Abstract
Background/Objectives:
Weight gain after quitting smoking is a common concern for smokers and can discourage quit attempts. The purpose of this analysis was to describe the long-term weight gain, smoking cessation attributable (SCA) weight gain and describe their relationship to cigarette consumption and body mass index (BMI) 10 years ago in a contemporary, nationally representative sample of smokers who continued to smoke and those who quit.
Subjects/Methods:
In all, 12 204 adults ⩾36 years old were selected from the 2003–2012 National Health and Nutrition Examination Survey (NHANES). Ten-year weight gain for never, continuing and former smokers (who quit 1–10 years ago) was calculated by body mass index (BMI) 10 years ago and cigarettes per day (CPD). SCA weight gain was calculated by taking the difference between the adjusted mean 10-year weight gain of former smokers and that of continuing smokers.
Results:
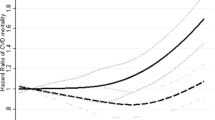
Mean 10-year weight gain among continuing smokers was 3.5 versus 8.4 kg among former smokers; the SCA weight gain was 4.9 kg. After Bonferroni correction, there was no significant difference in overall weight gain between continuing and former smokers of 1–14 CPD, and SCA weight gain was lowest in this group (2.0 kg, confidence interval (CI): 0.3, 3.7). SCA weight gain was highest for former smokers of ⩾25 CPD (10.3 kg, CI: 7.4, 13.2) and for those who were obese (7.1 kg, CI: 2.9, 11.3) mostly because of lower than average weight gain or weight loss among continuing smokers in these groups.
Conclusions:
In a current, nationally representative sample, baseline BMI and CPD were important factors that contributed to the magnitude of long-term weight gain following smoking cessation. Light to moderate smokers (<15 CPD) experienced little SCA weight gain, whereas heavy smokers (⩾25 CPD) and those who were obese before quitting experienced the most.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others

References
US Burden of Disease Collaborators. The State of US Health, 1990–2010: burden of diseases, injuries, and risk factors. JAMA 2013; 310: 591–608.
US Department of Health Human Services. The Health Benefits of Smoking Cessation. Public Health Service, Centers for Disease Control Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health: Washington, DC, 1990.
Aubin HJ, Farley A, Lycett D, Lahmek P, Aveyard P . Weight gain in smokers after quitting cigarettes: Meta-analysis. BMJ 2012; 345: e4439.
Albanes D, Jones DY, Micozzi MS, Mattson ME . Associations between smoking and body weight in the US population: analysis of NHANES II. Am J Public Health 1987; 77: 439–444.
Flegal KM, Troiano RP, Pamuk ER, Kuczmarski RJ, Campbell SM . The influence of smoking cessation on the prevalence of overweight in the United States. N Engl J Med 1995; 333: 1165–1170.
O'Hara P, Connett JE, Lee WW, Nides M, Murray R, Wise R . Early and late weight gain following smoking cessation in the Lung Health Study. Am J Epidemiol 1998; 148: 821–830.
Janzon E, Hedblad B, Berglund G, Engstrom G . Changes in blood pressure and body weight following smoking cessation in women. J Intern Med 2004; 255: 266–272.
Williamson DF, Madans J, Anda RF, Kleinman JC, Giovino GA, Byers T . Smoking cessation and severity of weight gain in a national cohort. N Engl J Med 1991; 324: 739–745.
Lycett D, Munafo M, Johnstone E, Murphy M, Aveyard P . Associations between weight change over 8 years and baseline body mass index in a cohort of continuing and quitting smokers. Addiction 2011; 106: 188–196.
Aubin HJ, Berlin I, Smadja E, West R . Factors associated with higher body mass index, weight concern, and weight gain in a multinational cohort study of smokers intending to quit. Int J Environ Res Public Health 2009; 6: 943–957.
Pomerleau CS, Zucker AN, Stewart AJ . Characterizing concerns about post-cessation weight gain: results from a national survey of women smokers. Nicotine Tob Res 2001; 3: 51–60.
Clearman DR, Jacobs DR Jr . Relationships between weight and caloric intake of men who stop smoking: the Multiple Risk Factor Intervention Trial. Addict Behav 1991; 16: 401–410.
Swan GE, Carmelli D . Characteristics associated with excessive weight gain after smoking cessation in men. Am J Public Health 1995; 85: 73–77.
Flegal KM . The effects of changes in smoking prevalence on obesity prevalence in the United States. Am J Public Health 2007; 97: 1510–1514.
Mackay DF, Gray L, Pell JP . Impact of smoking and smoking cessation on overweight and obesity: Scotland-wide, cross-sectional study on 40,036 participants. BMC Public Health 2013; 13: 348.
Zipf G, Chiappa M, Porter KS, Ostchega Y, Lewis BG, Dostal J . National Health and Nutrition Examination Survey: plan and operations, 1999–2010. Vital Health Stat 2013; 1: 1–28.
National Heart Lung and Blood Institute. Clinical Guidelines on the Identification, Evaluation and Treatment of Overweight and Obesity in Adults. National Institutes of Health: Bethesda, MD, USA,1998.
Johnson CL, Paulose-Ram R, Ogden CL, Carroll MA, Kruszon-Moran D, Dohrmann SM et al. National Health and Nutrition Examination Survey: analytic guidelines 1999–2010. Vital Health Stat 2013; 2: 1–16.
