Abstract
Background/Objectives:
Assessing fatty acid (FA) composition in relation to inflammatory markers can shed light on the role of different FA and their metabolism in low-grade inflammation. Existing exploratory studies in children are scarce, and findings inconsistent. We hence aim to analyse associations of FA with common inflammatory markers, high-sensitivity C-reactive protein (hs-CRP) and interleukin-6 (IL-6), in 10-year-old children.
Subjects/Methods:
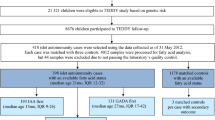
Complete data were available for 958 participants from the 10-year follow-up of the LISAplus (Influence of Lifestyle-Related Factors on the Immune System and the Development of Allergies in Childhood plus the Influence of Traffic Emissions and Genetics) birth cohort study. FA composition was assessed in serum glycerophospholipids. Hs-CRP and IL-6 were categorised into three levels. Associations of FA with inflammatory markers were assessed using multinomial logistic regression, adjusting for potential confounders. Additionally, sex-stratified analyses were carried out.
Results:
FA exposures associated with significantly higher low-grade inflammation, as indicated by higher hs-CRP or IL-6 levels, included: palmitic acid (PA) (IL-6: P<0.001, 95% confidence interval: 1.30; 2.43), arachidonic acid (AA) (hs-CRP: P=0.002, 1.07; 1.31), n-6 highly unsaturated FA (HUFA) (hs-CRP: P=0.002, 1.06; 1.27), ratio of AA to linoleic acid (AA/LA) (hs-CRP: P<0.001, 1.16; 1.62) and total saturated FA (SFA) (IL-6: P<0.001, 1.77; 3.15). FA exposures associated with reduced levels of inflammatory markers included LA (hs-CRP: P=0.001, 0.84; 0.96; IL-6: P<0.001, 0.69; 0.90) and total polyunsaturated FA (PUFA) (IL-6: P<0.001, 0.57; 0.78).
Conclusions:
These findings suggest that higher SFA and minor n-6 HUFA, namely PA and AA, are associated with increased low-grade inflammation in children, whereas the major dietary n-6 PUFA and total PUFA are associated with reduced inflammation. Elevated desaturase activity, estimated by the ratio AA/LA, may be associated with higher inflammation, particularly in boys.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Libby P . Inflammation in atherosclerosis. Arterioscler Thromb Vasc Biol 2012; 32: 2045–2051.
Libby P, Ridker PM . Inflammation and atherosclerosis: role of C-reactive protein in risk assessment. Am J Med 2004; 116: 9s–16s.
Tilg H, Moschen AR . Adipocytokines: mediators linking adipose tissue, inflammation and immunity. Nat Rev Immunol 2006; 6: 772–783.
Visser M, Bouter LM, McQuillan GM, Wener MH, Harris TB . Elevated C-reactive protein levels in overweight and obese adults. JAMA 1999; 282: 2131–2135.
Pepys MB, Hirschfield GM . C-reactive protein: a critical update. J Clin Invest 2003; 111: 1805–1812.
Jarvisalo MJ, Harmoinen A, Hakanen M, Paakkunainen U, Viikari J, Hartiala J et al. Elevated serum C-reactive protein levels and early arterial changes in healthy children. Arterioscler Thromb Vasc Biol 2002; 22: 1323–1328.
Kapiotis S, Holzer G, Schaller G, Haumer M, Widhalm H, Weghuber D et al. A proinflammatory state is detectable in obese children and is accompanied by functional and morphological vascular changes. Arterioscler Thromb Vasc Biol 2006; 26: 2541–2546.
Calder PC, Albers R, Antoine JM, Blum S, Bourdet-Sicard R, Ferns GA et al. Inflammatory disease processes and interactions with nutrition. Br J Nutr 2009; 101 (Suppl 1), S1–45.
Calder PC . Polyunsaturated fatty acids and inflammatory processes: new twists in an old tale. Biochimie 2009; 91: 791–795.
Calder PC . Omega-3 polyunsaturated fatty acids and inflammatory processes: nutrition or pharmacology? Br J Clin Pharmacol 2013; 75: 645–662.
Fekete K, Marosvölgyi T, Jakobik V, Decsi T . Methods of assessment of n-3 long-chain polyunsaturated fatty acid status in humans: a systematic review. Am J Clin Nutr 2009; 89: 2070S–2084SS.
Zeleniuch-Jacquotte A, Chajes V, Van Kappel AL, Riboli E, Toniolo P . Reliability of fatty acid composition in human serum phospholipids. Eur J Clin Nutr 2000; 54: 367–372.
