Abstract
Background:
We performed a 5-year multicenter study to evaluate the safety and effectiveness of the LAP-BAND System surgery (LBS) in patients with obesity with a body mass index (BMI) of 30–39.9 kg m−2. This pivotal study was designed to support LBS application to the US Food and Drug Administration for broadening the indications for surgery and the lower BMI indication was approved with 1-year data in 2011, with the intention to complete the 5-year evaluation.
Objectives:
To present broad health outcome data including weight change, patient reported outcomes, comorbidity change and complications during the 5-year study.
Setting:
The study was conducted at seven US private practice clinical trial sites.
Methods:
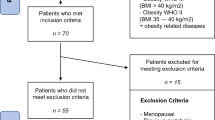
We enrolled 149 BMI 30–39.9 subjects into a 5-year, multicenter, longitudinal, prospective post-approval study. Data for those completing each time point are presented.
Results:
The predefined target of at least 30% excess weight loss was achieved by more than 76% of subjects by 1-year and at every year thereafter during the 5-year study. Mean percentage weight loss at 5 years was 15.9±12.4%. Sustained weight loss was accompanied by sustained improvement in generic and weight-specific quality of life, symptoms of depression and the prevalence of binge-eating disorder. The number of subjects with normal fasting triglyceride, high-density lipoprotein cholesterol, plasma glucose and HbA1c increased significantly between baseline and 5 years. Fifty-four months after LBS implantation, the rate of device explants without replacement was 5.4%; however, the rate of explants increased to 12.1% by month 60 owing to no cost-elective band removals offered to subjects at study exit. No deaths or unanticipated adverse device effects were reported.
Conclusions:
The LBS is safe and effective for people with BMI 30–39.9 with demonstrated improvements in weight loss, comorbidities and quality of life, and with a low explant rate through 5 years following treatment.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Shields M, Carroll MD, Ogden CL . Adult obesity prevalence in Canada and the United States. NCHS Data Brief 2011; 1–8.
CDC. Behavioral Risk Factor Surveillance System (BRFSS) annual data. CDC: Atlanta, GA, USA, 2009.
Dixon JB . The effect of obesity on health outcomes. Mol Cell Endocrinol 2010; 316: 104–108.
NIH. Gastrointestinal Surgery For Severe Obesity. NIH Consens Statement 25–27 March 1991, vol. 2015. NIH, 1991.
Belachew M, Legrand M, Vincenti V, Deffechereux T, Jourdan JL, Monami B et al. Laparoscopic placement of adjustable silicone gastric band in the treatment of morbid obesity: how to do it. Obes Surg 1995; 5: 66–70.
Flum DR, Belle SH, King WC, Wahed AS, Berk P, Chapman W et al. Perioperative safety in the longitudinal assessment of bariatric surgery. N Engl J Med 2009; 361: 445–454.
Demaria EJ, Winegar DA, Pate VW, Hutcher NE, Ponce J, Pories WJ . Early postoperative outcomes of metabolic surgery to treat diabetes from sites participating in the ASMBS bariatric surgery center of excellence program as reported in the Bariatric Outcomes Longitudinal Database. Ann Surg 2010; 252: 559–566; discussion 566–557.
Dixon JB, Straznicky NE, Lambert EA, Schlaich MP, Lambert GW . Surgical approaches to the treatment of obesity. Nat Rev Gastroenterol Hepatol 2011; 8: 429–437.
Padwal RS, Pajewski NM, Allison DB, Sharma AM . Using the Edmonton obesity staging system to predict mortality in a population-representative cohort of people with overweight and obesity. CMAJ 2011; 183: E1059–E1066.
Aasheim ET, Aylwin SJ, Radhakrishnan ST, Sood AS, Jovanovic A, Olbers T et al. Assessment of obesity beyond body mass index to determine benefit of treatment. Clin Obes 2011; 77–84.
Al-Qahtani AR . Laparoscopic adjustable gastric banding in adolescent: safety and efficacy. J Pediatr Surg 2007; 42: 894–897.
Bray GA . Medical treatment of obesity: the past, the present and the future. Best Pract Res Clin Gastroenterol 2014; 28: 665–684.
Miras AD, le Roux CW . Can medical therapy mimic the clinical efficacy or physiological effects of bariatric surgery? Int J Obes 2014; 38: 325–333.
Mitka M . FDA action allows more obese patients to qualify for a bariatric procedure. J Am Med Assoc 2011; 305: 1287–1288.
Michaelson R MD, Gross TM, Whitcup SM, for the LAP-BAND Lower BMI Study Group. LAP-BAND for lower BMI: 2-year results from the multicenter pivotal study. Obesity 2013; 21: 1148–1158.
