Abstract
Background/Objectives:
To evaluate the association between the carbohydrate quality index (CQI) and weight change or incident overweight/obesity (body mass index ⩾25 kg/m2) in the ‘Seguimiento Universidad de Navarra (SUN)’ cohort.
Subjects/Methods:
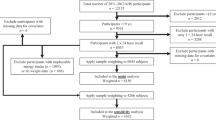
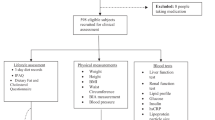
A total of 8741 participants who were initially free of overweight/obesity were followed up for a median of 7.9 years. We evaluated at baseline the CQI according to four criteria: dietary fiber intake, glycemic index, whole grains/total grains ratio and solid carbohydrates/total carbohydrates ratio. Subjects were classified into quintiles according to CQI. Weight was recorded at baseline and updated every 2 years during follow-up.
Results:
Increasing CQI of diet was not significantly associated with lower weight gain, although participants in the highest quintile had the lowest average crude weight gain (+211 g/year). We observed 1862 incident cases of overweight/obesity during follow-up. CQI was significantly associated (P for trend 0.006) with a lower risk of overweight/obesity; adjusted odds ratio for the fourth and fifth quintiles were 0.81 (95% confidence interval (CI): 0.66–0.99) and 0.74 (95% CI: 0.60–0.92), respectively.
Conclusions:
In this Mediterranean cohort, CQI showed a significant inverse association with the incidence of overweight/obesity, which highlights that carbohydrate intake guidelines related to obesity prevention should be focused on improving the CQI of the diet.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Kelly T, Yang W, Chen CS, Reynolds K, He J . Global burden of obesity in 2005 and projections to 2030. Int J Obes (Lond) 2008; 32: 1431–1437.
Hu FB . Obesity epidemiology. Oxford University Press: Oxford; New York, 2008.
Hutfless S, Gudzune KA, Maruthur N, Wilson RF, Bleich SN, Lau BD et al. Strategies to prevent weight gain in adults: a systematic review. Am J Prev Med 2013; 45: e41–e51.
Thomas DE, Elliott EJ, Baur L . Low glycaemic index or low glycaemic load diets for overweight and obesity. Cochrane Database Syst Rev 2007; 18: CD005105.
Aller EE, Abete I, Astrup A, Martinez JA, van Baak MA . Starches, sugars and obesity. Nutrients 2011; 3: 341–369.
Wycherley TP, Moran LJ, Clifton PM, Noakes M, Brinkworth GD . Effects of energy-restricted high-protein, low-fat compared with standard-protein, low-fat diets: a meta-analysis of randomized controlled trials. Am J Clin Nutr 2012; 96: 1281–1298.
Summerbell CD, Cameron C, Glasziou PP . WITHDRAWN: Advice on low-fat diets for obesity. Cochrane Database Syst Rev 2008; 3: CD003640.
Hooper L, Abdelhamid A, Moore HJ, Douthwaite W, Skeaff CM, Summerbell CD . Effect of reducing total fat intake on body weight: systematic review and meta-analysis of randomised controlled trials and cohort studies. BMJ 2012; 345: e7666.
Fogelholm M, Anderssen S, Gunnarsdottir I, Lahti-Koski M . Dietary macronutrients and food consumption as determinants of long-term weight change in adult populations: a systematic literature review. Food Nutr Res 2012; 56: 19103.
Joint FAO/WHO Expert Consultation. WHO technical report series 916: Diet, nutrition and the prevention of chronic diseases. World Health Organization: Geneva, Switzerland, 2003.
van Dam RM, Seidell JC . Carbohydrate intake and obesity. Eur J Clin Nutr 2007; 61 (Suppl 1): S75–S99.
Merchant AT, Vatanparast H, Barlas S, Dehghan M, Shah SM, De Koning L et al. Carbohydrate intake and overweight and obesity among healthy adults. J Am Diet Assoc 2009; 109: 1165–1172.
Roberts CK, Liu S . Carbohydrate intake and obesity: an association that needs "refining". J Am Diet Assoc 2009; 109: 1163–1164.
DiMeglio DP, Mattes RD . Liquid versus solid carbohydrate: effects on food intake and body weight. Int J Obes Relat Metab Disord 2000; 24: 794–800.
Overby NC, Sonestedt E, Laaksonen DE, Birgisdottir BE . Dietary fiber and the glycemic index: a background paper for the Nordic Nutrition Recommendations 2012. Food Nutr Res 2013; 57: 20709.
