Abstract
Germ-line mutations in MLH1, MSH2, MSH6, and PMS2 have been shown to cause Lynch syndrome. The penetrance of the cancer and tumor spectrum has been repeatedly studied, and multiple professional societies have proposed clinical management guidelines for affected individuals. Several studies have demonstrated a reduced penetrance for monoallelic carriers of PMS2 mutations compared with the other mismatch repair (MMR) genes, but clinical management guidelines have largely proposed the same screening recommendations for all MMR gene carriers. The authors considered whether enough evidence existed to propose new screening guidelines specific to PMS2 mutation carriers with regard to age at onset and frequency of colonic screening. Published reports of PMS2 germ-line mutations were combined with unpublished cases from the authors’ research registries and clinical practices, and a discussion of potential modification of cancer screening guidelines was pursued. A total of 234 monoallelic PMS2 mutation carriers from 170 families were included. Approximately 8% of those with colorectal cancer (CRC) were diagnosed before age 30, and each of these tumors presented on the left side of the colon. As it is currently unknown what causes the early onset of CRC in some families with monoallelic PMS2 germline mutations, the authors recommend against reducing cancer surveillance guidelines in families found having monoallelic PMS2 mutations in spite of the reduced penetrance.
Genet Med 18 1, 13–19.
Similar content being viewed by others
Main
In the mid-1990s, through a convergence of scientific observations by yeast geneticists, cancer geneticists, and clinicians, the cause of Lynch syndrome, formerly referred to as hereditary nonpolyposis colon cancer, was found to be heterozygous DNA mismatch repair (MMR) gene germ-line mutations (reviewed by Boland and Lynch1). Mutations in MSH2 were reported in 1993 and mutations in MLH1 were reported in 1994.2,3,4,5 PMS2 was cloned and found to be causative of Lynch syndrome in 1994.6 MSH6 was added to the list in 1997.7 Although additional genes participate in the DNA MMR process, only these four are well established as causes of Lynch syndrome. Over the past two decades, information on disease penetrance and spectrum accumulated, and multiple professional societies and experts have issued recommendations for the management of individuals with Lynch syndrome; these recommendations are generally written to encompass carriers of mutations in any of these four genes8,9,10 ( Tables 1 and 2 ).
In 1995, Hamilton et al.11 studied 14 families with “Turcot syndrome” (the co-occurrence of colorectal polyposis with a primary tumor of the central nervous system). Germ-line APC mutations were found in 10 families, and three of the remaining four cases had evidence of a tumor DNA MMR defect. Germ-line mutations were discovered in two cases: one in MLH1 and one in PMS2. The PMS2 mutation occurred in an 18-year-old man with colonic adenomas, a glioblastoma at age 4 years, and café-au-lait spots. His sister had a history of rectal carcinoma. In a similarly affected, consanguineous family, Trimbath et al.12 identified homozygous PMS2 mutations in affected members. In 2004, De Vos et al.13 noted that the heterozygous family members of a homozygous case seemed to have no cancer predisposition whatsoever, raising the possibility that PMS2 predisposed to cancer only when biallelic mutations were present. To underscore this possibility, De Vos et al. conducted further molecular analysis in the family with PMS2 Turcot syndrome described by Hamilton et al. and identified a second PMS2 mutation. Analysis of PMS2 for mutations has turned out to be far more complex than analysis of the other MMR genes because of the existence of multiple pseudogenes.14,15 As a result, clinical testing for PMS2 mutations was not available until relatively recently, and even now there exists some uncertainty about how many mutations may be missed or miscalled as a result of the presence of pseudogenes.15
Despite limitations in mutation detection technologies, since 2004 multiple studies have confirmed an increased risk for cancer in heterozygous carriers of PMS2 mutations, although penetrance for cancer is lower than for the other three MMR genes. Based on 55 families with presumably monoallelic PMS2 mutations, Senter et al.16 reported risk for colorectal cancer (CRC) as 15–20% by age 70, well less than half that of MLH1 and MSH2 mutation carriers. The study, which ascertained cases based on tumors with selective loss of expression of PMS2 (predominantly colorectal but endometrial cases as well), found 6 cases (out of 99) with biallelic mutations, a proportion of biallelic mutation carriers that far exceeded that found in the other Lynch syndrome–related genes. The six biallelic cases all demonstrated an absence of the PMS2 protein in the tumor tissue and adjacent normal tissue. In a 2008 review of all published cases with biallelic MMR mutations (now known as constitutional mismatch repair deficiency), more than half of the individuals (43/78) carried PMS2 mutations, even though heterozygous PMS2 mutations are thought to account for only 1–15% of all individuals with Lynch syndrome.17,18,19,20,21 In Truninger et al.,22 the isolated absence of PMS2 by immunohistochemistry (IHC) was found in 1.5% of >1,000 consecutively collected CRC specimens from individuals undergoing surgical resection; that study showed a similar incidence of Lynch syndrome caused by mutations in PMS2 as Lynch syndrome caused by mutations in MSH2. The phenotype associated with mutations in PMS2 clearly differs in significant ways from those associated with MSH2, MLH1, and MSH6.