Nakamura MT, Nara TY . Structure, function, and dietary regulation of Δ6, Δ5, and Δ9 desaturases. Annu Rev Nutr 2004; 24: 345–376.
Ferrucci L, Cherubini A, Bandinelli S, Bartali B, Corsi A, Lauretani F et al. Relationship of plasma polyunsaturated fatty acids to circulating inflammatory markers. J Clin Endocrinol Metab 2006; 91: 439–446.
Steffen BT, Steffen LM, Tracy R, Siscovick D, Hanson NQ, Nettleton J et al. Obesity modifies the association between plasma phospholipid polyunsaturated fatty acids and markers of inflammation: the Multi-Ethnic Study of Atherosclerosis. Int J Obes (Lond) 2012; 36: 797–804.
Kaikkonen JE, Kresanov P, Ahotupa M, Jula A, Mikkila V, Viikari JS et al. High serum n6 fatty acid proportion is associated with lowered LDL oxidation and inflammation: the Cardiovascular Risk in Young Finns Study. Free Radic Res 2014; 48: 420–426.
Muka T, Kiefte-de Jong JC, Hofman A, Dehghan A, Rivadeneira F, Franco OH . Polyunsaturated fatty acids and serum C-reactive protein: the Rotterdam study. Am J Epidemiol 2015; 181: 846–856.
Klein-Platat C, Drai J, Oujaa M, Schlienger JL, Simon C . Plasma fatty acid composition is associated with the metabolic syndrome and low-grade inflammation in overweight adolescents. Am J Clin Nutr 2005; 82: 1178–1184.
González-Gil EM, Santabárbara J, Siani A, Ahrens W, Sioen I, Eiben G et al. Whole-blood fatty acids and inflammation in European children: the IDEFICS Study. Eur J Clin Nutr 2016; 70: 819–823.
Heinrich J, Bolte G, Holscher B, Douwes J, Lehmann I, Fahlbusch B et al. Allergens and endotoxin on mothers' mattresses and total immunoglobulin E in cord blood of neonates. Eur Respir J 2002; 20: 617–623.
Glaser C, Rzehak P, Demmelmair H, Klopp N, Heinrich J, Koletzko B et al. Influence of FADS polymorphisms on tracking of serum glycerophospholipid fatty acid concentrations and percentage composition in children. PLoS One 2011; 6: e21933.
Glaser C, Demmelmair H, Sausenthaler S, Herbarth O, Heinrich J, Koletzko B . Fatty acid composition of serum glycerophospholipids in children. J Pediatr 2010; 157: 826–831. e1.
Standl M, Thiering E, Demmelmair H, Koletzko B, Heinrich J . Age-dependent effects of cord blood long-chain PUFA composition on BMI during the first 10 years of life. Br J Nutr 2014; 111: 2024–2031.
Glaser C, Demmelmair H, Koletzko B . High-throughput analysis of fatty acid composition of plasma glycerophospholipids. J Lipid Res 2010; 51: 216–221.
Lands B . Consequences of essential fatty acids. Nutrients 2012; 4: 1338–1357.
Simopoulos AP . The importance of the omega-6/omega-3 fatty acid ratio in cardiovascular disease and other chronic diseases. Exp Biol Med (Maywood) 2008; 233: 674–688.
Marventano S, Kolacz P, Castellano S, Galvano F, Buscemi S, Mistretta A et al. A review of recent evidence in human studies of n-3 and n-6 PUFA intake on cardiovascular disease, cancer, and depressive disorders: does the ratio really matter? Int J Food Sci Nutr 2015; 66: 611–622.
Harris WS, Mozaffarian D, Rimm E, Kris-Etherton P, Rudel LL, Appel LJ et al. Omega-6 fatty acids and risk for cardiovascular disease. A Science Advisory From the American Heart Association Nutrition Subcommittee of the Council on Nutrition, Physical Activity, and Metabolism; Council on Cardiovascular Nursing; and Council on Epidemiology and Prevention. Circulation 2009; 119: 902–907.
Ohnishi H, Saito Y . Eicosapentaenoic acid (EPA) reduces cardiovascular events: relationship with the EPA/arachidonic acid ratio. J Atheroscler Thromb 2013; 20: 861–877.
Cotogni P, Trombetta A, Muzio G, Maggiora M, Canuto RA . The omega-3 fatty acid docosahexaenoic acid modulates inflammatory mediator release in human alveolar cells exposed to bronchoalveolar lavage fluid of ARDS patients. Biomed Res Int 2015; 2015: 642520.
