Abstract
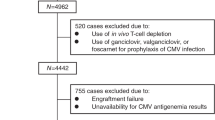
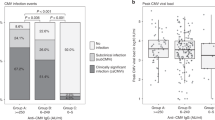
Several studies have reported an association between CMV reactivation and a decreased incidence of relapse for AML after adult donor allogeneic hematopoietic cell transplantation (HCT). Limited data, however, are available on the impact of CMV reactivation on relapse after cord blood (CB) stem cell transplantation. The unique combination of higher incidence of CMV reactivation in the seropositive recipient and lower incidence of graft versus host disease (GvHD) in CB HCT permits a valuable design to analyze the impact of CMV reactivation. Data from 1684 patients transplanted with CB between 2003 and 2010 for AML and ALL were analyzed. The median time to CMV reactivation was 34 days (range: 2–287). CMV reactivation and positive CMV serology were associated with increased non-relapse mortality (NRM) among both AML and ALL CB recipients (reactivation, AML: relative risk (RR) 1.41 (1.07–1.85); ALL: 1.60 (1.14–2.23); Serology, AML: RR 1.39 (1.05–1.85), ALL: RR 1.61 (1.18–2.19)). For patients with ALL, but not those with AML, this yielded inferior overall survival (P<0.005). Risk of relapse was not influenced by CMV reactivation or positive CMV serostatus for either disease.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Winston DJ, Gale RP . Prevention and treatment of cytomegalovirus infection and disease after bone marrow transplantation in the 1990s. Bone Marrow Transplant 1991; 8: 7–11.
Ljungman P, Hakki M, Boeckh M . Cytomegalovirus in hematopoietic stem cell transplant recipients. Hematol Oncol Clin North Am 2011; 25: 151–169.
Behrendt CE, Rosenthal J, Bolotin E, Nakamura R, Zaia J, Forman SJ . Donor and recipient CMV serostatus and outcome of pediatric allogeneic HSCT for acute leukemia in the era of CMV-preemptive therapy. Biol Blood Marrow Transplant 2009; 15: 54–60.
Elmaagacli AH, Steckel NK, Koldehoff M, Hegerfeldt Y, Trenschel R, Ditschkowski M et al. Early human cytomegalovirus replication after transplantation is associated with a decreased relapse risk: evidence for a putative virus-versus-leukemia effect in acute myeloid leukemia patients. Blood 2011; 118: 1402–1412.
Green ML, Leisenring WM, Xie H, Walter RB, Mielcarek M, Sandmaier BM et al. CMV reactivation after allogeneic HCT and relapse risk: evidence for early protection in acute myeloid leukemia. Blood 2013; 122: 1316–1324.
Ito S, Pophali P, Co W, Koklanaris EK, Superata J, Fahle GA et al. CMV reactivation is associated with a lower incidence of relapse after allo-SCT for CML. Bone Marrow Transplant 2013; 48: 1313–1316.
Jang JE, Kim SJ, Cheong JW, Hyun SY, Kim YD, Kim YR et al. Early CMV replication and subsequent chronic GVHD have a significant anti-leukemic effect after allogeneic HSCT in acute myeloid leukemia. Ann Hematol 2014; 94: 275–282.
Manjappa S, Bhamidipati PK, Stokerl-Goldstein KE, DiPersio JF, Uy GL, Westervelt P et al. Protective effect of cytomegalovirus reactivation on relapse after allogeneic hematopoietic cell transplantation in acute myeloid leukemia patients is influenced by conditioning regimen. Biol Blood Marrow Transplant 2014; 20: 46–52.
Foley B, Cooley S, Verneris MR, Pitt M, Curtsinger J, Luo X et al. Cytomegalovirus reactivation after allogeneic transplantation promotes a lasting increase in educated NKG2C+ natural killer cells with potent function. Blood 2012; 119: 2665–2674.
Scheper W, van Dorp S, Kersting S, Pietersma F, Lindemans C, Hol S et al. gammadeltaT cells elicited by CMV reactivation after allo-SCT cross-recognize CMV and leukemia. Leukemia 2013; 27: 1328–1338.
Nakamura R, Battiwalla M, Solomon S, Follmann D, Chakrabarti S, Cortez K et al. Persisting posttransplantation cytomegalovirus antigenemia correlates with poor lymphocyte proliferation to cytomegalovirus antigen and predicts for increased late relapse and treatment failure. Biol Blood Marrow Transplant 2004; 10: 49–57.
Soiffer RJ, Lerademacher J, Ho V, Kan F, Artz A, Champlin RE et al. Impact of immune modulation with anti-T-cell antibodies on the outcome of reduced-intensity allogeneic hematopoietic stem cell transplantation for hematologic malignancies. Blood 2011; 117: 6963–6970.