Historical and recent guidelines for clinical management largely combine carriers of PMS2 mutations with all cases of Lynch syndrome8 or propose delaying screening by 5 years.9 The authors, all involved in the care of individuals with Lynch syndrome, formed an unfunded ad hoc virtual working group to collate and examine the available information on PMS2 monoallelic mutation carriers to consider this question: “Are there adequate data to inform clinical management guidelines for individuals with PMS2 mutations that may deviate from those formulated for individuals with mutations in the other three Lynch syndrome genes?” A new penetrance analysis was not the objective because, like previously published cases, the ascertainment of nearly all new unpublished cases identified came from high-risk clinics or registries. Having more families collected in such a strongly biased manner would be unlikely to provide a level of evidence needed to recommend changes in practice. This is a report of the outcomes of this working group.
Methods
Published reports of PMS2 germ-line mutation carriers were identified by searching PubMed using the terms “PMS2,” “monoallelic MMR,” “Lynch syndrome,” and “hereditary non polyposis colon cancer (HNPCC).” This search yielded 4,554 publications, of which 100% of relevant reports of germ-line monoallelic PMS2 mutation carriers were included. Relevance for inclusion was cross-referenced by multiple authors. The references of all papers so identified also were reviewed for other eligible reports. All cases with putative monoallelic PMS2 germ-line mutations were abstracted. For case reports of biallelic mutation carriers, parents were presumed to be obligate monoallelic carriers, and information on their health was included if the paper provided adequate detail (which occurred infrequently). A concerted effort was made to ensure that cases presented in multiple articles were included only once in the series. Cases in which monoallelic mutations were suspected only based on tumor studies (no germ-line testing) were not included. No efforts were made to contact the authors of previous publications to request information not included in those papers.
In addition to published cases, all unpublished cases of individuals with reported monoallelic PMS2 mutations known from the authors’ research registries or clinical practices also were collected if permitted by local institutional review boards. For all cases, both published and unpublished, the following information was collected when known: gender, last known age, specific PMS2 mutation, site of CRC, age(s) at diagnosis of CRC, other non-CRC cancer diagnoses and ages at diagnoses, microsatellite instability (MSI) status of any tumor or nonmalignant tissue testing, loss of PMS2 expression by IHC of any tumor or nonmalignant tissue, and method of ascertainment of the individual. Family history collection was not included because it was inconsistently available and often incomplete.
Once collection of the entire list of cases and associated data was completed, the table was circulated to the working group for consideration. An online discussion was conducted via e-mail; the specific question was whether there was sufficient evidence to suggest that a modification of standard Lynch syndrome cancer screening guidelines9,10 was indicated for carriers of monoallelic PMS2 mutations. Discussion was moderated and recorded by M.L.G. and N.M.L. At various points in the process, summaries of the viewpoints previously expressed were provided back to the work group to facilitate continued discussion. Ongoing discussion was pursued until all viewpoints were expressed and consensus on the conclusion as articulated in this article was achieved. Throughout the discussion, all participants were invited to provide feedback on the collected data, and all authors participated at a minimum by giving their agreement to the conclusion that was finally formed.
