Abstract
Objective:
To analyze the changes in vitamin B6 status in women following slightly hypocaloric diets based on the relative increase consumption of foods whose intakes are below those recommended, and to study how these changes influence the proportion of fat-free mass.
Design:
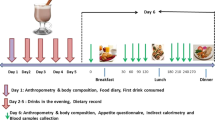
Intervention study of two slightly hypocaloric diets: diet V (increased consumption of vegetables), or diet C (increased consumption of cereals, especially breakfast cereals).
Subjects:
A total of 49 women with a body mass index (BMI) of 25–35 kg/m2.
Measurements:
Dietetic, anthropometric and biochemical data were collected at the start of the study and at 2 and 6 weeks.
Results:
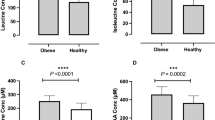
Both the C and V subjects showed a reduction in their energy intake, body weight, BMI and fat mass. Pyridoxine intake increased in both groups and plasma pyridoxal phosphate (PLP) levels increased only with diet C. An association was found between the increase in plasma PLP at 6 weeks and the increase in pyridoxine intake (r=0.451; P<0.01). Multiple regression analysis showed a positive association between the increase in PLP at the end of the study and the increases in the pyridoxine intake, B6 density or B6/protein ratio. At the end of the study, and only in those women whose PLP levels were increased, the higher the increase in PLP level, the higher the increase in fat-free mass percentage (r=0.4426, P<0.05)
Conclusions:
Interventions aimed at weight control should also try to maintain or improve nutritional status. A diet rich in cereals (especially fortified breakfast cereals) appears to be useful in improving vitamin B6 status. Such an improvement could help maintain fat-free mass during periods of weight loss.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Spinneker A, Sola R, Lemmen V, Castillo MJ, Pietrzik K, González-Gross M . Vitamin B6 status, deficiency and its consequences—an overview. Nutr Hosp 2007; 22: 7–24.
O'Neale J (ed). Metabolism and Nutrition. 2nd edn. Mosby: London, 2003.
Biolo G, Ciocchi B, Stulle M, Bosutti A, Barazzoni R, Zanetti M et al. Calorie restriction accelerates the catabolism of lean body mass during 2 wk of bed rest. Am J Clin Nutr 2007; 86: 366–372.
Manore MM . Effect of physical activity on thiamine, riboflavin, and vitamin B6 Requirements. Am J Clin Nutr 2000; 72: 598S–606S.
Neumark-Sztainer D, Hannan PJ, Story M, Perry CL . Weight-control behaviors among adolescent girls and boys: implications for dietary intake. J Am Diet Assoc 2004; 104: 913–920.
van der Beek EJ, Lowik MRH, Hulshof KFAM, Kistemaker C . Combinations of low thiamin, riboflavin, vitamin B6 and vitamin C intake among Dutch adults. (Dutch Nutrition Surveillance System). J Am Coll Nutr 1994; 13: 383–391.
World Health Organization (WHO). Energy and Protein Requirements. Report of a joint FAO/WHO/ONU expert consultation. Technical report series 724, World Health Organization: Geneva, 1985.
Department of Nutrition. Food composition tables. In: Ortega RM, López-Sobaler AM, Requejo A, Andrés P (eds). Food Composition. A Basic Tool for Assessing Nutritional Status. Complutense: Madrid, 2004, pp 15–81.
Ortega RM, Requejo AM, López-Sobaler AM, Navia B, Perea JM, Mena MC et al. Knowledge of what constitutes a balanced diet and its relationship with food habits in university students. Nutr Clin 2000; 20: 19–25.
Navia B, Ortega RM, Requejo AM, Mena MC, Perea JM, López-Sobaler AM . Influence of the desire to lose weight on food habits, and knowledge of the characteristics of a balanced diet, in a group of Madrid university students. Eur J Clin Nutr 2003; 57: 90S–93S.
Basiotis PP, Carlson A, Gerrior SA, Juan WY, Lino M . The Healthy Eating Index: 1999–2000. Center for Nutrition Policy and Promotion, Department of Agriculture (USDA): USA, 2002.