Martinelli N, Girelli D, Malerba G, Guarini P, Illig T, Trabetti E et al. FADS genotypes and desaturase activity estimated by the ratio of arachidonic acid to linoleic acid are associated with inflammation and coronary artery disease. Am J Clin Nutr 2008; 88: 941–949.
Vessby B, Gustafsson IB, Tengblad S, Boberg M, Andersson A . Desaturation and elongation of fatty acids and insulin action. Ann NY Acad Sci 2002; 967: 183–195.
R Core Team. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing. Vienna, Austria, 2016.
Venables WN, Ripley BD . Modern Applied Statistics with S, 4th edn. Springer: New York, NY, USA, 2002.
Shine B, de Beer FC, Pepys MB . Solid phase radioimmunoassays for human C-reactive protein. Clin Chim Acta 1981; 117: 13–23.
Kleiner G, Marcuzzi A, Zanin V, Monasta L, Zauli G . Cytokine levels in the serum of healthy subjects. Mediat Inflamm 2013; 2013: 6.
Vittinghoff E, McCulloch CE . Relaxing the rule of ten events per variable in logistic and Cox regression. Am J Epidemiol 2007; 165: 710–718.
Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR . A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol 1996; 49: 1373–1379.
Black S, Kushner I, Samols D . C-reactive protein. J Biol Chem 2004; 279: 48487–48490.
Castell JV, Gómez-Lechón MJ, David M, Andus T, Geiger T, Trullenque R et al. Interleukin-6 is the major regulator of acute phase protein synthesis in adult human hepatocytes. FEBS Lett 1989; 242: 237–239.
Bode JG, Albrecht U, Häussinger D, Heinrich PC, Schaper F . Hepatic acute phase proteins—regulation by IL-6-and IL-1-type cytokines involving STAT3 and its crosstalk with NF-κB-dependent signaling. Eur J Cell Biol 2012; 91: 496–505.
Ganter U, Arcone R, Toniatti C, Morrone G, Ciliberto G . Dual control of C-reactive protein gene expression by interleukin-1 and interleukin-6. EMBO J 1989; 8: 3773–3779.
Ford ES . C-reactive protein concentration and cardiovascular disease risk factors in children: findings from the National Health and Nutrition Examination Survey 1999–2000. Circulation 2003; 108: 1053–1058.
Decsi T, Kennedy K . Sex-specific differences in essential fatty acid metabolism. Am J Clin Nutr 2011; 94 (Suppl), 1914S–1919SS.
Burdge GC, Wootton SA . Conversion of alpha-linolenic acid to eicosapentaenoic, docosapentaenoic and docosahexaenoic acids in young women. Br J Nutr 2002; 88: 411–420.
James MJ, Gibson RA, Cleland LG . Dietary polyunsaturated fatty acids and inflammatory mediator production. Am J Clin Nutr 2000; 71 (Suppl), 343s–348s.
King DE, Egan BM, Geesey ME . Relation of dietary fat and fiber to elevation of C-reactive protein. Am J Cardiol 2003; 92: 1335–1339.
Weigert C, Brodbeck K, Staiger H, Kausch C, Machicao F, Haring HU et al. Palmitate, but not unsaturated fatty acids, induces the expression of interleukin-6 in human myotubes through proteasome-dependent activation of nuclear factor-kappaB. J Biol Chem 2004; 279: 23942–23952.
Ajuwon KM, Spurlock ME . Palmitate activates the NF-κB transcription factor and induces IL-6 and TNFα expression in 3T3-L1 adipocytes. J Nutr 2005; 135: 1841–1846.
Enzenbach C, Kroger J, Zietemann V, Jansen EH, Fritsche A, Doring F et al. Erythrocyte membrane phospholipid polyunsaturated fatty acids are related to plasma C-reactive protein and adiponectin in middle-aged German women and men. Eur J Nutr 2011; 50: 625–636.
De Caterina R, Liao JK, Libby P . Fatty acid modulation of endothelial activation. Am J Clin Nutr 2000; 71 (Suppl), 213s–223ss.
Lands B . Historical perspectives on the impact of n-3 and n-6 nutrients on health. Prog Lipid Res 2014; 55: 17–29.
Johnson GH, Fritsche K . Effect of dietary linoleic acid on markers of inflammation in healthy persons: a systematic review of randomized controlled trials. J Acad Nutr Diet 2012; 112: 1029–1041, 41.e1–41.e15.
Mohrhauer H, Holman RT . The effect of dose level of essential fatty acids upon fatty acid composition of the rat liver. J Lipid Res 1963; 4: 151–159.