Martinez-Gonzalez MA, Sanchez-Villegas A, De Irala J, Marti A, Martinez JA . Mediterranean diet and stroke: objectives and design of the SUN project. Seguimiento Universidad de Navarra. Nutr Neurosci 2002; 5: 65–73.
Segui-Gomez M, de la Fuente C, Vazquez Z, de Irala J, Martinez-Gonzalez MA . Cohort profile: the 'Seguimiento Universidad de Navarra' (SUN) study. Int J Epidemiol 2006; 35: 1417–1422.
Willet W . Issues in analysis and presentation of dietary data. In: Nutritional Epidemiology, 2nd ed. Oxford University Press: New York, NY, 1998, p 322.
Martin-Moreno JM, Boyle P, Gorgojo L, Maisonneuve P, Fernandez-Rodriguez JC, Salvini S et al. Development and validation of a food frequency questionnaire in Spain. Int J Epidemiol 1993; 22: 512–519.
de la Fuente-Arrillaga C, Ruiz ZV, Bes-Rastrollo M, Sampson L, Martinez-Gonzalez MA . Reproducibility of an FFQ validated in Spain. Public Health Nutr 2010; 13: 1364–1372.
Fernandez-Ballart JD, Pinol JL, Zazpe I, Corella D, Carrasco P, Toledo E et al. Relative validity of a semi-quantitative food-frequency questionnaire in an elderly Mediterranean population of Spain. Br J Nutr 2010; 103: 1808–1816.
Moreiras O, Carbajal A, Cabrera L Tablas de composición de alimentos. 9ª ed. Ediciones Pirámide (Grupo Anaya, SA): Madrid, 2005.
Zazpe I, Sánchez-Taínta A, Santiago S, de la Fuente-Arrillaga C, Bes-Rastrollo M, Martínez JA et al. Quality of dietary carbohydrate intake and micronutrient adequacy in a Mediterranean cohort: the SUN (Seguimiento Universidad de Navarra) project. Br J Nutr. e-pub ahead of print 25 March 2014.
Bes-Rastrollo M . Validation of self-reported weight and body mass index in a cohort of university graduates in Spain. Rev Esp Obes 3: 352–358 2005.
Martinez-Gonzalez MA, Lopez-Fontana C, Varo JJ, Sanchez-Villegas A, Martinez JA . Validation of the Spanish version of the physical activity questionnaire used in the nurses' health study and the health professionals' follow-up study. Public Health Nutr 2005; 8: 920–927.
Hauner H, Bechthold A, Boeing H, Bronstrup A, Buyken A, Leschik-Bonnet E et al. Evidence-based guideline of the German Nutrition Society: carbohydrate intake and prevention of nutrition-related diseases. Ann Nutr Metab 2012; 60 (Suppl 1): 1–58.
Iqbal SI, Helge JW, Heitmann BL . Do energy density and dietary fiber influence subsequent 5-year weight changes in adult men and women? Obesity (Silver Spring) 2006; 14: 106–114.
Ludwig DS, Pereira MA, Kroenke CH, Hilner JE, Van Horn L, Slattery ML et al. Dietary fiber, weight gain, and cardiovascular disease risk factors in young adults. JAMA 1999; 282: 1539–1546.
Hu FB . Resolved: there is sufficient scientific evidence that decreasing sugar-sweetened beverage consumption will reduce the prevalence of obesity and obesity-related diseases. Obes Rev 2013; 14: 606–619.
Yancy WS, Wang CC, Maciejewski ML . Trends in energy and macronutrient intakes by weight status over four decades. Public Health Nutr 2013; 16: 1–10.
Varela-Moreiras G, Ruiz E, Valero T, Avila JM, del Pozo S . The Spanish diet: an update. Nutr Hosp 2013; 28 (Suppl 5): 13–20.
National Health Survey 2011-2012. Ministry of Health, Social Services and Equality, National Statistics Institute [WWW document] URL: http://www.msssi.gob.es/estadEstudios/estadisticas/encuestaNacional/encuestaNac2011/PresentacionENSE2012.pdf.
Wolever TM . Is glycaemic index (GI) a valid measure of carbohydrate quality? Eur J Clin Nutr 2013; 67: 522–531.