Results
Supplementary Tables S1–S3 online show details regarding the 234 monoallelic PMS2 mutation carriers from 170 families that were included in the final data set: 129 carriers were from previously published reports and 105 were previously unreported cases. This included 90 men, 101 women, and 43 with sex not specified.
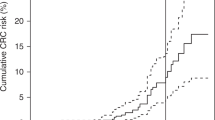
Most individuals had been diagnosed with CRC (n = 159, 68%), with a mean age of 48 years (range 22–80 years) at first CRC diagnosis (age at diagnosis was not available for four individuals) (Supplementary Table S1 online). The percentages of 155 identifiable carriers that developed CRC at age in their 20s, 30s, 40s, 50s, and 60s or above are 8% (n = 12), 20% (n = 31), 31% (n = 49), 22% (n = 34), and 19% (n = 29), respectively. Fifteen carriers had either synchronous or metachronous CRC.
Table 3 shows the distribution of CRC by colorectal subsite. None of the CRCs diagnosed at an age younger than 30 years (0 of 9 patients) were located in the ascending colon or cecum, compared with 57% (57 of 100) diagnosed at an age older than 30 years (P < 0.001). In those younger than age 30, 78% of the CRCs were in the left colon (within the splenic flexure, descending colon, sigmoid colon, rectosigmoid junction, or rectum). In PMS2 carriers with colon cancer in their 30s–80s, the percentage in the left colon ranged from 21% to 60%. Following these observations, previously published cases of biallelic MMR mutation carriers16,23 were reviewed for the CRC site and also are shown in Table 3 . In these cases, the majority of the reported CRC was in the left colon.
Of individuals with non-CRC tumors (Supplementary Tables S1 and S2 online), there were 32 women, 9 men, and 5 cases with sex not reported. The most common cancer after CRC was uterine cancer (n = 20), with an average age at diagnosis of 54.5 years (range 30–80 years). Three cases of ovarian cancer and two cases of primary peritoneal cancer were reported, with an average age at diagnosis of 53 years. Other cancers reported included cancers of the breast, duodenum and small intestine, stomach, urinary tract, brain, and central nervous system.
Tumor IHC results were known for 110 cases (IHC was performed on not only CRC but also other tumor types, as well as a large adenoma in one case); all showed isolated loss of PMS2, except one individual whose CRC showed loss of both MSH6 and PMS2 (rechecked and confirmed). MSI status was known for 51 of the cases; 50 were MSI high and 1 case of a rectal adenocarcinoma with isolated loss of PMS2 by IHC was microsatellite stable.
Seventy-six of the PMS2 mutation carriers had no history of CRC (Supplementary Tables S2 and S3 online). The average last known age was 48 years (range 18–78 years; median 47 years). Of these, 32 were abstracted from previously published reports, and 44 were from our previously unpublished clinical practice and research experiences.
Approximately 97 e-mail correspondences were sent among the group during the process, with an average of three e-mails sent from each member of the working group. After the cases were compiled and distributed to the group, an eventual consensus was formed by the group: There does not exist enough evidence to modify standard Lynch syndrome cancer screening guidelines for carriers of monoallelic PMS2 mutations as determined by current molecular testing methods.
Discussion
In a completely different context, former US Secretary of Defense Donald Rumsfeld asserted, “There are known knowns; there are things we know we know. We also know there are known unknowns; that is to say we know there are some things we do not know. But there are also unknown unknowns—the ones we don’t know we don’t know.”24 The relevance of this quotation to PMS2 is still developing, but data on PMS2 today are sufficient to know only that there remain some very important unknowns. The convergence of several factors has made understanding the clinical implications of PMS2 mutations elusive. The gene is difficult to sequence because of its structure and repetitive nature, so there was a long delay in clinical testing availability relative to the other MMR genes, reducing the available data on this gene from clinical laboratories. Multiple studies16,22,25,26 have indicated a low penetrance compared with mutations in the other Lynch syndrome genes, and our survey of available carriers shows a large number of unaffected carriers and supports this observation. Most PMS2 carriers likely are undiagnosed because they are not diagnosed with a cancer or, alternatively, affected carriers do not undergo genetic evaluation and testing because of a lack of identifiable risk factors suspicious for Lynch syndrome in their personal or family history. Universal testing for Lynch syndrome is not being performed widely and/or has not been going on long enough to have altered the situation.