Perry GS, Byers TE, Mokdad AH, Serdula MK, Williamson DF . The validity of self-reports of past body weights by US adults. Epidemiology 1995; 6: 61–66.
Prospective Studies Collaboration, Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson J et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet 2009; 373: 1083–1096.
Fiore MC . Treating Tobacco Use and Dependence: 2008 Update. Clinical Practice Guideline. US Department of health and Human Services. Public Health Service: Rockville, MD, USA, 2008.
Le Strat Y, Rehm J, Le Foll B . How generalisable to community samples are clinical trial results for treatment of nicotine dependence: a comparison of common eligibility criteria with respondents of a large representative general population survey. Tob Control 2011; 20: 338–343.
Flegal KM, Carroll MD, Kit BK, Ogden CL . Prevalence of obesity and trends in the distribution of body mass index among U.S. adults, 1999–2010. JAMA 2012; 307: 491–497.
Fryar C, Carroll M, Ogden C . Prevalence of overweight, obesity, and extreme obesity among adults: United States, trends 1960–1962 through 2011–2012. NCHS Health E-Stat 2014. Available at http://www.cdc.gov/nchs/data/hestat/obesity_adult_11_12/obesity_adult_11_12.htm.
US Department of Health and Human Services. The Health Consequences of Smoking—50 Years of Progress, A Report of the Surgeon General. US Department of Health and Human Services: Atlanta, GA, USA, 2014.
Pomerleau CS, Ehrlich E, Tate JC, Marks JL, Flessland KA, Pomerleau OF . The female weight-control smoker: a profile. J Subst Abuse 1993; 5: 391–400.
Klesges RC, Somes G, Pascale RW, Klesges LM, Murphy M, Brown K et al. Knowledge and beliefs regarding the consequences of cigarette smoking and their relationships to smoking status in a biracial sample. Health Psychol 1988; 7: 387–401.
Audrain-McGovern J, Benowitz NL . Cigarette smoking, nicotine, and body weight. Clin Pharmacol Ther 2011; 90: 164–168.
Fernandez E, Chapman S . Quitting smoking and gaining weight: The odd couple. BMJ 2012; 345: e4544.
Veldheer S, Yingst J, Foulds G, Hrabovsky S, Berg A, Sciamanna C et al. Once bitten, twice shy: concern about gaining weight after smoking cessation and its association with seeking treatment. Int J Clin Pract 2014; 68: 388–395.
Levine MD, Bush T, Magnusson B, Cheng Y, Chen X . Smoking-related weight concerns and obesity: Differences among normal weight, overweight, and obese smokers using a telephone tobacco quitline. Nicotine Tob Res 2013; 15: 1136–1140.
Clair C, Rigotti NA, Porneala B, Fox CS, D'Agostino RB, Pencina MJ et al. Association of smoking cessation and weight change with cardiovascular disease among adults with and without diabetes. JAMA 2013; 309: 1014–1021.
Freedman DM, Sigurdson AJ, Rajaraman P, Doody MM, Linet MS, Ron E . The mortality risk of smoking and obesity combined. Am J Prev Med 2006; 31: 355–362.
Farley AC, Hajek P, Lycett D, Aveyard P . Interventions for preventing weight gain after smoking cessation. Cochrane Database Syst Rev 2012; 1: CD006219.
West R, Zatonski W, Przewozniak K, Jarvis MJ . Can we trust national smoking prevalence figures? Discrepancies between biochemically assessed and self-reported smoking rates in three countries. Cancer Epidemiol Biomarkers Prev 2007; 16: 820–822.
Caraballo RS, Giovino GA, Pechacek TF, Mowery PD . Factors associated with discrepancies between self-reports on cigarette smoking and measured serum cotinine levels among persons aged 17 years or older: Third National Health and Nutrition Examination Survey, 1988–1994. Am J Epidemiol 2001; 153: 807–814.
Bland JM, Altman DG . Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986; 1: 307–310.
Acknowledgements
This research was supported by funds from the Penn State Cancer Institute to JF.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
JF has done paid consulting for pharmaceutical companies involved in producing smoking cessation medications including GSK, Pfizer, Novartis, J&J and Cypress Bioscience. The other authors have no conflict of interest to declare.
Additional information
Supplementary Information accompanies this paper on International Journal of Obesity website
Supplementary information
Rights and permissions
About this article
Cite this article
Veldheer, S., Yingst, J., Zhu, J. et al. Ten-year weight gain in smokers who quit, smokers who continued smoking and never smokers in the United States, NHANES 2003–2012. Int J Obes 39, 1727–1732 (2015). https://doi.org/10.1038/ijo.2015.127
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2015.127
This article is cited by
-
Association between weight gain following smoking cessation and development of hypertension in the future
Hypertension Research (2024)
-
Development and Evaluation of a Health Behavior Change Clinic in Primary Care: An Interdisciplinary Partnership
Journal of Clinical Psychology in Medical Settings (2023)
-
Brain-derived neurotrophic factor gene variants and obesity in former smokers
BMC Genomics (2021)
-
Cardiometabolic Morbidity and Mortality with Smoking Cessation, Review of Recommendations for People with Diabetes and Obesity
Current Diabetes Reports (2020)
-
Tobacco Smoking, Eating Behaviors, and Body Weight: a Review
Current Addiction Reports (2019)