Abstract
Background/Objectives:
Few studies have used healthy eating index (HEI) and mediterranean diet adherence (MDA) scores to evaluate the diet quality during pregnancy. To determine the relationship between first trimester diet quality and insulin sensitivity/resistance biomarkers at birth.
Subjects/Methods:
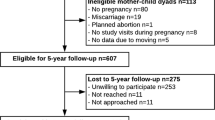
Cord-blood insulin sensitivity/resistance biomarkers of the offspring of 35 women whose diets were ‘adequate’ or ‘inadequate’ according to their HEI score (>70 or ⩽70, respectively) and their 13-point MDA score (⩾7 or <7, respectively).
Results:
Low HEI-score diets contained less (g/1000 kcal) carbohydrates (CHO; P=0.027) and fibre (P=0.011), and more fats (P<0.001) and cholesterol (P<0.001), and contributed (percentage contribution to total energy (%En)) fewer CHO (P=0.005), more fats (P=<0.001) and saturated fatty acid (SFA; P=0.002) than their high HEI-score counterparts. Low MDA-score diets contained less (g/1000 kcal) fibre (P<0.001) and more cholesterol (P=0.05), had lower polyunsaturated fatty acids+monounsaturated fatty acid/SFA (PUFA+MUFA/SFA; P=0.05) and higher SFA/CHO (P=0.021) and ω-6/ω-3 PUFA ratios (P=0.044) than their respective counterparts. Women consuming the low HEI- or low MDA-score diets had low-fasting glycaemia (P=0.016 or P=0.025, respectively) but delivered infants with high insulinaemia (P=0.048 or P=0.017, respectively), homeostatic model assessment for insulin resistance (HOMA-IR; P=0.031 or P=0.049, respectively) and glycaemia (P=0.018 or P=0.048, respectively). The relative risk (RR) of high-neonatal glycaemia and insulinaemia were 7.6 (P=0.008) and 6.7 (P=0.017) for low vs high HEI-score groups. High HOMA-IR and high glucose RR were, respectively, 3.4 (P=0.043) and 3.9 (P=0.016) in neonates from the <7 MDA- vs ⩾7 MDA-score group. These RRs were not affected by potential confounders.
Conclusion:
Maternal diets with low HEI- or MDA-scores during the first trimester of pregnancy negatively affect insulin resistance markers at birth.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Rifas-Shiman SL, Rich-Edwards JW, Kleinman KP, Oken E, Gillman MW . Dietary quality during pregnancy varies by maternal characteristics in Project Viva: a US cohort. J Am Diet Assoc 2009; 109: 1004–1011.
Tsigga M, Filis V, Hatzopoulou K, Kotzamanidis C, Grammatikopoulou MG . Healthy eating index during pregnancy according to pre-gravid and gravid weight status. Public Health Nutr 2011; 14: 290–296.
Rifas-Shiman SL, Richard-Edwards JW, Willet WC, Kleinman KP, Oken E, Gillman MW . Changes in dietary intake from the first to the second trimester of pregnancy. Pediatr Perinat Epidemiol 2006; 20: 35–42.
Crozier SR, Robinson SM, Godfrey KM, Cooper C, Inskip HM . Women’s dietary patterns change little from before to during pregnancy. J Nutr 2009; 139: 1956–1963.
Burger KNJ, Beulens JWJ, Boer JMA, Spijkerman AMW, van der A DL . Dietary glycemic load and glycemic index and risk of coronary heart disease and stroke in Dutch men and women: The EPIC-MORGEN Study. PLoS One 2011; 6: e25955.
Nillsson AC, Ostman WM, Knudsen KE, Holst JJ, Riörch IM . A cereal-based evening meal rich in indigestible carbohydrates increases plasma butyrate the next morning. J Nutr 2010; 140: 1932–1936.
Martín de Santa Olalla L, Sánchez-Muniz FJ, Vaquero MP . N-3 fatty acids in glucose metabolism and insulin sensitivity. Nutr Hosp 2009; 24: 113–127.
Vessby B, Uusitupa M, Hermansen K, Riccardi G, Rivellese AA, Tapsell LC et al. Substituting dietary saturated for monounsaturated fat impairs insulin sensitivity in healthy men and women: the KANWU study. Diabetologia 2001; 44: 312–319.
Vessby B, Gustafsson IB, Boberg J, Karlström B, Lithell H, Werner I . Substituting polyunsaturated for saturated fat as a single change in a Swedish diet: effects on serum lipoprotein metabolism and glucose tolerance in patients with hyperlipoproteinaemia. Eur J Clin Invest 1980; 10: 193–202.
Jeppesen J, Hansen TW, Rasmussen S, Ibsen H, Torp-Pedersen C, Madsbad S . Insulin resistance, the metabolic syndrome, and risk of incident cardiovascular disease. A population-based study. J Am Coll Cardiol 2007; 49: 2112–2119.
Lemos JO, Rondo PHC, Pereira JA, Oliveira RG, Freire MBS, Sonsin PB . The relationship between birth weight and insulin resistance in childhood. Br J Nutr 2010; 103: 386–392.
