microbiota and SCFA in lean and overweight healthy subjects. Obesity (Silver Spring) 2010; 18: 190–195.
Million M, Lagier JC, Yahav D, Paul M . Gut bacterial microbiota and obesity. Clin Microbiol Infect 2013; 19: 305–313.
Macfarlane S . Antibiotic treatments and microbes in the gut. Environ Microbiol 2014; 16: 919–924.
Riley LW, Raphael E, Faerstein E . Obesity in the United States - dysbiosis from exposure to low-dose antibiotics? Front Public Health 2013; 1: 69.
Turnbaugh PJ, Ley RE, Mahowald MA, Magrini V, Mardis ER, Gordon JI . An obesity-associated gut microbiome with increased capacity for energy harvest. Nature 2006; 444: 1027–1031.
Harris K, Kassis A, Major G, Chou CJ . Is the gut microbiota a new factor contributing to obesity and its metabolic disorders? J Obes 2012; 2012: 879151.
Dethlefsen L, Huse S, Sogin ML, Relman DA . The pervasive effects of an antibiotic on the human gut microbiota, as revealed by deep 16 S rRNA sequencing. PLoS Biol 2008; 6: e280.
De La Cochetiere MF, Durand T, Lepage P, Bourreille A, Galmiche JP, Dore J . Resilience of the dominant human fecal microbiota upon short-course antibiotic challenge. J Clin Microbiol 2005; 43: 5588–5592.
Robinson CJ, Young VB . Antibiotic administration alters the community structure of the gastrointestinal micobiota. Gut Microbes 2010; 1: 279–284.
Robinson CJ, Bohannan BJ, Young VB . From structure to function: the ecology of host-associated microbial communities. Microbiol Biol Rev 2010; 74: 453–476.
Dethlefsen L, Relman DA . Incomplete recovery and individualized responses of the human distal gut microbiota to repeated antibiotic perturbation. Proc Natl Acad Sci USA 2011; 108: 4554–4561.
Jernberg C, Lofmark S, Edlund C, Jansson JK . Long-term impacts of antibiotic exposure on the human intestinal microbiota. Microbiology 2010; 156: 3216–3223.
Jernberg C, Lofmark S, Edlund C, Jansson JK . Long-term ecological impacts of antibiotic administration on the human intestinal microbiota. ISME J 2007; 1: 56–66.
Martin MA, Sela DA. Infant gut microbiota: developmental influences and health outcomes. In: Clancy KBH, Hinde K, Rutherford JN (eds). Building Babies: Primate Development in Proximate and Ultimate Perspective. Spring Science+Business Media: New York, NY, USA, 2011; 233–256.
Trasande L, Blustein J, Liu M, Corwin E, Cox LM, Blaser MJ . Infant antibiotic exposures and early-life body mass. Int J Obes (Lond) 2013; 37: 16–23.
Lane JA, Murray LJ, Harvey IM, Donovan JL, Nair P, Harvey RF . Randomised clinical trial: helicobacter pylori eradication is associated with a significantly increased body mass index in a placebo-controlled study. Aliment Pharmacol Ther 2011; 33: 922–929.
Schwartz BS, Bailey-Davis L, Bandeen-Roche K, Pollak J, Hirsch AG, Nau C et al. Attention deficit disorder, stimulant use, and childhood body mass index trajectory. Pediatrics 2014; 133: 668–676.
Liu AY, Curriero FC, Glass TA, Stewart WF, Schwartz BS . The contextual influence of coal abandoned mine lands in communities and type 2 diabetes in Pennsylvania. Health Place 2013; 22: 115–122.
Casey JA, Curriero FC, Cosgrove SE, Nachman KE, Schwartz BS . High-density livestock operations, crop field Aapplication of manure, and risk of community-associated methicillin-resistant staphylococcus aureus infection in pennsylvania. JAMA Int Med 2013; 173: 1980–1990.
Casey JA, Cosgrove SE, Stewart WF, Pollak J, Schwartz BS . A population-based study of the epidemiology and clinical features of methicillin-resistant Staphylococcus aureus infection in Pennsylvania, 2001-2010. Epidemiol Infect 2013; 141: 1166–1179.
Schwartz BS, Stewart WF, Godby S, Pollak J, Dewalle J, Larson S et al. Body mass index and the built and social environments in children and adolescents using electronic health records. Am J Prev Med 2011; 41: e17–e28.
Medi-Span Master Drug Data Base Documentation Manual. Medi-Span: Indianapolis, IN, USA, 2007.
Berkey CS, Colditz GA . Adiposity in adolescents: change in actual BMI works better than change in BMI z score for longitudinal studies. Ann Epidemiol 2007; 17: 44–50.
Cole TJ, Faith MS, Pietrobelli A, Heo M . What is the best measure of adiposity change in growing children: BMI, BMI %, BMI z-score or BMI centile? Eur J Clin Nutr 2005; 59: 419–425.
Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z et al. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat 11 2002: 1–190.
Bandeen-Roche K, Hall CB, Stewart WF, Zeger SL . Modelling disease progression in terms of exposure history. Stat Med 1999; 18: 2899–2916.
Cleveland WS . Robust locally weighted regression and smoothing scatterplots. J Am Stat Assoc 1979; 74: 829–836.
Seber GAF Linear Regression Analysis. Wiley: New York, NY, USA, 1977.
Munyaka PM, Khafipour E, Ghia JE . External influence of early childhood establishment of gut microbiota and subsequent health implications. Front Pediatr 2014; 2: 109.