Schwingshackl L, Hoffmann G . Long-term effects of low glycemic index/load vs. high glycemic index/load diets on parameters of obesity and obesity-associated risks: a systematic review and meta-analysis. Nutr Metab Cardiovasc Dis 2013; 23: 699–706.
Malik VS, Popkin BM, Bray GA, Despres JP, Willett WC, Hu FB . Sugar-sweetened beverages and risk of metabolic syndrome and type 2 diabetes: a meta-analysis. Diabetes Care 2010; 33: 2477–2483.
Du H, van der AD, Boshuizen HC, Forouhi NG, Wareham NJ, Halkjaer J et al. Dietary fiber and subsequent changes in body weight and waist circumference in European men and women. Am J Clin Nutr 2010; 91: 329–336.
Mozaffarian D, Hao T, Rimm EB, Willett WC, Hu FB . Changes in diet and lifestyle and long-term weight gain in women and men. N Engl J Med 2011; 364: 2392–2404.
Cho SS, Qi L, Fahey Jr GC, Klurfeld DM . Consumption of cereal fiber, mixtures of whole grains and bran, and whole grains and risk reduction in type 2 diabetes, obesity, and cardiovascular disease. Am J Clin Nutr 2013; 98: 594–619.
Slavin J . Fiber and prebiotics: mechanisms and health benefits. Nutrients 2013; 5: 1417–1435.
Williams PG . Evaluation of the evidence between consumption of refined grains and health outcomes. Nutr Rev 2012; 70: 80–99.
Acknowledgements
The authors thank the enthusiastic collaboration and participation of the SUN cohort participants. We also thank the other members of the SUN study Group: Alonso A, Barrio López MT, Basterra-Gortari FJ, Beunza JJ, Carlos Chillerón S, Carmona L, de Irala J, De la Rosa PA, Delgado-Rodriguez M, Donat Vargas CL, Fernández Montero A, Galbete Ciáurriz C, García López M, Gea Sánchez A, Goñi Ochandorena E, Guillen-Grima F, Hernández A, Lahortiga F, Llorca J, Lopez del Burgo C, Marí Sanchís A, Martí del Moral A, Martín Calvo N, Martínez JA, Nuñez-Cordoba JM, Pimenta A, Ruiz Canela M, Ruiz Zambrana A, Sanchez Adán D, Sanchez-Villegas A, Toledo Atucha E, Toledo Atucha J and Vázquez Ruiz Z. We are also grateful to the members of the Department of Nutrition of Harvard School of Public Health (A Ascherio, W Willett and FB Hu), who helped us design the SUN study. The SUN study has received funding from the Instituto de Salud Carlos III, Official Agency of the Spanish Government for biomedical research (Grants PI1002293, PI1002658, RD06/0045, G03/140 and PI13/00615), the Ministerio de Sanidad, Política Social e Igualdad through the Plan Nacional de Drogas (2010/087), the Navarra Regional Government (45/2011) and the University of Navarra.
Author Contributions
The authors’ responsibilities were as follows: IZ, SS and MAM designed research; IZ, SS and MAM conducted the research; CSO, SB, CFA, MBR and MAM provided essential materials; IZ, SS, CSO, MBR and MAM analyzed data or performed statistical analysis; and SS and IZ had primary responsibility for the final content. All authors revised and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Disclaimer
The funding sources had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; and preparation, review or approval of the manuscript.
Rights and permissions
About this article
Cite this article
Santiago, S., Zazpe, I., Bes-Rastrollo, M. et al. Carbohydrate quality, weight change and incident obesity in a Mediterranean cohort: the SUN Project. Eur J Clin Nutr 69, 297–302 (2015). https://doi.org/10.1038/ejcn.2014.187
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2014.187
This article is cited by
-
Association between quality and quantity of carbohydrate intake with selected anthropometric indices among primary school girls in Kerman city, Iran: a cross-sectional study
BMC Pediatrics (2024)
-
How do carbohydrate quality indices influence on bone mass density in postmenopausal women? A case–control study
BMC Women's Health (2023)
-
Dietary carbohydrate quality index (CQI), cardio-metabolic risk factors and insulin resistance among adults with obesity
BMC Endocrine Disorders (2023)
-
Preoperative Carbohydrate Quality Index Is Related to Markers of Glucose Metabolism 12 Months After Roux-en-Y Gastric Bypass
Obesity Surgery (2023)
-
Relationship between dietary carbohydrate quality index and metabolic syndrome among type 2 diabetes mellitus subjects: a case-control study from Ghana
BMC Public Health (2021)