Mericq V, Ong KK, Bazaes R, Peña V, Avila A, Salazar T et al. Longitudinal changes in insulin sensitivity and secretion from birth to age three years in small- and appropriate-for-gestational-age children. Diabetologia 2005; 48: 2609–2614.
Gesteiro E, Bastida S, Sánchez-Muniz FJ . Insulin resistance markers in term, normoweight neonates. The Merida cohort. Eur J Pediatr 2009; 168: 281–288.
Smith CE, Arnett DK, Corella D, Tsai MY, Lai CQ, Parnell LD et al. Perilipin polymorphism interacts with saturated fat and carbohydrates to modulate insulin resistance. Nutr Metab Cardiovasc Dis 2012; 22: 449–455.
Cabello-Saavedra E, Bes-Rastrollo M, Martinez JA, Diez-Espino J, Buil-Cosiales P, Serrano-Martinez M et al. Macronutrient intake and metabolic syndrome in subjects at high cardiovascular risk. Ann Nutr Metab 2010; 56: 152–159.
Kastorini C-M, Milionis HJ, Esposito K, Giugliano D, Goudevenos JA, Panagiotakos DB . The effect of mediterranean diet on metabolic syndrome and its components. J Am Coll Cardiol 2011; 57: 1299–1313.
Koning L de, Chiuve SE, Fung TT, Willett WC, Rimm EB, Hu FB . Diet-quality scores and the risk of type 2 diabetes in men. Diabetes Care 2011; 34: 1150–1156.
Kennedy ET, Ohls J, Carlson S, Fleming K . The healthy eating index: design and applications. J Am Diet Assoc 1995; 95: 1103–1108.
Mc Cullough ML, Feskanich D, Stampfer MJ, Giovannucci EL, Rimm EB, Hu FB et al. Diet quality and major chronic disease risk in men and women: moving toward improved dietary guidance. Am J Clin Nutr 2002; 76: 1261–1271.
Bodnar LM, Siega-Riz AM . A diet quality index for pregnancy detects variation in diet and difference by sociodemographic factors. Public Health Nutr 2002; 5: 801–809.
Hahn CS, Rock CL, King I, Drewnowski A . Validation of the healthy eating index with use of plasma biomarkers in a clinical sample of women. Am J Clin Nutr 2001; 74: 479–489.
Weinstein SJ, Vogt TM, Gerrior SA . Healthy eating index scores are associated with blood nutrient concentrations in the third National Health and Nutrition Examination Survey. J Am Diet Assoc 2004; 104: 576–584.
Trichopoulou A, Costacou T, Bamia C, Trichopoulos D . Adherence to a mediterranean diet and survival in a Greek population. N Engl J Med 2003; 348: 2599–2608.
Estruch R, Martínez-González MA, Corella D, Salas-Salvadó J, Ruiz-Gutiérrez V, Covas MI et alPREDIMED Study Investigators Effects of a mediterranean-style diet on cardiovascular risk factors: a randomized trial. Ann Intern Med 2006; 145: 1–11.
Salas-Salvado J, Fernandez-Ballart J, Ros E, Martinez-Gonzalez M-A, Fito M, Estruch R et alPREDIMED Study Investigators Effect of a mediterranean diet supplemented with nuts on metabolic syndrome status. One-year results of the PREDIMED randomized trial. Arch Intern Med 2008; 168: 2449–2458.
O’Sullivan BA, Henderson ST, Davis JM . Gestational diabetes. J Am Pharm Assoc (Wash) 1998; 38: 364–371., quiz 372-373.
Serra Majem L, Aranceta Bartrina J . Alimentación infantil y juvenil. Estudio enKid. Ed, Masson: Barcelona, 2002.
Mataix Verdú J, Llopis González J Jiménez Contreras JF, Lendoiro Otero RM, Meniño Olivera MJ (eds).. Manual gráfico e contenido nutricional de pratos galegos. Graphic Manual and Nutritional Content of Galicia Dishes. Consellería de Sanidad, Carrefour: Galicia, Spain, 1993.
Ortega RM, López-Sobaler AM, Andrés P, Requejo AM, Aparicio A, Molinero LM . DIAL software for assessing diets and food calculations. Departamento de Nutrición (UCM) and Alce Ingeniería SA Madrid 2004: http://www.alceingenieria.net/nutricion.htm. (accessed April 2011).
Requejo AM, Ortega RM El rombo de la alimentación. Ministerio de Sanidad y Consumo: Madrid, 1996.
Sociedad Española de Nutrición Comunitaria Guía de la alimentación saludable. SENC: Madrid, 2004.
Norte Navarro AI, Ortiz Moncada R . Spanish diet quality according to the healthy eating index. Nutr Hosp 2011; 26: 330–336.
Schröder H, Vila J, Marrugat J, Covas MI . Low energy density diets are associated with favorable nutrient intake profile and adequacy in free-living elderly men and women. J Nutr 2008; 138: 1476–1481.