Admiraal R, van Kesteren C, Jol-van der Zijde CM, Lankester AC, Bierings MB, Egberts TCG et al. Association between anti-thymocyte globulin exposure and CD4+ immune reconstitution in paediatric haemopoietic cell transplantation: a multicentre, retrospective pharmacodynamic cohort analysis. Lancet Haematol 2015; 2: e194–e203.
Thomson KJ, Mackinnon S, Peggs KS . CMV-specific cellular therapy for acute myeloid leukemia? Blood 2012; 119: 1088–1090 author reply 1090-1081.
Sellar RS, Arce Vargas F, Henry JY, Verfuerth S, Charrot S, Beaton B et al. CMV promotes recipient T-cell immunity following reduced intensity T-cell depleted HSCT significantly modulating chimerism status. Blood 2014; 125: 731–739.
Jeljeli M, Guerin-El Khourouj V, Porcher R, Fahd M, Leveille S, Yakouben K et al. Relationship between cytomegalovirus (CMV) reactivation, CMV-driven immunity, overall immune recovery and graft-versus-leukaemia effect in children. Br J Haematol 2014; 166: 229–239.
Ljungman P, Brand R, Hoek J, de la Camara R, Cordonnier C, Einsele H et al. Donor cytomegalovirus status influences the outcome of allogeneic stem cell transplant: a study by the European group for blood and marrow transplantation. Clin Infect Dis 2014; 59: 473–481.
Travi G, Pergam SA, Xie H, Boeckh MJ . Donor CMV serostatus not predictive of relapse in D-/R- pediatric HCT. Biol Blood Marrow Transplant 2009; 15: 758–760.
McGoldrick SM, Bleakley ME, Guerrero A, Turtle CJ, Yamamoto TN, Pereira SE et al. Cytomegalovirus-specific T cells are primed early after cord blood transplant but fail to control virus in vivo. Blood 2013; 121: 2796–2803.
Eapen M, Rubinstein P, Zhang MJ, Stevens C, Kurtzberg J, Scaradavou A et al. Outcomes of transplantation of unrelated donor umbilical cord blood and bone marrow in children with acute leukaemia: a comparison study. Lancet 2007; 369: 1947–1954.
Kumar P, Defor TE, Brunstein C, Barker JN, Wagner JE, Weisdorf DJ et al. Allogeneic hematopoietic stem cell transplantation in adult acute lymphocytic leukemia: impact of donor source on survival. Biol Blood Marrow Transplant 2008; 14: 1394–1400.
Willemze R, Rodrigues CA, Labopin M, Sanz G, Michel G, Socie G et al. KIR-ligand incompatibility in the graft-versus-host direction improves outcomes after umbilical cord blood transplantation for acute leukemia. Leukemia 2009; 23: 492–500.
Wagner JE, Eapen M, Carter S, Wang Y, Schultz KR, Wall DA et al. One-unit versus two-unit cord-blood transplantation for hematologic cancers. N Engl J Med 2014; 371: 1685–1694.
Armand P, Kim HT, Logan BR, Wang Z, Alyea EP, Kalaycio ME et al. Validation and refinement of the Disease Risk Index for allogeneic stem cell transplantation. Blood 2014; 123: 3664–3671.
Lonnqvist B, Ringden O, Ljungman P, Wahren B, Gahrton G . Reduced risk of recurrent leukaemia in bone marrow transplant recipients after cytomegalovirus infection. Br J Haematol 1986; 63: 671–679.
Cantoni N, Hirsch HH, Khanna N, Gerull S, Buser A, Bucher C et al. Evidence for a bidirectional relationship between cytomegalovirus replication and acute graft-versus-host disease. Biol Blood Marrow Transplant 2010; 16: 1309–1314.
Schmidt-Hieber M, Labopin M, Beelen D, Volin L, Ehninger G, Finke J et al. CMV serostatus still has an important prognostic impact in de novo acute leukemia patients after allogeneic stem cell transplantation: a report from the Acute Leukemia Working Party of EBMT. Blood 2013; 122: 3359–3364.
Nichols WG, Corey L, Gooley T, Davis C, Boeckh M . High risk of death due to bacterial and fungal infection among cytomegalovirus (CMV)-seronegative recipients of stem cell transplants from seropositive donors: evidence for indirect effects of primary CMV infection. J Infect Dis 2002; 185: 273–282.
Ariza-Heredia EJ, Nesher L, Chemaly RF . Cytomegalovirus diseases after hematopoietic stem cell transplantation: a mini-review. Cancer Lett 2014; 342: 1–8.