Dixon JB, McPhail T, O’Brien PE . Minimal reporting requirements for weight loss: current methods not ideal. Obes Surg 2005; 15: 1034–1039.
Arnau RC, Meagher MW, Norris MP, Bramson R . Psychometric evaluation of the Beck Depression Inventory-II with primary care medical patients. Health Psychol 2001; 20: 112–119.
Ware J . SF-36 Health Survey: Manual and Interpretation Guide. The Health Institute, New England Medical Center: Boston, MA, USA, 1997.
Coulman KD, Abdelrahman T, Owen-Smith A, Andrews RC, Welbourn R, Blazeby JM . Patient-reported outcomes in bariatric surgery: a systematic review of standards of reporting. Obes Rev 2013; 14: 707–720.
Kolotkin RL, Crosby RD . Psychometric evaluation of the impact of weight on quality of life-lite questionnaire (IWQOL-lite) in a community sample. Qual Life Res 2002; 11: 157–171.
Stunkard AJ, Messick S . The three-factor eating questionnaire to measure dietary restraint, disinhibition and hunger. J Psychosom Res 1985; 29: 71–83.
Celio AA, Wilfley DE, Crow SJ, Mitchell J, Walsh BT . A comparison of the binge eating scale, questionnaire for eating and weight patterns-revised, and eating disorder examination questionnaire with instructions with the eating disorder examination in the assessment of binge eating disorder and its symptoms. Int J Eat Disord 2004; 36: 434–444.
Favretti F, O’Brien PE, Dixon JB . Patient management after LAP-BAND placement. Am J Surg 2002; 184: S38–S41.
Ware J . SF-36 Physical and Mental Health Summary Scales: A User's Manual. The Health Institute, New England Medical Center: Boston, MA, USA 1994.
Sjostrom L . Review of the key results from the Swedish Obese Subjects (SOS) trial: a prospective controlled intervention study of bariatric surgery. J Int Med 2012; 273: 219–234.
O’Brien PE, McPhail T, Chaston TB, Dixon JB . Systematic review of medium-term weight loss after bariatric operations. Obes Surg 2006; 16: 1032–1040.
Guyenet SJ, Schwartz MW . Clinical review: regulation of food intake, energy balance, and body fat mass: implications for the pathogenesis and treatment of obesity. J Clin Endocrinol Metab 2012; 97: 745–755.
Levin BE, Keesey RE . Defense of differing body weight set points in diet-induced obese and resistant rats. Am J Physiol 1998; 274: R412–R419.
Colles SL, Dixon JB, O’Brien PE . Hunger control and regular physical activity facilitate weight loss after laparoscopic adjustable gastric banding. Obes Surg 2008; 18: 833–840.
Colles SL, Dixon JB, O’Brien PE . Loss of control is central to psychological disturbance associated with binge eating disorder. Obesity (Silver Spring) 2008; 16: 608–614.
Dixon AF, Dixon JB, O’Brien PE . Laparoscopic adjustable gastric banding induces prolonged satiety: a randomized blind crossover study. J Clin Endocrinol Metab 2005; 90: 813–819.
Bruce AS, Bruce JM, Ness AR, Lepping RJ, Malley S, Hancock L et al. A comparison of functional brain changes associated with surgical versus behavioral weight loss. Obesity (Silver Spring) 2014; 22: 337–343.
Arnstein NB, Shapiro B, Ekhauser FE, Dmuchowski CF, Knol JA, Strodel WE et al. Morbid obesity treated by gastroplasty: radionuclide gastric emptying studies. Radiology 1985; 156: 501–504.
Burton PR, Brown WA . The mechanism of weight loss with laparoscopic adjustable gastric banding: induction of satiety not restriction. Int J Obes 2011; 35: S26–S30.
Melissas J, Koukouraki S, Askoxylakis J, Stathaki M, Daskalakis M, Perisinakis K et al. Sleeve gastrectomy: a restrictive procedure? Obes Surg 2007; 17: 57–62.
Dixon JB, Dixon ME, O’Brien PE . Quality of life after lap-band placement: influence of time, weight loss, and comorbidities. Obes Res 2001; 9: 713–721.
Kolotkin RL, Crosby RD, Gress RE, Hunt SC, Adams TD . Two-year changes in health-related quality of life in gastric bypass patients compared with severely obese controls. Surg Obes Relat Dis 2009; 5: 250–256.
O’Brien PE, Dixon JB, Laurie C, Skinner S, Proietto J, McNeil J et al. Treatment of mild to moderate obesity with laparoscopic adjustable gastric banding or an intensive medical program: a randomized trial. Ann Int Med 2006; 144: 625–633.
