Abstract
Background:
Weight status in children and adolescents is commonly defined using age- and gender-corrected standard deviation scores for body mass index (BMI-SDS, also called z-scores). Values are not reliable for the extremely obese however. Moreover, paediatricians and parents may have difficulties understanding z-scores, and while percentiles are easier to gauge, the very obese have values above the 99th percentile, making distinction difficult. The notion of excess body weight (EBW) is increasingly applied in adult patients, mainly in the context of bariatric surgery. However, a clear definition is not available to date for the paediatric population.
Methods:
A simple definition of EBW for children and adolescents is introduced, with median weight as a function of height, age and gender (characterized by an asterisk): EBW (%)=100x(weight−median weight*)/median weight*. EBW is compared with BMI-SDS and waist-to-height ratio (WHtR). Using two data sources (APV registry and German Health Interview and Examination Survey for Children and Adolescents (KiGGS)) including more than 14 000 children, the relationships between these anthropometric and various metabolic parameters are analysed for a group of overweight/obese children who have sought obesity therapy (APV), for the general paediatric population and for the subset of overweight/obese children from the general population (KiGGS).
Results:
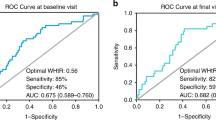
The three anthropometric parameters are strongly correlated, with the linear correlation coefficients exceeding 0.8 in the general population and 0.75 in those seeking obesity therapy. Moreover, their relationship to metabolic parameters is quite similar regarding correlations and area under the curve from receiver operating characteristic analyses.
Conclusions:
EBW has similar predictive value for metabolic or cardiovascular comorbidities compared with BMI and WHtR. As it is reliable at the extreme end of the obesity spectrum, easily communicable and simple to use in daily practice, it would make a very useful addition to existing tools for working with obese children and adolescents. Its usefulness in assessing weight change needs to be studied however.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Javed A, Jumean M, Murad MH, Okorodudu D, Kumar S, Somers VK et al. Diagnostic performance of body mass index to identify obesity as defined by body adiposity in children and adolescents: a systematic review and meta-analysis. Pediatr Obes 2014 (e-pub ahead of print 25 June 2014).
Cole TJ, Faith MS, Pietrobelli A, Heo M . What is the best measure of adiposity change in growing children: BMI, BMI %, BMI z-score or BMI centile? Eur J Clin Nutr 2005; 59: 419–425.
Browning LM, Hsieh SD, Ashwell M . A systematic review of waist-to-height ratio as a screening tool for the prediction of cardiovascular disease and diabetes: 0.5 could be a suitable global boundary value. Nutr Res Rev 2010; 23: 247–269.
Savva SC, Lamnisos D, Kafatos AG . Predicting cardiometabolic risk: waist-to-height ratio or BMI. A meta-analysis. Diabetes Metab Syndr Obes 2013; 6: 403–419.
Savva SC, Tornaritis M, Savva ME, Kourides Y, Panagi A, Silikiotou N et al. Waist circumference and waist-to-height ratio are better predictors of cardiovascular disease risk factors in children than body mass index. Int J Obes Relat Metab Disord 2000; 24: 1453–1458.
Hara M, Saitou E, Iwata F, Okada T, Harada K . Waist-to-height ratio is the best predictor of cardiovascular disease risk factors in Japanese school children. J Artheroscler Thromb 2002; 9: 127–132.
Owens S, Litaker M, Allison J, Riggs S, Ferguson M, Gutin B . Prediction of visceral adipose tissue from simple anthropometric measurements in youths with obesity. Obes Res 1999; 7: 16–22.
Lee KK, Park HS, Yum KS . Cut-off values of visceral fat area and waist-to-height ratio: diagnostic criteria for obesity-related disorders in Korean children and adolescents. Yonsei Med J 2012; 53: 99–105.
Hunt LP, Ford A, Sabin MA, Crowne EC, Shield JPH . Clinical measures of adiposity and percentage fat loss: which measure most accurately reflects fat loss and what should we aim for? Arch Dis Child 2007; 92: 399–403.
Toschke AM, Reinehr T . Different anthropometric index changes in relation to cardiovascular risk profile change. Clin Nutr 2008; 27: 457–463.
Kromeyer-Hauschild K, Wabitsch M, Kunze D, Geller F, Geiß HC, Hesse V et al. Percentiles of body mass index in children and adolescents evaluated from different regional German studies. Monatsschr Kinderheilkd 2001; 149: 807–818.
