Abstract
Objective:
To examine the acute effects of high-intensity intermittent exercise (HIIE) on energy intake, perceptions of appetite and appetite-related hormones in sedentary, overweight men.
Design:
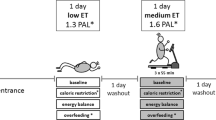
Seventeen overweight men (body mass index: 27.7±1.6 kg m−2; body mass: 89.8±10.1 kg; body fat: 30.0±4.3%; VO2peak: 39.2±4.8 ml kg−1 min−1) completed four 30-min experimental conditions using a randomised counterbalanced design. CON: resting control, MC: continuous moderate-intensity exercise (60% VO2peak), HI: high-intensity intermittent exercise (alternating 60 s at 100% VO2peak and 240 s at 50% VO2peak), VHI: very-high-intensity intermittent exercise (alternating 15 s at 170% VO2peak and 60 s at 32% VO2peak). Participants consumed a standard caloric meal following exercise/CON and an ad-libitum meal 70 min later. Capillary blood was sampled and perceived appetite assessed at regular time intervals throughout the session. Free-living energy intake and physical activity levels for the experimental day and the day after were also assessed.
Results:
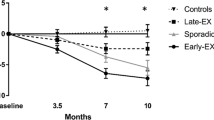
Ad-libitum energy intake was lower after HI and VHI compared with CON (P=0.038 and P=0.004, respectively), and VHI was also lower than MC (P=0.028). Free-living energy intake in the subsequent 38 h remained less after VHI compared with CON and MC (P⩽0.050). These observations were associated with lower active ghrelin (P⩽0.050), higher blood lactate (P⩽0.014) and higher blood glucose (P⩽0.020) after VHI compared with all other trials. Despite higher heart rate and ratings of perceived exertion (RPE) during HI and VHI compared with MC (P⩽0.004), ratings of physical activity enjoyment were similar between all the exercise trials (P=0.593). No differences were found in perceived appetite between trials.
Conclusions:
High-intensity intermittent exercise suppresses subsequent ad-libitum energy intake in overweight inactive men. This format of exercise was found to be well tolerated in an overweight population.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Ross R, Freeman JA, Janssen I . Exercise alone is an effective strategy for reducing obesity and related comorbidities. Exerc Sport Sci Rev 2000; 28: 165–170.
Catenacci VA, Wyatt HR . The role of physical activity in producing and maintaining weight loss. Nat Clin Pract Endocrinol Metab 2007; 3: 518–529.
Okay D . Exercise and obesity. Prim Care 2009; 36: 379–393.
Guelfi KJ, Donges CE, Duffield R . Beneficial effects of 12 weeks of aerobic compared with resistance exercise training on perceived appetite in previously sedentary overweight and obese men. Metabolism 2013; 62: 235–243.
Balaguera-Cortes L, Wallman KE, Fairchild TJ, Guelfi KJ . Energy intake and appetite-related hormones following acute aerobic and resistance exercise. Appl Physiol Nutr Metab 2011; 36: 958–966.
Crisp NA, Fournier PA, Licari MK, Braham R, Guelfi KJ . Optimising sprint interval exercise to maximise energy expenditure and enjoyment in overweight boys. Appl Physiol Nutr Metab 2012; 37: 1222–1231.
Thivel D, Isacco L, Montaurier C, Boirie Y, Duche P, Morio B . The 24-h energy intake of obese adolescents is spontaneously reduced after intensive exercise: a randomized controlled trial in calorimetric chambers. PLoS One 2012; 7: e29840.
Erdmann J, Tahbaz R, Lippl F, Wagenpfeil S, Schusdziarra V . Plasma ghrelin levels during exercise—effects of intensity and duration. Regul Pept 2007; 143: 127–135.
Ueda S, Yoshikawa T, Katsura Y, Usui T, Nakao H, Fujimoto S . Changes in gut hormone levels and negative energy balance during aerobic exercise in obese young males. J Endocrinol 2009; 201: 151–159.
Kessler HS, Sisson SB, Short KR . The potential for high-intensity interval training to reduce cardiometabolic disease risk. Sports Med 2012; 42: 489–509.
National Physical Activity Guidelines for Australia. Commonwealth Department of Health and Ageing 2005.
Van Strien T, Frijters JER, Bergers G, Defares PB . The Dutch Eating Behavior Questionnaire (DEBQ) for assessment of restrained, emotional, and external eating behavior. Int J Eat Disord 1986; 5: 295–315.
West JS, Ayton T, Wallman KE, Guelfi KJ . The effect of 6 days of sodium phosphate supplementation on appetite, energy intake, and aerobic capacity in trained men and women. Int J Sport Nutr Exerc Metab 2012; 22: 422–429.
Peryam DR, Pilgrim FJ . Hedonic scale method of measuring food preferences. Food Technol 1957; 11: 9–14.
