Abstract
Background and Objective:
The United States has experienced a large increase in the prevalence of obesity since the 1970s. Our objective was to describe recent trends in obesity and abdominal obesity among adults in the United States.
Design:
Trend study of cross-sectional studies.
Subjects:
We used data from up to 22 872 men and non-pregnant women aged ⩾20 years from the National Health and Nutrition Examination Survey (NHANES) 1999–2008.
Main Outcome Measures:
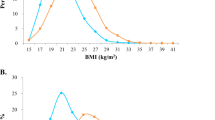
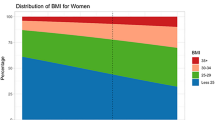
Main outcome measures are mean body mass index and waist circumference, percentages of obesity and abdominal obesity. Obesity was defined as a body mass index ⩾30 kg m−2, and abdominal obesity was defined as a waist circumference ⩾102 cm in men and ⩾88 cm in women.
Results:
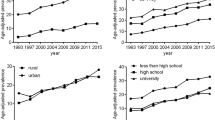
In men, the age-adjusted mean body mass index, mean waist circumference, and prevalence of obesity and abdominal obesity were 27.8 kg m−2, 99.1 cm, and 26.9 and 37.8%, respectively, during 1999–2000 and 28.5 kg m−2 (Ptrend=0.001), 100.8 cm (Ptrend=0.002), and 32.0 (Ptrend=0.001) and 43.7% (Ptrend=0.002), respectively, during 2007–2008. In women, the age-adjusted mean body mass index, mean waist circumference, and prevalence of obesity and abdominal obesity were 28.2 kg m−2, 92.2 cm, and 33.2 and 55.8%, respectively, during 1999–2000 and 28.6 kg m−2 (Ptrend=0.181), 94.9 cm (Ptrend=0.006), and 35.2 (Ptrend=0.180) and 61.8% (Ptrend=0.036), respectively, during 2007–2008. Significant linear trends for increasing prevalence of obesity were noted among men with the least and most education.
Conclusion:
Between 1999 and 2008, both obesity and abdominal obesity increased in men, and abdominal obesity increased in women.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Flegal KM, Carroll MD, Ogden CL, Johnson CL . Prevalence and trends in obesity among US adults, 1999–2000. JAMA 2002; 288: 1723–1727.
Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM . Prevalence of overweight and obesity in the United States, 1999–2004. JAMA 2006; 295: 1549–1555.
Guh DP, Zhang W, Bansback N, Amarsi Z, Birmingham CL, Anis AH . The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC Public Health 2009; 9: 88.
Olshansky SJ, Passaro DJ, Hershow RC, Layden J, Carnes BA, Brody J et al. A potential decline in life expectancy in the United States in the 21st century. N Engl J Med 2005; 352: 1138–1145.
Finkelstein EA, Trogdon JG, Cohen JW, Dietz W . Annual medical spending attributable to obesity: payer- and service-specific estimates. Health Aff (Millwood) 2009; 28: w822–w831.
US Department of Health and Human Services. Healthy People 2010 Leading Health Indicators Accessed at: http://www.healthypeople.gov/Document/HTML/uih/uih_4.htm on 2 April 2010.
US Department of Health and Human Services and Office of Disease Prevention and Health Promotion. Healthy People 2010 Online Documents Accessed at http://www.healthypeople.gov/Document/ on October 24 2008.
Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey. Accessed at http://www.cdc.gov/nchs/nhanes.htm on July 13 2009.
World Health Organization. Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee 1995, WHO Technical Report Series 854.
Heitmann BL . Ten-year trends in overweight and obesity among Danish men and women aged 30–60 years. Int J Obes Relat Metab Disord 2000; 24: 1347–1352.
Gutierrez-Fisac JL, Regidor E, Banegas Jr B, Rodriguez AF . The size of obesity differences associated with educational level in Spain 1987 and 1995/97. J Epidemiol Community Health 2002; 56: 457–460.
Lindstrom M, Isacsson SO, Merlo J . Increasing prevalence of overweight, obesity and physical inactivity: two population-based studies 1986 and 1994. Eur J Public Health 2003; 13: 306–312.
Charafeddine R, Van OH, Demarest S . Trends in social inequalities in obesity: Belgium, 1997 to 2004. Prev Med 2009; 48: 54–58.
Marques-Vidal P, Bovet P, Paccaud F, Chiolero A . Changes of overweight and obesity in the adult Swiss population according to educational level, from 1992 to 2007. BMC Public Health 2010; 10: 87.
Lahti-Koski M, Seppanen-Nuijten E, Mannisto S, Harkanen T, Rissanen H, Knekt P et al. Twenty-year changes in the prevalence of obesity among Finnish adults. Obes Rev 2010; 11: 171–176.
Zhang Q, Wang Y . Trends in the association between obesity and socioeconomic status in US adults: 1971 to 2000. Obes Res 2004; 12: 1622–1632.
Swinburn B, Sacks G, Ravussin E . Increased food energy supply is more than sufficient to explain the US epidemic of obesity. Am J Clin Nutr 2009; 90: 1453–1456.
French SA . Public health strategies for dietary change: schools and workplaces. J Nutr 2005; 135: 910–912.
Baker EA, Kelly C, Barnidge E, Strayhorn J, Schootman M, Struthers J et al. The Garden of Eden: acknowledging the impact of race and class in efforts to decrease obesity rates. Am J Public Health 2006; 96: 1170–1174.
Patrick H, Nicklas TA . A review of family and social determinants of children's eating patterns and diet quality. J Am Coll Nutr 2005; 24: 83–92.
Ayala GX, Rogers M, Arredondo EM, Campbell NR, Baquero B, Duerksen SC et al. Away-from-home food intake and risk for obesity: examining the influence of context. Obesity (Silver Spring) 2008; 16: 1002–1008.
Brownell KD, Farley T, Willett WC, Popkin BM, Chaloupka FJ, Thompson JW et al. The public health and economic benefits of taxing sugar-sweetened beverages. N Engl J Med 2009; 361: 1599–1605.
Centers for Disease Control Prevention. Prevalence of regular physical activity among adults—United States, 2001 and 2005. MMWR Morb Mortal Wkly Rep 2007; 56: 1209–1212.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Disclaimer
The findings and conclusions in this article are those of the authors and do not represent the official position of the Centers for Disease Control and Prevention.
Rights and permissions
About this article
Cite this article
Ford, E., Li, C., Zhao, G. et al. Trends in obesity and abdominal obesity among adults in the United States from 1999–2008. Int J Obes 35, 736–743 (2011). https://doi.org/10.1038/ijo.2010.186
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2010.186
Keywords
This article is cited by
-
Identification of potential causal variants for premature ovarian failure by whole exome sequencing
BMC Medical Genomics (2020)
-
Associations of the ages at menarche and menopause with blood pressure and hypertension among middle-aged and older Chinese women: a cross-sectional analysis of the baseline data of the China Health and Retirement Longitudinal Study
Hypertension Research (2019)
-
Gastroösophageale Refluxerkrankung und geschlechtsspezifische Unterschiede
Der Gastroenterologe (2019)
-
A Comparative Study of Spatial Distribution of Gastrointestinal Cancers in Poverty and Affluent Strata (Kermanshah Metropolis, Iran)
Journal of Gastrointestinal Cancer (2019)
-
Sexual Dimorphism in Cardiovascular Disease Risk and Risk Factors Among Vegetarians: an Exploration of the Potential Mechanisms
Current Atherosclerosis Reports (2019)