In this review the authors examine a known unknown: “Are there adequate data to inform clinical management guidelines for individuals with monoallelic PMS2 mutations that may deviate from those formulated for individuals with mutations in the other three Lynch syndrome genes?” In considering the original question of the appropriateness of clinical screening recommendations for PMS2 mutation carriers, one has to balance the well-documented and accepted low penetrance (even in highly preselected cases that overestimate penetrance) and the intermittent development of CRC in strikingly young individuals: ~8% of the individuals with a CRC in this review were younger than the age of 30. The authors discussed the juxtaposition of low penetrance with a very young age at onset but were unable to resolve whether this was biologically incongruous. These properties of a genetic disorder may vary independently.
While this review did not set out to evaluate biallelic PMS2 mutation carriers (they were actively excluded), based on this limited amount of data one speculation that surfaced was how certain one could be that a very young person with CRC might not actually have biallelic mutations in PMS2, or perhaps an unidentified hypomorphic allele, given the notoriously difficult molecular analysis that this gene presents. Genetic testing for PMS2, while still difficult, has improved in recent years, and many of the published cases of PMS2 monoallelic mutation carriers may not have had deletion and duplication analysis performed because it was not available at the time. This current data set does include one young-onset case with a variant of uncertain significance in PMS2 in addition to the pathogenic mutation (case 129), and another case had 4 synchronous CRCs and 14 adenomas at age 26 (case 27), which is much more in keeping with the emerging picture of biallelic carriers.
IHC of nonmalignant tissue has been suggested as one method to distinguish monoallelic from biallelic carriers, but there are reports of expression in some tissues even in those with known biallelic mutations, so this is not a failsafe method to confirm a monoallelic mutation.27 For the majority of instances of CRC in patients younger than age 30, no information regarding IHC of nonmalignant tissue was available or it had not been tested in the individual. For three of the cases, the potential for a biallelic mutation, despite a single mutation identified by molecular analysis, was explored, and for all three cases, staining of PMS2 was present in nonmalignant tissue. Other than case 27, no other cases with early onset had multiple polyps. The clinical phenotype of café-au-lait macules was not reported in any of the cases described here but could have been overlooked. None of the cases with CRC at an age younger than 30 were diagnosed with a pediatric brain tumor or hematologic malignancy that would have suggested constitutional mismatch repair deficiency. No CRCs had occurred in the parents of the very-young-onset cases, arguing against particularly virulent monoallelic mutations resulting in disease with a very early onset and higher penetrance.
Cases of CRC diagnosed at an age younger than 30 were evaluated further to determine whether there was any pattern that distinguished them from the PMS2 mutation carriers diagnosed with cancer at older ages. One unexpected difference was that the very-young-onset cancers did not show the typical CRC site of Lynch syndrome. In fact, none of the nine cases had a right-sided tumor, whereas those diagnosed after age 30 showed the typical right-sided predisposition. Compared with MMR biallelic cases previously described by Durno et al.23 and Senter et al.16 ( Table 3 ), there does seem to be a trend toward left-sided CRCs among the published MMR biallelic carriers, similar to the observed presumed monoallelic PMS2 carriers younger than age 30, though the data are limited.
Overall, given the possible lack of the typical café-au-lait macules, hematologic or brain tumor phenotypes, and the trend toward left-sided CRCs, this group may be qualitatively and clinically different from biallelic PMS2 mutation carriers, yet also different from monoallelic PMS2 mutation carriers. Beyond a possible undetected second PMS2 mutation, another possible consideration could be the presence of a modifier of cancer risk involving another gene altogether, that is, digenic inheritance, which might result in early cancer. In this scenario, family members who inherit just the PMS2 mutation would have risks of monoallelic PMS2 carriers. Family members inheriting both the modifier and the PMS2 monoallelic mutation could be at a higher risk and more likely to develop early-onset cancers, perhaps even more left colonic predisposition. This hypothesis certainly merits additional consideration and genetic research.