Katz A, Nambi SS, Mather K, Baron AD, Follmann DA, Sullivan G et al. Quantitative insulin sensitivity check index: a simple, accurate method for assessing insulin sensitivity in humans. J Clin Endocrinol Metab 2000; 85: 2402–2410.
Livesey G . A systematic review of the glycaemic response to foods and health. ILSI Europe workshop. Glycaemic response on health: Nice, France, 2006 pp 82–127.
Serra Majem L, Ribas Barba L, Aranceta Bartrina J, Pérez Rodrigo C, Saavedra Santana P, Peña Quintana L . Obesidad infantil y juvenil en España. Resultados del Estudio enKid (1998-2000). Med Clin. Barc, 2003; 121: 725–732.
Spanish National Nutrition Survey (Encuesta Española de Ingesta Dietética). http://www.aesan.msc.es/AESAN/docs/docs/notas_prensa/Presentacion_ENIDE.pdf (accessed April 2011).
FAO/WHO The Joint FAO/WHO expert consultation on fats and fatty acids in human nutrition. FAO food and nutrition paper 91. Food and Agriculture Organization of the United Nations: Rome, 2010 ISSN 0254-4725.
Maedler K, Oberholzer J, Bucher P, Spinas GA, Donath MY . Monounsaturated fatty acids prevent the deleterious effects of palmitate and high glucose on human pancreatic beta-cell turnover and function. Diabetes 2003; 52: 726–733.
Roche HM . Fatty acids and the metabolic syndrome. Proc Nutr Soc 2005; 64: 23–29.
Meyer KA, Kushi LH, Jacobs DR, Folsom AR . Dietary fat and incidence of type 2 diabetes in older Iowa women. Diabetes Care 2001; 24: 1528–1535.
Salmeron J, Hu FB, Manson JE, Stampfer MJ, Colditz GA, Rimm EB et al. Dietary fat intake and risk of type 2 diabetes in women. Am J Clin Nutr 2001; 73: 1019–1026.
Panagiotakos DB, Tzima N, Pitsavos C, Chrysohoou C, Zampelas A, Toussoulis D et al. The association between adherence to the mediterranean diet and fasting indices of glucose homeostasis: the ATTICA study. J Am Coll Nutr 2007; 26: 32–38.
Holness MJ, Smith ND, Greenwood GK, Sugden MC . Acute ω-3 fatty acid enrichment selectively reverses high-saturated fat feeding-induced insulin hypersecretion but does not improve peripheral insulin resistance. Diabetes 2004; 53 (Suppl): S166–S171.
Mayer-Davis EJ, Monaco JH, Hoen HM, Carmichael S, Vitolins MZ, Rewers MJ et al. Dietary fat and insulin sensitivity in a triethnic population: the role of obesity. The insulin resistance atherosclerosis study (IRAS). Am J Clin Nutr 1997; 65: 79–87.
López S, Bermúdez B, Pacheco YM, Villar J, Abia R, Muriana FJG . Distinctive postprandial modulation of β-cell function and insulin sensitivity by dietary fats: monounsaturated compared with saturated fatty acids. Am J Clin Nutr 2008; 88: 638–644.
Pérez-Jiménez F, López Miranda J, Pinillos D, Velasco MJ, Castro P, Ostos M . A high MUFA and NCEP diet decrease the insulin resistance in young healthy subjects. Circulation 1998; 90: 193S.
Lairon D . Dietary fibres: effects on lipid metabolism and mechanisms of action. Eur J Clin Nutr 1996; 50: 125–133.
Acknowledgements
This study was partially supported by the Spanish AGL-2008 04892-C03–02 project. We thank the Gynecology and Obstetrics Department and Laboratory Services of Mérida Hospital (Extremadura, Spain), participant mothers and children, and Carmen Bravo from Departamento de Apoyo a la Investigación de la Universidad Complutense of Madrid.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on European Journal of Clinical Nutrition website
Supplementary information
Rights and permissions
About this article
Cite this article
Gesteiro, E., Rodríguez Bernal, B., Bastida, S. et al. Maternal diets with low healthy eating index or mediterranean diet adherence scores are associated with high cord-blood insulin levels and insulin resistance markers at birth. Eur J Clin Nutr 66, 1008–1015 (2012). https://doi.org/10.1038/ejcn.2012.92
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2012.92
Keywords
This article is cited by
-
The possible relationship between the healthy eating index-2015 and the 10-year risk of cardiovascular diseases
BMC Nutrition (2023)
-
Adherence to Mediterranean diet impacts gastrointestinal microbial diversity throughout pregnancy
BMC Pregnancy and Childbirth (2021)
-
Maternal diet quality during pregnancy is associated with biomarkers of metabolic risk among male offspring
Diabetologia (2021)
-
Walking in pregnancy and prevention of insomnia in third trimester using pedometers: study protocol of Walking_Preg project (WPP). A randomized controlled trial
BMC Pregnancy and Childbirth (2020)
-
The triglyceride-glucose index, an insulin resistance marker in newborns?
European Journal of Pediatrics (2018)