Goedert JJ, Hua X, Yu G, Shi J . Diversity and composition of the adult fecal microbiome associated with history of cesarean birth or appendectomy: analysis of the American Gut Project. EBioMedicine 2014; 1: 167–172.
Mueller NT, Whyatt R, Hoepner L, Oberfield S, Dominguez-Bello MG, Widen EM et al. Prenatal exposure to antibiotics, cesarean section and risk of childhood obesity. Int J Obes (Lond) 2015; 39: 665–670.
Blustein J, Attina T, Liu M, Ryan AM, Cox LM, Blaser MJ et al. Association of caesarean delivery with child adiposity from age 6 weeks to 15 years. Int J Obes (Lond) 2013; 37: 900–906.
Li HT, Zhou YB, Liu JM . The impact of cesarean section on offspring overweight and obesity: a systematic review and meta-analysis. Int J Obes (Lond) 2013; 37: 893–899.
Hersh AL, Jackson MA, Hicks LA . Principles of judicious antibiotic prescribing for upper respiratory tract infections in pediatrics. Pediatrics 2013; 132: 1146–1154.
Hersh AL, Shapiro DJ, Pavia AT, Shah SS . Antibiotic prescribing in ambulatory pediatrics in the United States. Pediatrics 2011; 128: 1053–1061.
Bailey LC, Forrest CB, Zhang P, Richards TM, Livshits A, DeRusso PA . Association of Antibiotics in Infancy With Early Childhood Obesity. JAMA Pediatr 2014; 168: 1063–1069.
Ajslev TA, Andersen CS, Gamborg M, Sorensen TI, Jess T . Childhood overweight after establishment of the gut microbiota: the role of delivery mode, pre-pregnancy weight and early administration of antibiotics. Int J Obes (Lond) 2011; 35: 522–529.
Ray K . Gut microbiota: adding weight to the microbiota's role in obesity—exposure to antibiotics early in life can lead to increased adiposity. Nat Rev Gastroenterol Hepatol 2012; 9: 615.
Mansi Y, Abdelaziz N, Ezzeldin Z, Ibrahim R . Randomized controlled trial of a high dose of oral erythromycin for the treatment of feeding intolerance in preterm infants. Neonatology 2011; 100: 290–294.
Trehan I, Goldbach HS, LaGrone LN, Meuli GJ, Wang RJ, Maleta KM et al. Antibiotics as part of the management of severe acute malnutrition. N Engl J Med 2013; 368: 425–435.
Smith MI, Yatsunenko T, Manary MJ, Trehan I, Mkakosya R, Cheng J et al. Gut microbiomes of Malawian twin pairs discordant for kwashiorkor. Science 2013; 339: 548–554.
Guzman MA, Scrimshaw NS, Monroe RJ . Growth and development of Central American children. I. Growth responses of rural Guatemalan school children to daily administration of penicillin and aureomycin. Am J Clin Nutr 1958; 6: 430–438.
Lozupone CA, Stombaugh JI, Gordon JI, Jansson JK, Knight R . Diversity, stability and resilience of the human gut microbiota. Nature 2012; 489: 220–230.
Jakobsson HE, Jernberg C, Andersson AF, Sjolund-Karlsson M, Jansson JK, Engstrand L . Short-term antibiotic treatment has differing long-term impacts on the human throat and gut microbiome. Plos One 2010; 5: e9836.
Agans R, Rigsbee L, Kenche H, Michail S, Khamis HJ, Paliy O . Distal gut microbiota of adolescent children is different from that of adults. FEMS Microbiol Ecol 2011; 77: 404–412.
U.S. Department of Agriculture Agricultural Research Service. Energy Intakes: Percentages of Energy from Protein, Carbohydrate, Fat, and Alcohol, by Gender and Age, What We Eat in America, NHANES 2009–2010. 2012; www.ars.usda.gov/ba/bhnrc/fsrg (accessed 8 August 2014).
Arora T, Sharma R . Fermentation potential of the gut microbiome: implications for energy homeostasis and weight management. Nutr Rev 2011; 69: 99–106.
Barker DJ . Obesity and early life. Obes Rev 2007; 8: 45–49.
Huang TT, Drewnosksi A, Kumanyika S, Glass TA . A systems-oriented multilevel framework for addressing obesity in the 21st century. Prev Chronic Dis 2009; 6: A82.
Ludwig DS, Gortmaker SL . Programming obesity in childhood. Lancet 2004; 364: 226–227.
Acknowledgements
The project described was supported by Grant Number U54 HD-070725 from the Eunice Kennedy Shriver National Institute of Child Health & Human Development (NICHD). The project is co-funded by the NICHD and the Office of Behavioral and Social Sciences Research (OBSSR). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Schwartz, B., Pollak, J., Bailey-Davis, L. et al. Antibiotic use and childhood body mass index trajectory. Int J Obes 40, 615–621 (2016). https://doi.org/10.1038/ijo.2015.218
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2015.218
This article is cited by
-
The impact of early-life antibiotics and probiotics on gut microbial ecology and infant health outcomes: a Pregnancy and Birth Cohort in Northwest China (PBCC) study protocol
BMC Pediatrics (2022)
-
Antibiotics prior to age 2 years have limited association with preschool growth trajectory
International Journal of Obesity (2022)
-
Early childhood infections and body mass index in adolescence
International Journal of Obesity (2021)
-
Neonatal antibiotic exposure impairs child growth during the first six years of life by perturbing intestinal microbial colonization
Nature Communications (2021)
-
Impact of probiotics supplement on the gut microbiota in neonates with antibiotic exposure: an open-label single-center randomized parallel controlled study
World Journal of Pediatrics (2021)