Centers for Disease Control and Prevention. CDC Growth Charts. National Center for Health Statistics: United States; http://www.cdc.gov/growthcharts/html_charts/bmiagerev.htm (last accessed 25 2August 2014).
Sakamoto N, Yang L . BMI centile curves for Japanese children aged 5-17 years in 2000-2005. Public Health Nutr 2009; 12: 1688–1692.
Khadilkar V, Khadilkar A . Growth charts: a diagnostic tool. Indian J Endocrinol Metab 2011; 15 (Suppl 3): S166–S171.
Zimmet P, Alberti KG, Kaufman F, Tajima N, Silink M, Arslanian S et al. The metabolic syndrome in children and adolescents—an IDF consensus report. Pediatr Diabetes 2007; 8: 299–306.
Kurtoglu S, Akin L, Kendirci M, Hatipoglu N, Elmali F, Mazicioglu M . The absence of insulin resistance in metabolic syndrome definition leads to underdiagnosing of metabolic risk in obese patients. Eur J Pediatr 2012; 171: 1331–1337.
Neuhauser H, Schienkiewitz A, Rosario A, Dortschy R, Kurth BM . Referenzperzentile für anthropometrische Maßzahlen und Blutdruck aus der Studie zur Gesundheit von Kindern und Jugendlichen in Deutschland (KiGGS). RKI-Hausdruckerei: Berlin, 2013.
Keskin M, Kurtoglu S, Kendirci M, Atabek ME, Yazici C . Homeostasis model assessment is more reliable than the fasting glucose/insulin ratio and quantitative insulin sensitivity check index for assessing insulin resistance among obese children and adolescents. Pediatrics 2005; 115: e500–e503.
Reinehr T, Wabitsch M, Andler W, Beyer P, Böttner A, Chen-Stute A et al. Medical care of obese children and adolescents. APV: a standardised multicentre documentation derived to study initial presentation and cardiovascular risk factors in patients transferred to specialised treatment institutions. Eur J Pediatr 2004; 163: 308–312.
Kurth BM, Kamtsiuris P, Hölling H, Schlaud M, Dölle R, Ellert U et al. The challenge of comprehensively mapping children's health in a nation-wide health survey: design of the German KiGGS-Study. BMC Public Health 2008; 8: 196.
Public Use File KiGGS. The German Health Survey for Children and Adolescents 2003–2006. Robert Koch Institute: Berlin, Germany, 2008.
DeLong ER, DeLong DM, Clarke-Pearson DL . Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 1988; 44: 837–845.
R Core Team. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing: Vienna, Austria http://www.R-project.org/ 2013.
Robin X, Turck N, Hainard A, Tiberti N, Lisacek F, Sanchez JC et al. pROC: an open-source package for R and S+ to analyze and compare ROC curves. BMC Bioinform 2011; 12: 77.
Weiss R, Dziura J, Burgert TS, Tamborlane WV, Taksali SE, Yeckel CW et al. Obesity and the metabolic syndrome in children and adolescents. N Engl J Med 2004; 350: 2362–2374.
Wells JC, Cole TJ . Height, adiposity and hormonal cardiovascular risk markers in childhood: how to partition the associations? Int J Obes 2014; 38: 930–935.
Acknowledgements
We express our gratitude to all health professionals of the APV Study Group taking care of overweight and obese children and contributing to the APV database. Part of the work was supported by the Federal Ministry of Education and Research, Germany (Integrated Research and Treatment Center IFB ‘Adiposity Diseases’, FKZ: 01E01001; Competence Network Obesity, FKZ 01GI1130).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Petroff, D., Kromeyer-Hauschild, K., Wiegand, S. et al. Introducing excess body weight in childhood and adolescence and comparison with body mass index and waist-to-height ratio. Int J Obes 39, 52–60 (2015). https://doi.org/10.1038/ijo.2014.170
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2014.170
This article is cited by
-
Effects of a novel mobile health intervention compared to a multi-component behaviour changing program on body mass index, physical capacities and stress parameters in adolescents with obesity: a randomized controlled trial
BMC Pediatrics (2021)
-
Association between junk food consumption and cardiometabolic risk factors in a national sample of Iranian children and adolescents population: the CASPIAN-V study
Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity (2020)
-
Resistin and visfatin concentrations are related to central obesity and inflammation in Brazilian children
Nutrire (2018)
-
Längsschnittstudie des aktuellen Wachstums 0‑ bis 6‑jähriger deutscher Kinder: Teil 3
Monatsschrift Kinderheilkunde (2017)