Abstract
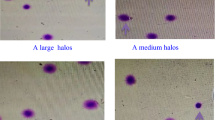
The clinical significance of sperm DNA damage lies in its association with natural conception rates and also might have a serious consequence on developmental outcome of the newborn. The aim of the present study is to determine whether stress and everyday life factors are associated with sperm DNA damage in adult men. The study population consisted of 286 men who attended the infertility clinic for diagnostic purposes and who had normal semen concentration of 20–300 m ml−1 or with slight oligozoospermia (semen concentration of 15–20 m ml−1) (WHO, 1999). Participants were interviewed and provided a semen sample. The sperm chromatin structure assay was assessed using flow cytometry. In the present study, we found evidence for a relationship between sperm DNA damage parameters and everyday life factors. High and medium level of occupational stress and age increase DNA fragmentation index (P=0.03, P=0.004 and P=0.03, respectively). Other lifestyle factors that were positively associated with percentage of immature sperms (high DNA stainability index) included: obesity and cell phone use for more than 10 years (P=0.02 and P=0.04, respectively). Our findings indicate that stress and lifestyle factor may affect sperm DNA damage. Data from the present study showed a significant effect of age, obesity, mobile phone radiation and occupational stress on sperm DNA damage. As DNA fragmentation represents an extremely important parameter indicative of infertility and potential outcome of assisted reproduction treatment, and most of the lifestyle factors are easily modifiable, the information about factors that may affect DNA damage are important.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Erenpreiss J, Elzanaty S, Giwercman A . Sperm DNA damage in men from infertile couples. Asian J Androl 2008; 10: 786–790.
Venkatesh S, Singh A, Shamsi MB, Thilagavathi J, Kumar R, Mitra DK et al. Clinical significance of sperm DNA damage threshold value in the assessment of male infertility. Reprod Sci 2011; 18: 1005–1013.
Guzick DS, Overstreet JW, Factor-Litvak P, Brzail CK, Nakajima ST, Coutifaris C et al. Sperm morphology, motility and concentration in fertile and infertile men. N Engl J Med 2001; 345: 1388–1393.
Virro MR, Larson-Cook KL, Everson DP . Sperm chromatin structure assay (SCSA) parameters are related to fertilization, blastocyst development, and ongoing pregnancy in in vitro fertilization and intracytoplasmic sperm injection cycles. Fertil Steril 2004; 81: 1289–1295.
Bungum M, Humaidan P, Axmon A, Spano M, Bungum L, Erenpreiss J et al. Sperm DNA integrity assessment in prediction of assisted reproduction technology outcome. Hum Reprod 2007; 22: 174–179.
Ménézo YJ, Hazout A, Panteix G, Robert F, Rollet J, Cohen-Bacrie P et al. Antioxidants to reduce sperm DNA fragmentation: an unexpected adverse effect. Reprod BioMed Online 2007; 14: 418–421.
Wyrobek AJ, Eskenazi B, Young S, Arnheim N, Tiemann-Boege I, Jabs EW et al. Advancing age has differential effects on DNA damage, chromatin integrity, gene mutations, and aneuploidies in sperm. Proc Natl Acad Sci USA 2006; 103: 9601–9606.
Schmid TE, Eskenazi B, Baumgartner A, Marchetti F, Young S, Weldon R et al. The effects of male age on sperm DNA damage in healthy non-smokers. Hum Reprod 2007; 22: 180–187.
Taha EA, Ez-Aldin AM, Sayed SK, Ghandour NM, Mostafa T . Effect of smoking on sperm vitality, DNA integrity, seminal oxidative stress, zinc in fertile men. Urology 2012; 80: 822–825.
Fariello RM, Pariz JR, Spaine DM, Gozzo FC, Pilau EJ, Fraietta R et al. Effect of smoking on the functional aspects of sperm and seminal plasma protein profiles in patients with varicocele. Hum Reprod 2012; 27: 3140–3149.
Vagnini L, Baruffi RL, Mauri AL, Petersen CG, Massaro FC, Pontes A et al. The effects of male age on sperm DNA damage in an infertile population. Reprod Biomed Online 2007; 15: 514–519.
Fariello RM, Pariz JR, Spaine DM, Cedenho AP, Bertolla RP, Fraietta R . Association between obesity and alteration of sperm DNA integrity and mitochondrial activity. BJU Int 2012; 110: 863–867.