One factor considered when the authors discussed screening options related to how the first case in the family presented. If this is an older-onset CRC presentation with the typical minimal family history, consistent with the PMS2 low-penetrance reports, then delaying colonoscopy for gene-carrying relatives to at least age 30 seems reasonable. In this review there were no cases of families ascertained with CRCs diagnosed at an age older than 30 that reported a history of relatives with CRCs diagnosed at an age younger than 30 (no family history data shown, and available data are incomplete). Conversely, if a family presents because of CRC at a very young age at onset, the possibility of an undetected second mutation in PMS2, other modifier gene, or digenic inheritance could be highlighted and counseled for. Screening of siblings, who may be at a 25% risk for carrying the same PMS2 genotype, may be advised to initiate CRC screening earlier, such as age 20. The children of the affected young person could also have digenic inheritance, if this was the mechanism, and so their risks might parallel that of the parent. These data suggest that perhaps the general rule of thumb to initiate screening 5 years younger than the youngest case in the family or by age 30, whichever is earliest, could be appropriate.
When looking at the reported age at onset of CRC, there is not a bimodal distribution across the decades. The percentages of the 155 carriers who developed CRC at ages in the 20s, 30s, 40s, 50s, and 60s or above are 8, 20, 31, 22, and 19%, respectively. This may be a counterargument for the existence of a biallelic or digenic subset accounting for the very-early-onset cases and suggests a very broad age at onset of CRC among monoallelic PMS2 mutation carriers.
We thus are left with the dilemma of a known unknown: What is the cause of a low-penetrance disorder that sometimes occurs with very-early-onset cancer? There is currently no convincing evidence that the very-early-onset PMS2-related cancers represent a different disorder than the later-onset PMS2-related cancers. Review of all available data on monoallelic PMS2 mutation carriers speaks against stepping back from the cancer surveillance guidelines that have been developed for CRC and endometrial cancer risks in Lynch syndrome in general, in spite of well-documented differences in CRC risks. These guidelines still seem to be reasonable for carriers of monoallelic PMS2 until data emerge that change our current understanding.
The carrier frequency of PMS2 pathogenic mutations is unknown but may be more common than the other Lynch syndrome–related genes, given the notable excess of biallelic PMS2 cases reported to date. The possibility that a hypomorphic PMS2 variant, or involvement of another gene altogether, might occur when paired with a typical pathogenic PMS2 mutation may cause a very-early-onset cancer without the clinically striking phenotype of the constitutional mismatch repair deficiency is still entirely speculative. The phenomenon of very-early-onset development of cancers in PMS2 mutation carriers merits additional research. The authors hope to encourage ongoing prospective genetic and epidemiologic studies that might one day make known today’s unknowns.
Disclosure
H.H. has received an honorarium from Invitae and Quest Diagnostics within the past 12 months. She received research funding from Myriad Genetics. The other authors declare no conflict of interest.
References
Boland CR, Lynch HT. The history of Lynch syndrome. Fam Cancer 2013;12:145–157.
Fishel R, Lescoe MK, Rao MR, et al. The human mutator gene homolog MSH2 and its association with hereditary nonpolyposis colon cancer. Cell 1993;75:1027–1038.
Leach FS, Nicolaides NC, Papadopoulos N, et al. Mutations of a mutS homolog in hereditary nonpolyposis colorectal cancer. Cell 1993;75:1215–1225.
Bronner CE, Baker SM, Morrison PT, et al. Mutation in the DNA mismatch repair gene homologue hMLH1 is associated with hereditary non-polyposis colon cancer. Nature 1994;368:258–261.
Papadopoulos N, Nicolaides NC, Wei YF, et al. Mutation of a mutL homolog in hereditary colon cancer. Science 1994;263:1625–1629.
Nicolaides NC, Papadopoulos N, Liu B, et al. Mutations of two PMS homologues in hereditary nonpolyposis colon cancer. Nature 1994;371:75–80.
Miyaki M, Konishi M, Tanaka K, et al. Germline mutation of MSH6 as the cause of hereditary nonpolyposis colorectal cancer. Nat Genet 1997;17:271–272.