Ortega RM, López-Sobaler AM, Rodríguez-Rodríguez E, Bermejo LM, García González L, López Plaza B . Response to a weight control program based on approximating the diet to its theoretical ideal. Nutr Hosp 2005; 20: 393–402.
Ortega RM, Requejo AM, López-Sobaler AM . Activity questionnaire. In: Requejo AM, Ortega RM (eds). Nutriguía. Manual of Clinical Nutrition in Primary Care. Complutense: Madrid, 2006. pp 468.
Ortega RM, Requejo AM, Quintas ME, Sánchez-Quiles B, López-Sobaler AM, Andrés P . Estimated energy balance in female university students: differences with respect to body mass index and concern about body weight. Int J Obes 1996; 20: 1127–1129.
World Health Organization (WHO). Methodology of Nutritional Surveillance. Physical Condition: Use and Interpretation of Anthropometric Data. Report of a joint FAO/UNICEF/WHO expert consultation. Technical Report Series 854, World Health Organization: Geneva, 1995.
Siri WE . Gross composition of the body. In: Lawrence JH, Tobias CA (eds). Advances in Biological and Medical Physics. Academy Press: New York, 1956, pp 239–280.
Durnin JV, Womersley J . Body fat assessed from total body density and its estimation from skinfold thickness: measurements on 481 men and women aged from 16 to 72 years. Br J Nutr 1974; 32: 77–97.
Ortega RM, Requejo AM, López-Sobaler AM . Questionnaires for dietetic studies and the assessment of nutritional status. In: Requejo AM, Ortega RM (eds). Nutriguía. Manual of Clinical Nutrition in Primary Care. Complutense: Madrid, 2006, pp 456–459.
Department of Nutrition. Recommended daily intakes of energy and nutrients for the Spanish population. In: Ortega RM, López-Sobaler AM, Requejo A, Andrés P (eds). Food Composition. A Basic Tool for Assessing Nutritional Status. Complutense: Madrid, 2004, pp 82–85.
Ortega RM, López-Sobaler AM, Andrés P, Requejo AM, Molinero LM . DIAL software for assessing diets and food calculations. Departamento de Nutrición (UCM) y Alce Ingeniería, S.A. Version current 2004. Internet: http://www.alceingenieria.net/nutricion.htm (accessed 17 June 2008).
Poon HC, Schmidt BM . Enzymatic fluorometric assay for plasma pyridoxal 5′-phosphate. Clin Biochem 1991; 24: 149–152.
Institute of Medicine. DRI Reference Intakes for Thiamin, Riboflavin, Niacin, Vitamin B6, Folate, Vitamin B12, Pantothenic Acid, Biotin, and Choline. National Academy Press: Washington, DC, 1998.
Hansen CM, Leklem JE, Miller LT . Vitamin B-6 status indicators decrease in women consuming a diet high in pyridoxine glucoside. J Nutr 1996; 126: 2512–2518.
Ronnenberg AG, Goldman MB, Aitken IW, Xu X . Anemia and deficiencies of folate and vitamin B-6 are common and vary with season in Chinese women of childbearing age. J Nutr 2000; 130: 2703–2710.
Hansen CM, Shultz TD, Kwak HK, Memon HS, Leklem JE . Assessment of vitamin B-6 status in young women consuming a controlled diet containing four levels of vitamin B-6 provides an estimated average requirement and recommended dietary allowance. J Nutr 2001; 131: 1777–1786.
Miller JW, Green R, Mungas DM, Reed BR, Jagust WJ . Homocysteine, vitamin B6, and vascular disease in AD patients. Neurology 2002; 58: 1471–1475.
Elmadfa I, Majchrzak D, Rust P, Genser D . The thiamine status of adult humans depends on carbohydrate intake. Int J Vitam Nutr Res 2001; 71: 217–221.
