Abstract
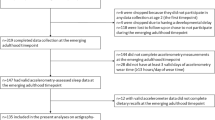
We examined satiety quotient (SQ) and energy intake (EI) according to sleep duration, quality and timing. Seventy-five overweight/obese men (age: 41.1±5.8 years; body mass index: 33.6±2.9 kg/m2) completed visual analogue scales for appetite sensations before, immediately after and every 10 minutes for 1 hour following a standardized breakfast. The mean SQ (primary outcome of the study) was calculated from four appetite sensations. The Pittsburgh Sleep Quality Index identified short-duration (<7 h/night) and ‘recommended sleep duration’ (⩾7 h/night) sleepers, poor (score ⩾5)- and good (score <5)-quality sleepers and late (midpoint of sleep >0230 hours) and early (midpoint of sleep ⩽0230 hours) sleepers. A 3-day food record and buffet-style meal assessed the EI. Short-duration sleepers had a lower mean SQ compared with recommended sleep duration sleepers (6.5±4.9 vs 8.8±4.3 mm/100 kcal; P=0.04). The mean SQ between poor and good (6.9±4.6 vs 8.7±4.6 mm/100 kcal; P=0.11) and that between early and late (8.99±5.10 vs 9.32±4.02 mm/100 kcal; P=0.78) sleepers were not significantly different. EI did not differ between the sleep groups. Thus, short-duration sleepers had a lower mean SQ compared with recommended sleep duration sleepers. However, this did not coincide with an increased EI.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Siervo M, Wells JC, Cizza G . The contribution of psychosocial stress to the obesity epidemic: an evolutionary approach. Horm Metab Res 2009; 41: 261–270.
Green SM, Delargy HJ, Joanes D, Blundell JE . A satiety quotient: a formulation to assess the satiating effect of food. Appetite 1997; 29: 291–304.
Drapeau V, King N, Hetherington M, Doucet E, Blundell J, Tremblay A . Appetite sensations and satiety quotient: predictors of energy intake and weight loss. Appetite 2007; 48: 159–166.
Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ . The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 1989; 28: 193–213.
Adamo KB, Wilson S, Belanger K, Chaput J-P . Later bedtime is associated with greater daily energy intake and screen time in obese adolescents independent of sleep duration. J Sleep Disorders Ther 2003; 2: 1–5.
Doucet E, St-Pierre S, Almeras N, Tremblay A . Relation between appetite ratings before and after a standard meal and estimates of daily energy intake in obese and reduced obese individuals. Appetite 2003; 40: 137–143.
St-Onge MP, Roberts AL, Chen J, Kelleman M, O’Keeffe M, RoyChoudhury A et al. Short sleep duration increases energy intakes but does not change energy expenditure in normal-weight individuals. Am J Clin Nutr 2011; 94: 410–416.
Brondel L, Romer MA, Nougues PM, Touyarou P, Davenne D . Acute partial sleep deprivation increases food intake in healthy men. Am J Clin Nutr 2010; 91: 1550–1559.
Baron KG, Reid KJ, Kern AS, Zee PC . Role of sleep timing in caloric intake and BMI. Obesity (Silver Spring) 2011; 19: 1374–1381.
Shechter A, O’Keeffe M, Roberts AL, Zammit GK, RoyChoudhury A, St-Onge MP . Alterations in sleep architecture in response to experimental sleep curtailment are associated with signs of positive energy balance. Am J Physiol Regul Integr Comp Physiol 2012; 303: R883–R889.
Gonnissen HK, Hursel R, Rutters F, Martens EA, Westerterp-Plantenga MS . Effects of sleep fragmentation on appetite and related hormone concentrations over 24 h in healthy men. Br J Nutr 2013; 109: 748–756.
Acknowledgements
VD and AT conceived and carried out the experiment. JM, JPC, VD and ARG analysed the data. All authors were involved in writing the paper and had final approval of the submitted and published versions. This study was partly funded by the Canadian Institutes of Health Research. ARG is funded by the Quebec Heart and Lung Research Institute. JPC holds a Junior Research Chair in Healthy Active Living and Obesity Research. AT holds a Canada Research Chair in Environment and Energy Balance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Appendix
Appendix

Rights and permissions
About this article
Cite this article
McNeil, J., Drapeau, V., Gallant, A. et al. Short sleep duration is associated with a lower mean satiety quotient in overweight and obese men. Eur J Clin Nutr 67, 1328–1330 (2013). https://doi.org/10.1038/ejcn.2013.204
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2013.204