Vasen HF, van der Meulen-de Jong AE, de Vos Tot Nederveen Cappel WH, Oliveira J ; ESMO Guidelines Working Group. Familial colorectal cancer risk: ESMO clinical recommendations. Ann Oncol 2009;20(suppl 4):51–53.
NCCN. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines) Genetic/Familial High-Risk Assessment: Colorectal Cancer. The NCCN Guidelines, 2014. http://www.nccn.org/professionals/physician_gls/pdf/genetics_colon.pdf. Accessed 20 March 2014.
Vasen HF, Blanco I, Aktan-Collan K, et al.; Mallorca group. Revised guidelines for the clinical management of Lynch syndrome (HNPCC): recommendations by a group of European experts. Gut 2013;62:812–823.
Hamilton SR, Liu B, Parsons RE, et al. The molecular basis of Turcot’s syndrome. N Engl J Med 1995;332:839–847.
Trimbath JD, Petersen GM, Erdman SH, Ferre M, Luce MC, Giardiello FM. Café-au-lait spots and early onset colorectal neoplasia: a variant of HNPCC? Fam Cancer 2001;1:101–105.
De Vos M, Hayward BE, Picton S, Sheridan E, Bonthron DT. Novel PMS2 pseudogenes can conceal recessive mutations causing a distinctive childhood cancer syndrome. Am J Hum Genet 2004;74:954–964.
Clendenning M, Hampel H, LaJeunesse J, et al. Long-range PCR facilitates the identification of PMS2-specific mutations. Hum Mutat 2006;27:490–495.
Vaughn CP, Baker CL, Samowitz WS, Swensen JJ. The frequency of previously undetectable deletions involving 3’ Exons of the PMS2 gene. Genes Chromosomes Cancer 2013;52:107–112.
Senter L, Clendenning M, Sotamaa K, et al. The clinical phenotype of Lynch syndrome due to germ-line PMS2 mutations. Gastroenterology 2008;135:419–428.
Wimmer K, Etzler J. Constitutional mismatch repair-deficiency syndrome: have we so far seen only the tip of an iceberg? Hum Genet 2008;124:105–122.
Peltomäki P. Deficient DNA mismatch repair: a common etiologic factor for colon cancer. Hum Mol Genet 2001;10:735–740.
Peltomäki P, Vasen H. Mutations associated with HNPCC predisposition – Update of ICG-HNPCC/INSiGHT mutation database. Dis Markers 2004;20:269–276.
Hampel H, Frankel WL, Martin E, et al. Screening for the Lynch syndrome (hereditary nonpolyposis colorectal cancer). N Engl J Med 2005;352:1851–1860.
Palomaki GE, McClain MR, Melillo S, Hampel HL, Thibodeau SN. EGAPP supplementary evidence review: DNA testing strategies aimed at reducing morbidity and mortality from Lynch syndrome. Genet Med 2009;11:42–65.
Truninger K, Menigatti M, Luz J, et al. Immunohistochemical analysis reveals high frequency of PMS2 defects in colorectal cancer. Gastroenterology 2005;128:1160–1171.
Durno CA, Holter S, Sherman PM, Gallinger S. The gastrointestinal phenotype of germline biallelic mismatch repair gene mutations. Am J Gastroenterol 2010;105:2449–2456.
Rumsfeld D. DoD News Briefing - Secretary Rumsfeld and Gen. Myers. News Transcript 12 February 2002. http://www.defense.gov/transcripts/transcript.aspx?transcriptid=2636. Accessed 19 June 2014.
Gill S, Lindor NM, Burgart LJ, et al. Isolated loss of PMS2 expression in colorectal cancers: frequency, patient age, and familial aggregation. Clin Cancer Res 2005;11:6466–6471.
Clendenning M, Senter L, Hampel H, et al. A frame-shift mutation of PMS2 is a widespread cause of Lynch syndrome. J Med Genet 2008;45:340–345.
Felton KE, Gilchrist DM, Andrew SE. Constitutive deficiency in DNA mismatch repair. Clin Genet 2007;71:483–498.