La Vignera S, Condorelli RA, Vicari E, Calogero AE . Negative effect of increased body weight on sperm conventional and nonconventional flow cytometric sperm parameters. J Androl 2012; 33: 53–58.
Dupont C, Faure C, Sermondade N, Boubaya M, Eustache F, Clement P et al. Obesity leads to higher risk of sperm DNA damage in infertile patients. Asian J Androl 2013; 15: 622–625.
Desai NR, Kesari KK, Agarwal A . Pathophysiology of cell phone radiation: oxidative stress and carcinogenesis with focus on male reproductive system. Reprod Biol Endocrinol 2009; 7: 114.
WHO Laboratory Manual for the Examination of Human Semen and Sperm-Cervical Mucus Interaction, 4th edn. Cambridge University Press: Cambridge, UK, 1999.
Jurewicz J, Radwan M, Sobala W, Ligocka D, Radwan P, Bochenek M et al. Lifestyle and semen quality- role of modifiable risk factors. Syst Biol Reprod Med 2014; 60: 43–51.
Dudek B, Waszkowska M, Merecz D, Hanke W. Employees’ Protection Against Occupational Stress (in polish), 2nd edn. Nofer Institute of Occupational Medicine, Publishing house of Nofer Institute of Occupational Medicine: Lodz, Poland, 2004.
World Health Organization (2012). Global database on body mass index 2012. Available at http://apps.who.int/bmi/index.jsp?introPage=intro_3.html. Accessed on 25 November 2012.
Ainsworth BE, Haskell WL, Leon A, Jacobs DR Jr, Montoye HJ, Sallis JF et al. Compendium of physical activities— classification of energy costs of human physical activities. Med Sci Sports Exerc 1993; 25: 71–80.
Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc 2000; 32: 498–516.
Kruger TF, Acosta AA, Simmons KF, Swanson RJ, Matta JF, Oehninger S . Predictive value of abnormal sperm morphology in in vitro fertilization. Fertil Steril 1988; 49: 112–117.
ASRM Practice Committee. Report on optimal evaluation of the infertile male. Fertil Steril 2006; 86: 202–209.
Evenson DP . Sperm chromatin structure assay (SCSA®). Methods Mol Biol 2013; 927: 147–164.
Evenson DP, Larson K, Jost LK . The sperm chromatin structure assay (SCSATM): clinical use for detecting sperm DNA fragmentation related to male infertility and comparisons with other techniques. Andrology Lab Corner. J Androl 2002; 23: 25–43.
R Core Team (2013) R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing: Vienna, Austria, ISBN 3-900051-07-0, URL http://www.R-project.org/.
Hjollund NH, Bonde JP, Henriksen TB, Giwercman A, Olsen J . Job strain and male fertility. Epidemiol 2004; 15: 114–117.
Sheiner EK, Sheiner E, Carel R, Potashnik G, Shoham- Vardi I . Potential association between male infertility and occupational psychological stress. J Occup Environ Med 2002; 44: 1093–1099.
El-Helaly M, Awadalla N, Mansour M, El-Biomy Y . Workplace exposures and male infertility- a case-control study. IJOMEH 2010; 23: 331–338.
Jurewicz J, Hanke W, Sobala W, Merecz D, Radwan M . The effect of stress on the semen quality (in polish). Med Pr 2010; 61: 607–613.
Jurewicz J, Radwan M, Merecz-Kot D, Sobala W, Ligocka D, Radwan P et al. Occupational, life stress and family functioning-does it affect semen quality? Ann Hum Biol 2014; 47: 220–228.
Chavarro JE, Toth TL, Wright DL, Meeker JD, Hauser R . Body mass index in relation to semen quality, sperm DNA integrity, and serum reproductive hormone levels among men attending an infertility clinic. Fertil Steril 2010; 93: 2222–2231.
Kort HI, Massey JB, Elsner CW, Mitchell-Leef D, Shapiro DB, Witt MA . Impact of body mass index values on sperm quality and quantity. J Androl 2006; 27: 450–452.
Hammiche JS, Laven JC, Boxmeer GR, Dohle EA, Steegers RP, Steegers-Theunissen M . Sperm quality decline among men below 60 years of age undergoing IVF or ICSI treatment. J Androl 2011; 32: 70–76.
Rybar R, Kopecka V, Prinosilova P, Markova P, Rubes J . Male obesity and age in relationship to semen parameters and sperm chromatin integrity. Andrologia 2011; 43: 286–291.