Ortega RM, López-Sobaler AM, Andrés P, Rodriguez-Rodriguez E, Aparicio A, Bermejo LM et al. Changes in folate status in overweight/obese women following two different weight control programmes based on an increased consumption of vegetables or fortified breakfast cereals. Br J Nutr 2006; 96: 712–718.
Ortega RM, Andrés P, López-Sobaler AM, Rodriguez-Rodriguez E, Aparicio A, Bermejo LM et al. Changes in thiamin intake and blood levels in young, overweight/obese women following hypocaloric diets based on the increased relative consumption of cereals or vegetables. Eur J Clin Nutr 2007; 61: 77–82.
Rodríguez-Rodríguez E, López-Sobaler AM, Andrés P, Aparicio A, Navia B, Ortega RM . Modification of iron status in young overweight/mildly obese women by two dietary interventions designed to achieve weight loss. Ann Nutr Metab 2007; 51: 367–373.
Reynolds RD . Bioavailability of vitamin B-6 from plant foods. Am J Clin Nutr 1988; 48 (3 Suppl): 863–867.
Preziosi P, Galan P, Deheeger M, Yacoub N, Drewnowski A, Hercberg S . Breakfast type, daily nutrient intakes and vitamin and mineral status of French children, adolescents, and adults. J Am Coll Nutr 1999; 18: 171–178.
Galvin MA, Kiely M, Flynn A . Impact of ready-to-eat breakfast cereal (RTEBC) consumption on adequacy of micronutrient intakes and compliance with dietary recommendations in Irish adults. Public Health Nutr 2003; 6: 351–363.
Gibson S . Micronutrient intakes, micronutrient status and lipid profiles among young people consuming different amounts of breakfast cereals: further analysis of data from the National Diet and Nutrition Survey of Young People aged 4–18 years. Public Health Nutr 2003; 6: 815–820.
Melanson KJ, Angelopoulos TJ, Nguyen VT, Martini M, Zukley L, Lowndes J et al. Consumption of whole-grain cereals during weight loss: effects on dietary quality, dietary fiber, magnesium, vitamin B-6, and obesity. J Am Diet Assoc 2006; 106: 1380–1388.
Miller LT, Leklem JE, Shultz TD . The effect of dietary protein on the metabolism of vitamin B-6 in humans. J Nutr 1985; 115: 1663–1672.
NCR. National Research Council. Recommended Dietary Allowances. 10th edn. National Academy Press: Washington DC, 1989.
Chang SJ, Hsiao LJ, Lee YC, Hsuen SY . Vitamin B6 status assessment in relation to dietary intake in high school students aged 16–18 years. Br J Nutr 2007; 97: 764–769.
Battezzati A, Bertoli S, San Romerio A, Testolin G . Body composition: an important determinant of homocysteine and methionine concentrations in healthy individuals. Nutr Metab Cardiovasc Dis 2007; 17: 525–534.
Acknowledgements
This work was financed by Kellogg España via the Universidad-Empresa project 362/2003. RMO, AMLS and PA contributed to the study design, and ARN, LMB, and ERR performed the data collection. RMO, AMLS, ARN, ERR, PA and LMB were involved in data analysis and the interpretation of results. ERR, RMO and AMLS contributed to the writing of the paper.
Author information
Authors and Affiliations
Corresponding author
Additional information
Conflict of interest/Disclosure
None of the authors have any personal or financial conflicts of interest.
Rights and permissions
About this article
Cite this article
Rodríguez-Rodríguez, E., López-Sobaler, A., Navarro, A. et al. Vitamin B6 status improves in overweight/obese women following a hypocaloric diet rich in breakfast cereals, and may help in maintaining fat-free mass. Int J Obes 32, 1552–1558 (2008). https://doi.org/10.1038/ijo.2008.131
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2008.131
Keywords
This article is cited by
-
Synergistic effect of Lactobacillus gasseri and Cudrania tricuspidata on the modulation of body weight and gut microbiota structure in diet-induced obese mice
Applied Microbiology and Biotechnology (2020)
-
Chronic Effects of Pyridoxine in the Gerbil Hippocampal CA1 Region after Transient Forebrain Ischemia
Neurochemical Research (2012)