Abstract
Background/objectives:
To investigate the association between dietary patterns and prevalence and incidence 3 years later of depressive symptoms using data from the mid-aged cohort in the Australian Longitudinal Study on Women’s Health.
Subjects/methods:
Participants (aged 50–55 years) completed a food frequency questionnaire in 2001. Depressive symptoms were measured in 2001 and 2004 using the validated 10-item Centre for Epidemiologic Studies Depression scale. Multiple logistic regression was used for cross-sectional analysis (8369 women) and longitudinal analysis (7588) to assess the associations between dietary patterns and prevalence of depressive symptoms, and then for longitudinal analysis (6060) on their associations with the incidence of depressive symptoms in 2004, while adjusting for sociodemographic and lifestyle factors.
Results:
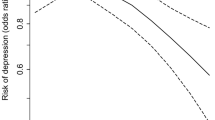
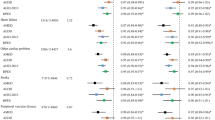
Six dietary patterns were identified from factor analysis: cooked vegetables, fruit, Mediterranean style, meat and processed meat, dairy, and high fat and sugar. A higher consumption of the Mediterranean-style diet had a cross-sectional association with lower prevalence of depressive symptoms in 2001, adjusted odds ratio 0.82 (95% confidence interval 0.77–0.88); and longitudinally with lower incidence of depressive symptoms in 2004, adjusted odds ratio 0.83 (0.75–0.91). None of the associations found for other dietary patterns remained statistically significant after adjustment for confounders. A dose–response relationship was found cross-sectionally when women were grouped according to quintiles of Mediterranean-style diet (P-value for trend <0.001).
Conclusions:
Consumption of a ‘Mediterranean-style’ dietary pattern by mid-aged women may have a protective influence against the onset of depressive symptoms. These findings suggest that dietary patterns have a potential role in the prevention and management of depressive symptoms.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
World Health Organization. Mental Health - Disorders management 2011 (cited 2011 29 August); Available from: http://www.who.int/mental_health/management/depression/definition/en/.
Lepine JP, Briley M . The increasing burden of depression. Neuropsychiatr Dis Treat 2011; 7 (Suppl 1), 3–7.
Sarris J, Schoendorfer N, Kavanagh DJ . Major depressive disorder and nutritional medicine: a review of monotherapies and adjuvant treatments. Nutr Rev 2009; 67: 125–131.
Murakami K, Sasaki S . Dietary intake and depressive symptoms: a systematic review of observational studies. Mol Nutr Food Res 2010; 54: 471–488.
Nanri A, Kimura Y, Matsushita Y, Ohta M, Sato M, Mishima N et al. Dietary patterns and depressive symptoms among Japanese men and women. Eur J Clin Nutr 2010; 64: 832–839.
Oddy WH, Robinson M, Ambrosini GL, O'Sullivan TA, de Klerk NH, Beilin LJ et al. The association between dietary patterns and mental health in early adolescence. Prev Med 2009; 49: 39–44.
Samieri C, Jutand M-A, Féart C, Capuron L, Letenneur L, Barberger-Gateau P . Dietary patterns derived by hybrid clustering method in older people: association with cognition, mood, and self-rated health. J Am Diet Assoc 2008; 108: 1461–1471.
Jacka FN, Pasco JA, Mykletun A, Williams LJ, Hodge AM, O’Reilly SL et al. Association of western and traditional diets with depression and anxiety in women. Am J Psychiat 2010; 167: 305–311.
Akbaraly TN, Brunner EJ, Ferrie JE, Marmot MG, Kivimaki M, Singh-Manoux A . Dietary pattern and depressive symptoms in middle age. Br J Psychiatry 2009; 195: 408–413.
Sanchez-Villegas A, Delgado-Rodriguez M, Alonso A, Schlatter J, Lahortiga F, Majem LS et al. Association of the mediterranean dietary pattern with the incidence of depression: the Seguimiento Universidad de Navarra/University of Navarra Follow-up (SUN) cohort. Arch Gen Psychiatry 2009; 66: 1090–1098.
World Health Organization. The World Health Report 2003. Shaping the future: Geneva, 2003.
Okubo H, Miyake Y, Sasaki S, Tanaka K, Murakami K, Hirota Y et al. Dietary patterns during pregnancy and the risk of postpartum depression in Japan: the Osaka Maternal and Child Health Study. Br J Nutr 2011; 105: 1251–1257.
Chatzi L, Melaki V, Sarri K, Apostolaki I, Roumeliotaki T, Georgiou V et al. Dietary patterns during pregnancy and the risk of postpartum depression: the mother-child ‘Rhea’ cohort in Crete, Greece. Public Health Nutr 2011; 14: 1663–1670.
Lucas M, Mirzaei F, O’Reilly EJ, Pan A, Willett WC, Kawachi I et al. Dietary intake of n−3 and n−6 fatty acids and the risk of clinical depression in women: a 10-y prospective follow-up study. Am J Clin Nutr 2011; 93: 1337–1343.
Brown WJ, Bryson L, Byles JE, Dobson AJ, Lee C, Mishra G et al. Women’s health Australia: Recruitment for a national longitudinal cohort study. Women Health 1998; 28: 23–40.
Lee C, Dobson AJ, Brown WJ, Bryson L, Byles J, Warner-Smith P et al. Cohort profile: the Australian Longitudinal Study on Women’s Health. Int J Epidemiol 2005; 34: 987–991.
Andresen EM, Malmgren JA, Carter WB, Patrick DL . Screening for depression in well older adults - evaluation of a short-form of the Ces-D. Am J Prev Med 1994; 10: 77–84.
Boey KW . Cross-validation of a short form of the CES-D in Chinese elderly. Int J Geriatr Psychiatry 1999; 14: 608–617.