Rago R, Salacone P, Caponecchia L, Sebastianelli L, Marcucci I, Calogero AE et al. The semen quality of the mobile phone users. J Endocrinol Invest 2013; 36: 970–974.
Valavanidis A, Vlachogianni T, Fiotakis K . Tobacco smoke: involvement of reactive oxygen species and stable free radicals in mechanisms of oxidative damage, carcinogenesis and synergistic effects with other respirable particles. Int J Environ Res Public Health 2009; 6: 445–462.
Hengstler JG, Bolm-Audorff U, Faldum A, Janssen K, Reifenrath M, Gotte W et al. Oesch occupational exposure to heavy metals: DNA damage induction and DNA repair inhibition prove co-exposures to cadmium, cobalt and lead as more dangerous than hitherto expected. Carcinogenesis 2003; 24: 63–73.
Arabi M . Nicotinic infertility: assessing DNA and plasma membrane integrity of human spermatozoa. Andrologia 2004; 36: 305–310.
Linschooten JO, Laubenthal J, Cemeli E, Baumgartner A, Anderson D, Sipinen VE et al. Incomplete protection of genetic integrity of mature spermatozoa against oxidative stress. Reprod Toxicol 2011; 32: 106–111.
Elshal MF, El-Sayed IH, Elsaied MA, El-Masry SA, Kumosani TA . Sperm head defects and disturbances in spermatozoal chromatin and DNA integrities in idiopathic infertile subjects: association with cigarette smoking. Clin Biochem 2009; 42: 589–594.
Li Y, Lin H, Ma M, Li L, Cai M, Zhou N et al. Semen quality of 1346 healthy men, results from the Chongqing area of southwest China. Hum Reprod 2009; 24: 459–469.
Trummer H, Habermann H, Haas J, Pummer K . The impact of cigarette smoking on human semen parameters and hormones. Hum Reprod 2002; 17: 1554–1559.
Vaamonde D, Da Silva-Grigoletto ME, Garcı'a-Manso JM, Barrera N, Vaamonde-Lemos R . Physically active men show better semen parameters and hormone values than sedentary men. Eur J Appl Physiol 2012; 112: 3267.
Sharma R, Biedenharn KR, Fedor JM, Agarwal A . Lifestyle factors and reproductive health: taking control of your fertility. Reprod Biol Endocrinol 2013; 11: 66.
Oldereid NB, Rui H, Purvis K . Life styles of men in barren couples and their relationship to sperm quality. Int J Fertil 1992; 37: 343–349.
Ramlau-Hansen CH, Thulstrup AM, Bonde JP, Olsen J, Bech BH . Semen quality according to prenatal coffee and present caffeine exposure: two decades of follow-up of a pregnancy cohort. Hum Reprod 2008; 23: 2799–2805.
Jensen TK, Swan SH, Skakkebaek NE, Rasmussen S, Jorgensen N . Caffeine intake and semen quality in population of 2554 young Danish men. Am J Epidemiol 2010; 171: 883–891.
Sobreiro BP, Lucon AM, Pasqualotto FF, Hallak J, Athayde KS, Arap S . Semen analysis in fertile patients undergoing vasectomy: reference values and variations according to age, length of sexual abstinence, seasonality, smoking habits and caffeine intake. Sao Paulo Med J 2005; 123: 161–166.
Li Y, Lin H, Li Y, Cao J . Association between socio-psycho-behavioral factors and male semen quality: Systematic review and meta-analyses. Fertil Steril 2011; 95: 116–123.
Gaur DS, Talekar MS, Pathak VP . Alcohol intake and cigarette smoking: Impact of two major lifestyle factors on male fertility. Indian J Pathol Microbiol 2010; 53: 35–40.
Koch OR, Pani G, Borrello S, Colavitti R, Cravero A, Farrè S et al. Oxidative stress and antioxidant defenses in ethanol-induced cell injury. Mol Aspects Med 2004; 25: 191–198.
Cederbaum AI, Lu Y, Wu D . Role of oxidative stress in alcohol-induced liver injury. Arch Toxicol 2009; 83: 519–548.
Kefer JC, Agarwal A, Sabanegh E . Role of antioxidants in the treatment of male infertility. Int J Urol 2009; 16: 449–457.
Evenson DP, Larson KL, Jost LK . Sperm chromatin structure assay: its clinical use for detecting sperm DNA fragmentation in male infertility and comparisons with other techniques. J Androl 2002; 23: 25–43.