Borg G . Psychophysical bases of perceived exertion. Med Sci Sports Exerc 1982; 14: 377–381.
Kendzierski D, DeCarlo KJ . Physical activity enjoyment scale: two validation studies. J Sport Exerc Psychol 1991; 13: 50–64.
Wansink B . Environmental factors that increase the food intake and consumption of unknowing consumers. Annu Rev Nutr 2004; 24: 455–479.
Hill AJ, Blundell JE . Nutrients and behaviour: research strategies for the investigation of taste characteristics, food preferences, hunger sensations and eating patterns in man. J Psychiatr Res 1982; 17: 203–212.
Deighton K, Barry R, Connon CE, Stensel DJ . Appetite, gut hormone and energy intake responses to low volume sprint interval and traditional endurance exercise. Eur J Appl Physiol 2013; 113: 1147–1156.
Mattes R . Hunger ratings are not a valid proxy measure of reported food intake in humans. Appetite 1990; 15: 103–113.
Wynne K, Stanley S, McGowan B, Bloom S . Appetite control. J Endocrinol 2005; 184: 291–318.
Broom DR, Stensel DJ, Bishop NC, Burns SF, Miyashita M . Exercise-induced suppression of acylated ghrelin in humans. J Appl Physiol 2007; 102: 2165–2171.
Clausen J . Effect of physical training on cardiovascular adjustments to exercise in man. Physiol Rev 1977; 57: 779–815.
Borghouts L, Borghouts B . Exercise and insulin sensitivity: A Review. Int J Sports Med 2000; 21: 1–12.
Dyck DJ . Leptin sensitivity in skeletal muscle is modulated by diet and exercise. Exerc Sport Sci Rev 2005; 33: 189–194.
Martins C, Morgan LM, Bloom SR, Robertson MD . Effects of exercise on gut peptides, energy intake and appetite. J Endocrinol 2007; 193: 251–258.
Broom DR, Batterham RL, King JA, Stensel DJ . Influence of resistance and aerobic exercise on hunger, circulating levels of acylated ghrelin, and peptide YY in healthy males. Am J Physiol Regul Integr Comp Physiol 2009; 296: R29–R34.
Lam CK, Chari M, Wang PY, Lam TK . Central lactate metabolism regulates food intake. Am J Physiol Endocrinol Metab 2008; 295: E491–E496.
Nagase H, Bray GA, York DA . Effects of pyruvate and lactate on food intake in rat strains sensitive and resistant to dietary obesity. Physiol Behav 1996; 59: 555–560.
Friedman MI . Control of energy intake by energy metabolism. Am J Clin Nutr 1995; 62: 1096S–1100S.
Scheurink AJ, Ammar AA, Benthem B, van Dijk G, Sodersten PA . Exercise and the regulation of energy intake. Int J Obes Relat Metab Disord 1999; 23 (Suppl 3): S1–S6.
Ryan RM, Frederick CM, Lepes D, Rubio N, Sheldon KM . Intrinsic motivation and exercise adherence. Int J Sport Exerc Psychol 1997; 28: 335–354.
Hagberg L, Lindahl B, Nyberg L, Hellénius ML . Importance of enjoyment when promoting physical exercise. Scand J Med Sci Sports 2009; 19: 740–747.
Bartlett JD, Close GL, MacLaren DP, Gregson W, Drust B, Morton JP . High-intensity interval running is perceived to be more enjoyable than moderate-intensity continuous exercise: implications for exercise adherence. J Sports Sci 2011; 29: 547–553.
Acknowledgements
The hormone assays were carried out with the facilities at the Centre for Microscopy, Characterisation and Analysis, The University of Western Australia that are supported by the fundings of the University, State and Federal Government. TJF is in receipt of a McCusker Charitable Foundation grant, which was used to help defray costs of the Hormone assays.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Sim, A., Wallman, K., Fairchild, T. et al. High-intensity intermittent exercise attenuates ad-libitum energy intake. Int J Obes 38, 417–422 (2014). https://doi.org/10.1038/ijo.2013.102
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2013.102
Keywords
This article is cited by
-
A Comparison of Acute High- and Moderate-Intensity Exercise on Cardio- Metabolic Function and Sleep Among Shift Workers
Journal of Science in Sport and Exercise (2024)
-
Exercise-induced responses in matrix metalloproteinases and osteopontin are not moderated by exercise format in males with overweight or obesity
European Journal of Applied Physiology (2023)
-
Post-exercise energy intake: do the intensity and mode of exercise matter? A systematic review and meta-analysis comparing high-intensity interval with moderate-intensity continuous protocols
European Journal of Clinical Nutrition (2022)
-
Effect of physical exercise in bariatric surgery patients: protocol of a randomized controlled clinical trial
Trials (2021)
-
Effects of a high-intensity interval training session and chocolate milk on appetite and cognitive performance in youth aged 9–13 years
European Journal of Clinical Nutrition (2021)