Cheng ST, Chan AC . The center for epidemiologic studies depression scale in older Chinese: thresholds for long and short forms. Int J Geriatr Psychiatry 2005; 20: 465–470.
Hodge A, Patterson AJ, Brown WJ, Ireland P, Giles G . The Anti Cancer Council of Victoria FFQ: relative validity of nutrient intakes compared with weighed food records in young to middle-aged women in a study of iron supplementation. Aust N Z J Public Health 2000; 24: 576–583.
Ireland P, Jolley D, Giles G, O’Dea K, Powles J, Rutishauser I et al. Development of the Melbourne FFQ: a food frequency questionnaire for use in an Australian prospective study involving and ethnically diverse cohort. Asia Pac J Clin Nutr 1994; 3: 19–31.
Australian Government Publishing Service. NUTTAB95: Nutrient Data Table for Use in Australia. Australian Government Publishing Service: Canberra, 1995.
Australian Bureau of Statistics. Australian Standard Classification of Occupations. The Australian Bureau of Statistics: Canberra, 1997.
Brown WJ, Burton NW, Marshall AL, Miller YD . Reliability and validity of a modified self-administered version of the active Australia physical activity survey in a sample of mid-age women. Aust N Z J Public Health 2008; 32: 535–541.
Bell S, Lee C . Development of the perceived stress questionnaire for young women. Psychol Health Med 2002; 7: 189–201.
Kline P An Easy Guide to Factor Analysis. Routledge: London, UK, 1994.
Kesse-Guyot E, Touvier M, Andreeva VA, Jeandel C, Ferry M, Hercberg S et al. Cross-sectional but not longitudinal association between n-3 fatty acid intake and depressive symptoms: results from the SU.VI.MAX 2 study. Am J Epidemiol 2012; 175: 979–987.
Sánchez-Villegas A, Verberne L, De Irala J, Ruíz-Canela M, Toledo E, Serra-Majem L et al. Dietary fat intake and the risk of depression: the SUN project. PLoS ONE 2011; 6: e16268.
Sánchez-Villegas A, Toledo E, de Irala J, Ruiz-Canela M, Pla-Vidal J, Martínez-González MA . Fast-food and commercial baked goods consumption and the risk of depression. Public Health Nutr 2012; 15: 424–432.
Crawford GB, Khedkar A, Flaws JA, Sorkin JD, Gallicchio L . Depressive symptoms and self-reported fast-food intake in midlife women. Prev Med 2011; 52: 254–257.
Begg S, Vos T, Barker B, Stevenson C, Stanley L, Lopez A . The Burden of Disease and Injury in Australia 2003. Australian Institute of Health and Welfare: Canberra, 2007.
Newby PK, Tucker KL . Empirically derived eating patterns using factor or cluster analysis: a review. Nutr Rev 2004; 62: 177–203.
Gomez-Pinilla F . Brain foods: the effects of nutrients on brain function. Nat Rev Neurosci 2008; 9: 568–578.
Parker G, Gibson NA, Brotchie H, Heruc G, Rees AM, Hadzi-Pavlovic D . Omega-3 fatty acids and mood disorders. Am J Psychiatry 2006; 163: 969–978.
Belmaker RH, Agam G . Major depressive disorder. N Engl J Med 2008; 358: 55–68.
Sinclair AJ, Tassoni D, Kaur G, Weisinger RS . The role of eicosanoids in the brain. Asia Pac J Clin Nutr 2008; 17: 220–228.
Toker L, Amar S, Bersudsky Y, Benjamin J, Klein E . The biology of tryptophan depletion and mood disorders. Isr J Psychiatry Relat Sci 2010; 47: 46–55.
Smith RS . The macrophage theory of depression. Med Hypotheses 1991; 35: 298–306.
Bottiglieri T . Homocysteine and folate metabolism in depression. Prog Neuropsychopharmacol Biol Psychiatry 2005; 29: 1103–1112.
Acknowledgements
We thank Professor Graham Giles of the Cancer Epidemiology Centre of The Cancer Council Victoria for permission to use the Dietary Questionnaire for Epidemiological Studies (Version 2), Melbourne: the Cancer Council Victoria, 1996. We also thank all the participants for their valuable contribution to this project. The Australian Government Department of Health and Ageing provided funding for the Australian Longitudinal Study on Women’s Health. GDM is supported by the Australian National Health and Medical Research Council.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Contributors: JR was responsible for statistical analysis, interpretation and presentation of data, and drafted the manuscript. AJD and GDM contributed to the study design, statistical analysis, interpretation of the data, and contributed a critical revision of the manuscript. All authors approved the final version.
Rights and permissions
About this article
Cite this article
Rienks, J., Dobson, A. & Mishra, G. Mediterranean dietary pattern and prevalence and incidence of depressive symptoms in mid-aged women: results from a large community-based prospective study. Eur J Clin Nutr 67, 75–82 (2013). https://doi.org/10.1038/ejcn.2012.193
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2012.193
Keywords
This article is cited by
-
The association between dietary inflammatory index, dietary antioxidant index, and mental health in adolescent girls: an analytical study
BMC Public Health (2022)
-
The relation between MIND diet with psychological disorders and psychological stress among Iranian adults
BMC Psychiatry (2022)
-
Dietary patterns, breakfast consumption, meals with family and associations with common mental disorders in adolescents: a school-based cross-sectional study
BMC Public Health (2022)
-
Adherence to the MIND dietary pattern and sleep quality, sleep related outcomes and mental health in male adults: a cross-sectional study
BMC Psychiatry (2022)
-
Mediterranean diet and depression: a population-based cohort study
International Journal of Behavioral Nutrition and Physical Activity (2021)