Dowty JG, Win AK, Buchanan DD, et al. Cancer risks for MLH1 and MSH2 mutation carriers. Hum Mutat 2013;34:490–497.
Bonadona V, Bonaïti B, Olschwang S, et al.; French Cancer Genetics Network. Cancer risks associated with germline mutations in MLH1, MSH2, and MSH6 genes in Lynch syndrome. JAMA 2011;305:2304–2310.
Quehenberger F, Vasen HF, van Houwelingen HC. Risk of colorectal and endometrial cancer for carriers of mutations of the hMLH1 and hMSH2 gene: correction for ascertainment. J Med Genet 2005;42:491–496.
Baglietto L, Lindor NM, Dowty JG, et al.; Dutch Lynch Syndrome Study Group. Risks of Lynch syndrome cancers for MSH6 mutation carriers. J Natl Cancer Inst 2010;102:193–201.
Hendriks YM, Wagner A, Morreau H, et al. Cancer risk in hereditary nonpolyposis colorectal cancer due to MSH6 mutations: impact on counseling and surveillance. Gastroenterology 2004;127:17–25.
Engel C, Loeffler M, Steinke V, et al. Risks of less common cancers in proven mutation carriers with lynch syndrome. J Clin Oncol 2012;30:4409–4415.
Watson P, Vasen HF, Mecklin JP, et al. The risk of extra-colonic, extra-endometrial cancer in the Lynch syndrome. Int J Cancer 2008;123:444–449.
Giardiello FM, Allen JI, Axilbund JE, et al. Guidelines on genetic evaluation and management of Lynch syndrome: a consensus statement by the U.S. Multi-Society Task Force on Colorectal Cancer. Gastrointest Endosc 2014;80:197–220.
Acknowledgements
This work was supported by grant UM1 CA167551 from the National Cancer Institute and through cooperative agreements with the following Colon Cancer Family Registry (CCFR) centers: Australasian Colorectal Cancer Family Registry (U01/U24 CA097735), Stanford Consortium Colorectal Cancer Family Registry (U01/U24 CA074799), Mayo Clinic Cooperative Family Registry for Colon Cancer Studies (U01/U24 CA074800), Ontario Registry for Studies of Familial Colorectal Cancer (U01/U24 CA074783), Seattle Colorectal Cancer Family Registry (U01/U24 CA074794), and University of Hawaii Colorectal Cancer Family Registry (U01/U24 CA074806). The content of this article does not necessarily reflect the views or policies of the National Cancer Institute or any of the collaborating centers in the CCFR, nor does mention of trade names, commercial products, or organizations imply endorsement by the US government or the CCFR. The City of Hope Clinical Cancer Genetics Community Research Network was supported in part by award RC4A153828 (primary investigator J.N.W.) from the National Cancer Institute, the Ohio State University (R01CA67941 and P30CA16058), and the National Institutes of Health (CA72851-18).
Author information
Authors and Affiliations
Corresponding author
Supplementary information
Supplementary Table S1
(DOC 735 kb)
Supplementary Table S2
(DOC 120 kb)
Supplementary Table S3
(DOC 151 kb)
Rights and permissions
About this article
Cite this article
Goodenberger, M., Thomas, B., Riegert-Johnson, D. et al. PMS2 monoallelic mutation carriers: the known unknown. Genet Med 18, 13–19 (2016). https://doi.org/10.1038/gim.2015.27
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/gim.2015.27
Keywords
This article is cited by
-
Resolving misalignment interference for NGS-based clinical diagnostics
Human Genetics (2021)
-
Hereditary brain tumor with a homozygous germline mutation in PMS2: pedigree analysis and prenatal screening in a family with constitutional mismatch repair deficiency (CMMRD) syndrome
Familial Cancer (2019)
-
Recommendations on Surveillance and Management of Biallelic Mismatch Repair Deficiency (BMMRD) Syndrome: A Consensus Statement by the US Multi-Society Task Force on Colorectal Cancer
American Journal of Gastroenterology (2017)
-
Elucidating the clinical significance of two PMS2 missense variants coexisting in a family fulfilling hereditary cancer criteria
Familial Cancer (2017)