Rett BS, Whelan J . Increasing dietary linoleic acid does not increase tissue arachidonic acid content in adults consuming Western-type diets: a systematic review. Nutr Metab (Lond) 2011; 8: 36.
Bjermo H, Iggman D, Kullberg J, Dahlman I, Johansson L, Persson L et al. Effects of n-6 PUFAs compared with SFAs on liver fat, lipoproteins, and inflammation in abdominal obesity: a randomized controlled trial. Am J Clin Nutr 2012; 95: 1003–1012.
Liou YA, King DJ, Zibrik D, Innis SM . Decreasing linoleic acid with constant alpha-linolenic acid in dietary fats increases (n-3) eicosapentaenoic acid in plasma phospholipids in healthy men. J Nutr 2007; 137: 945–952.
Brenna JT . Efficiency of conversion of alpha-linolenic acid to long chain n-3 fatty acids in man. Curr Opin Clin Nutr Metab Care 2002; 5: 127–132.
FAOFats and fatty acids in human nutrition. Report of an expert consultation. FAO food and nutrition paper no. 19, 2010, pp 1–166.
Riboli E, Ronnholm H, Saracci R . Biological markers of diet. Cancer Surv 1987; 6: 685–718.
Rise P, Eligini S, Ghezzi S, Colli S, Galli C . Fatty acid composition of plasma, blood cells and whole blood: relevance for the assessment of the fatty acid status in humans. Prostaglandins Leukot Essent Fatty Acids 2007; 76: 363–369.
Sergeant S, Ruczinski I, Ivester P, Lee TC, Morgan TM, Nicklas BJ et al. Impact of methods used to express levels of circulating fatty acids on the degree and direction of associations with blood lipids in humans. Br J Nutr 2016; 115: 251–261.
Schaeffer L, Gohlke H, Muller M, Heid IM, Palmer LJ, Kompauer I et al. Common genetic variants of the FADS1 FADS2 gene cluster and their reconstructed haplotypes are associated with the fatty acid composition in phospholipids. Hum Mol Genet 2006; 15: 1745–1756.
Steffen LM, Vessby B, Jacobs DR Jr, Steinberger J, Moran A, Hong CP et al. Serum phospholipid and cholesteryl ester fatty acids and estimated desaturase activities are related to overweight and cardiovascular risk factors in adolescents. Int J Obes (Lond) 2008; 32: 1297–1304.
Acknowledgements
We thank all the families for their participation in the LISAplus studies. Furthermore, we thank all members of the LISAplus study groups for their excellent work.The LISAplus study was mainly supported by grants from the Federal Ministry for Education, Science, Research and Technology and in addition from Helmholtz Zentrum Munich (former GSF), Helmholtz Centre for Environmental Research—UFZ, Leipzig, Research Institute at Marien-Hospital Wesel, Paediatric Practice, Bad Honnef for the first 2 years. The 4-, 6- and 10-year follow-up examinations of the LISAplus study were covered from the respective budgets of the involved partners (Helmholtz Zentrum Munich (former GSF), Helmholtz Centre for Environmental Research—UFZ, Leipzig, Research Institute at Marien-Hospital Wesel, Paediatric Practice, Bad Honnef, IUF—Leibniz-Research Institute for Environmental Medicine at the University of Düsseldorf) and in addition by a grant from the Federal Ministry for Environment (IUF Düsseldorf, FKZ 20462296). The work of BK is financially supported in part by the European Research Council Advanced Grant META-GROWTH (ERC-2012-AdG—no.322605).
Author contributions
CH, JH and MS were involved in the conception and design of the study; BK, HD, IL, AvB and JH in the data acquisition; CH, MS and CF in the statistical analyses; CH, MS, HD and JH in the interpretation; CH drafted the manuscript; all authors revised it critically for important intellectual content, and approved the final version to be published.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on European Journal of Clinical Nutrition website
Supplementary information
Rights and permissions
About this article
Cite this article
Harris, C., Demmelmair, H., von Berg, A. et al. Associations between fatty acids and low-grade inflammation in children from the LISAplus birth cohort study. Eur J Clin Nutr 71, 1303–1311 (2017). https://doi.org/10.1038/ejcn.2017.73
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2017.73
This article is cited by
-
Dietary saturated fat and low-grade inflammation modified by accelerometer-measured physical activity in adolescence: results from the GINIplus and LISA birth cohorts
BMC Public Health (2019)
-
FADS1 genotype is distinguished by human subcutaneous adipose tissue fatty acids, but not inflammatory gene expression
International Journal of Obesity (2019)