Dixon JB, Dixon ME, O’Brien PE . Depression in association with severe obesity: changes with weight loss. Arch Intern Med 2003; 163: 2058–2065.
Waters GS, Pories WJ, Swanson MS, Meelheim HD, Flickinger EG, May HJ . Long-term studies of mental health after the Greenville gastric bypass operation for morbid obesity. Am J Surg 1991; 161: 154–157 discussion 157–158.
Adams TD, Gress RE, Smith SC, Halverson RC, Simper SC, Rosamond WD et al. Long-term mortality after gastric bypass surgery. N Engl J Med 2007; 357: 753–761.
King WC, Chen JY, Mitchell JE, Kalarchian MA, Steffen KJ, Engel SG et al. Prevalence of alcohol use disorders before and after bariatric surgery. JAMA 2012; 307: 2516–2525.
Dixon JB, Straznicky NE, Lambert EA, Schlaich MP, Lambert GW . Laparoscopic adjustable gastric banding and other devices for the management of obesity. Circulation 2012; 126: 774–785.
Sjostrom L, Lindroos AK, Peltonen M, Torgerson J, Bouchard C, Carlsson B et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med 2004; 351: 2683–2693.
Straznicky N, Grassi G, Esler M, Lambert G, Dixon J, Lambert E et al. European Society of Hypertension Working Group on Obesity Antihypertensive effects of weight loss: myth or reality? J Hypertens 2010; 28: 637–643.
Schauer PR, Bhatt DL, Kirwan JP, Wolski K, Brethauer SA, Navaneethan SD et al. Bariatric surgery versus intensive medical therapy for diabetes—3-year outcomes. N Engl J Med 2014; 370: 2002–2013.
O'Brien PE, Macdonald L, Anderson M, Brennan L, Brown WA . Long-term outcomes after bariatric surgery: fifteen-year follow-up of adjustable gastric banding and a systematic review of the bariatric surgical literature. Ann Surg 2013; 257: 87–94.
Ren CJ, Fielding GA . Laparoscopic adjustable gastric banding: surgical technique. J Laparoendosc Adv Surg Tech A 2003; 13: 257–263.
DeMaria EJ, Sugerman HJ, Meador JG, Doty JM, Kellum JM, Wolfe L et al. High failure rate after laparoscopic adjustable silicone gastric banding for treatment of morbid obesity. Ann Surg 2001; 233: 809–818.
Ponce J, Paynter S, Fromm R . Laparoscopic adjustable gastric banding: 1,014 consecutive cases. J Am Coll Surg 2005; 201: 529–535.
Westling A, Bjurling K, Ohrvall M, Gustavsson S . Silicone-adjustable gastric banding: disappointing results. Obes Surg 1998; 8: 467–474.
Acknowledgements
The LAP-BAND Lower BMI Study Group Investigators included Thomas Chua, MD (Wisconsin), Kevin Montgomery, MD (Washington), Terry Simpson, MD (Arizona), Timothy Ehrlich, MD (Connecticut), George Woodman, MD (Tennessee), Brad Watkins, MD (Ohio), and Hans Joseph Schmidt (New Jersey).
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
Allergan Medical (Goleta, CA, USA) designed and funded the study before it was transferred to Apollo Endosurgery (Austin, TX, USA). LLE, VV and JBD are consultants for Apollo Endosurgery. LLE and JBD were also consultants for Allergan Medical while the study was being conducted. VV was an employee of Allergan, Inc. and a shareholder while the study was being conducted. RM was an investigator in the study and a consultant to Allergan Medical (Goleta, CA, USA).
Rights and permissions
About this article
Cite this article
Dixon, J., Eaton, L., Vincent, V. et al. LAP-BAND for BMI 30–40: 5-year health outcomes from the multicenter pivotal study. Int J Obes 40, 291–298 (2016). https://doi.org/10.1038/ijo.2015.156
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2015.156
This article is cited by
-
Weight Loss and Health Status 5 Years After Adjustable Gastric Banding in Adolescents
Obesity Surgery (2020)
-
Pre-operative Restraint and Post-operative Hunger, Disinhibition and Emotional Eating Predict Weight Loss at 2 Years Post-laparoscopic Adjustable Gastric Banding
Obesity Surgery (2020)
-
Medical devices for the treatment of obesity
Nature Reviews Gastroenterology & Hepatology (2017)
-
The Physiology and Pathophysiology of Gastroesophageal Reflux in Patients with Laparoscopic Adjustable Gastric Band
Obesity Surgery (2017)
-
Food for Thought: Reward Mechanisms and Hedonic Overeating in Obesity
Current Obesity Reports (2017)