Schulte RT, Ohl DA, Sigman M, Smith GD . Sperm DNA damage in male infertility: etiologies, assays and outcomes. J Assist Reprod Genet 2010; 27: 3–12.
Aitken RJ, De Iuliis GN . On the possible origins of DNA damage in human spermatozoa. Mol Hum Reprod 2010; 16: 3–13.
Aktan G, Dogru-Abbasoglu S, Kucukgergin C, Kadioglu A, Ozdemirler-Erata G, Kocak-Toker N . Mystery of idiopathic male infertility: is oxidative stress an actual risk? Fertil Steril 2013; 99: 1211–1215.
Atig F, Raffa M, Ali HB, Abdelhamid K, Saad A, Ajina M . Altered antioxidant status and increased lipid per-oxidation in seminal plasma of tunisian infertile men. Int J Biol Sci 2012; 8: 139–149.
Khosravi F, Valojerdi MR, Amanlou M, Karimian L, Abolhassani F . Relationship of seminal reactive nitrogen and oxygen species and total antioxidant capacity with sperm DNA fragmentation in infertile couples with normal and abnormal sperm parameters. Andrologia 2012; 46: 17–23.
Wright C, Milne S, Leeson H, Sperm DNA . damage caused by oxidative stress: modifiable clinical, lifestyle and nutritional factors in male infertility. Rep BioMed Online 2014; 28: 684–703.
Eskiocak S, Gozen AS, Taskiran A, Kilic AS, Eskiocak M, Gulen S . Effects of psychological stress on the L-arginine-nitric oxide pathway and semen quality. Braz J Med Biol Res 2006; 39: 581–585.
Eskiocak S, Gozen AS, Kilic AS, Molla S . Association between mental stress & some antioxidant enzymes of seminal plasma. Ind J Med Res 2005; 112: 491–496.
Darzynkiewicz Z, Juan G, Li X, Gorczyca W, Murakami T, Traganos F . Cytometry in cell necrobiology: analysis of apoptosis and accidental cell death (necrosis). Cytometry 1997; 27: 1–20.
WHO Laboratory Manual for the Examination of Human Semen and Sperm-Cervical Mucus Interaction, 5th edn. Cambridge University Press: Cambridge, UK, 2010.
Bungum M . Sperm DNA integrity assessment: a new tool in diagnosis and treatment of fertility. Obstet Gynecol Int 2012; 2012: 531042.
Erenpreiss J, Jepson K, Giwercman A, Tsarev I, Erenpreisa J, Spano M . Toluidine blue cytometry test for sperm DNA conformation: comparison with the flow cytometric sperm chromatin structure and TUNEL assays. Hum Reprod 2004; 19: 2277–2282.
Chohan KR, Griffin JT, Lafromboise M, De Jonge CJ, Carrell DT . Comparison of chromatin assays for DNA fragmentation evaluation in human sperm. J Androl 2006; 27: 53–59.
Garcia-Peiro A, Oliver-Bonet M, Navarro J, Abad C, Guitart M, Amengual MJ et al. Dynamics of sperm DNA fragmentation in patients carrying structurally rearranged chromosomes. Int J Androl 2011; 34: e546–e553.
The Practice Committee of the American Society for Reproductive Medicine. The clinical utility of sperm DNA integrity testing. Fertil Steril 2008; 90: 178–180.
Henkel R, Hoogendijk CF, Bouic PJ, Kruger TF . TUNEL assay and SCSA determine different aspects of sperm DNA damage. Andrologia 2010; 42: 305–313.
Ribas-Maynou J, Garcia-Peiro A, Fernandez-Encinas A, Abad C, Amengul MJ, Prada E et al. Comprahensive analysis of sperm DNA fragmentation by five different assays: TUNEL assay, SCSA, SCD test and alkaline and natural Comet assay. Andrology 2013; 5: 715–722.
Acknowledgements
This study was performed under the project ‘Epidemiology of reproductive hazards - multicenter study in Poland’ supported by National Center for Research and Development in Poland, with grant no. PBZ-MEiN-/8/2//2006; contract no. K140/P01/2007/1.2.1.2. and the project ‘Lifestyle factors, parabens and semen quality’ financed with a grant for statutory activity IMP 10.23/2015.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Radwan, M., Jurewicz, J., Merecz-Kot, D. et al. Sperm DNA damage—the effect of stress and everyday life factors. Int J Impot Res 28, 148–154 (2016). https://doi.org/10.1038/ijir.2016.15
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijir.2016.15