Marty FM, Winston DJ, Rowley SD, Vance E, Papanicolaou GA, Mullane KM et al. CMX001 to prevent cytomegalovirus disease in hematopoietic-cell transplantation. N Engl J Med 2013; 369: 1227–1236.
Blyth E, Clancy L, Simms R, Ma CK, Burgess J, Deo S et al. Donor-derived CMV-specific T cells reduce the requirement for CMV-directed pharmacotherapy after allogeneic stem cell transplantation. Blood 2013; 121: 3745–3758.
Leen AM, Bollard CM, Mendizabal AM, Shpall EJ, Szabolcs P, Antin JH et al. Multicenter study of banked third-party virus-specific T cells to treat severe viral infections after hematopoietic stem cell transplantation. Blood 2013; 121: 5113–5123.
Gea-Banacloche JC . Antiviral cell therapy: is this the future? Blood 2013; 121: 5108–5109.
Heslop HE . Pharmacotherapy versus T lymphocytes for CMV. Blood 2013; 121: 3544–3545.
Jain NA, Lu K, Ito S, Muranski P, Hourigan CS, Haggerty J et al. The clinical and financial burden of pre-emptive management of cytomegalovirus disease after allogeneic stem cell transplantation-implications for preventative treatment approaches. Cytotherapy 2014; 16: 927–933.
Acknowledgements
The CIBMTR is supported by Public Health Service Grant/Cooperative Agreement 5U24-CA076518 from the National Cancer Institute (NCI), the National Heart, Lung and Blood Institute (NHLBI) and the National Institute of Allergy and Infectious Diseases (NIAID); a Grant/Cooperative Agreement 5U10HL069294 from NHLBI and NCI; a contract HHSH250201200016C with Health Resources and Services Administration (HRSA/DHHS); two Grants N00014-13-1-0039 and N00014-14-1-0028 from the Office of Naval Research; and grants from Alexion; *Amgen Inc.; Anonymous donation to the Medical College of Wisconsin; Be the Match Foundation; *Bristol Myers Squibb Oncology; *Celgene Corporation; *Chimerix Inc.; Fred Hutchinson Cancer Research Center; Gamida Cell Ltd.; Genentech Inc.; Genzyme Corporation; *Gilead Sciences Inc.; Health Research Inc. Roswell Park Cancer Institute; HistoGenetics Inc.; Incyte Corporation; *Jazz Pharmaceuticals Inc.; Jeff Gordon Children’s Foundation; The Leukemia & Lymphoma Society; The Medical College of Wisconsin; Merck & Co Inc.; Mesoblast; *Millennium: The Takeda Oncology Co.; *Miltenyi Biotec Inc.; National Marrow Donor Program; Neovii Biotech NA Inc.; Novartis Pharmaceuticals Corporation; Onyx Pharmaceuticals; Optum Healthcare Solutions Inc.; Otsuka America Pharmaceutical Inc.; Otsuka Pharmaceutical Co, Ltd.—Japan; Oxford Immunotec; Perkin Elmer Inc.; Pharmacyclics; *Sanofi US; Seattle Genetics; Sigma-Tau Pharmaceuticals; *Spectrum Pharmaceuticals Inc.; St. Baldrick’s Foundation; *Sunesis Pharmaceuticals Inc.; Swedish Orphan Biovitrum Inc.; Telomere Diagnostics Inc.; TerumoBCT; Therakos Inc.; University of Minnesota; and *Wellpoint Inc. Corporate Members have been denoted by the ‘*’ symbol.
Disclaimer
The views expressed in this article do not reflect the official policy or position of the National Institute of Health, the Department of the Navy, the Department of Defense, Health Resources and Services Administration (HRSA) or any other agency of the US Government.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Ramanathan, M., Teira, P., Battiwalla, M. et al. Impact of early CMV reactivation in cord blood stem cell recipients in the current era. Bone Marrow Transplant 51, 1113–1120 (2016). https://doi.org/10.1038/bmt.2016.89
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2016.89
This article is cited by
-
CMV Infection Post Allogeneic Hematopoietic Stem Cell Transplantation in a Resource Limited Country
Indian Journal of Hematology and Blood Transfusion (2023)
-
Reduced leukemia relapse through cytomegalovirus reactivation in killer cell immunoglobulin-like receptor-ligand-mismatched cord blood transplantation
Bone Marrow Transplantation (2021)
-
Effects of HLA mismatch on cytomegalovirus reactivation in cord blood transplantation
Bone Marrow Transplantation (2019)
-
Intrabone transplant provides full stemness of cord blood stem cells with fast hematopoietic recovery and low GVHD rate: results from a prospective study
Bone Marrow Transplantation (2019)
-
Cytomegalovirus infection is associated with AML relapse after allo-HSCT: a meta-analysis of observational studies
Annals of Hematology (2019)