Abstract
Metabolic syndrome (MetS) is a constellation of cardiovascular risk factors that increases the risk of cardiovascular disease, diabetes mellitus and all cause mortality. Long-term survivors of hematopoietic cell transplantation (HCT) have a substantial risk of developing MetS and cardiovascular disease, with the estimated prevalence of MetS being 31–49% among HCT recipients. Although MetS has not yet been proven to impact cardiovascular risk after HCT, an understanding of the incidence and risk factors for MetS in HCT recipients can provide the foundation to evaluate screening guidelines and develop interventions that may mitigate cardiovascular-related mortality. A working group was established through the Center for International Blood and Marrow Transplant Research and the European Group for Blood and Marrow Transplantation with the goal of reviewing literature and recommend practices appropriate to HCT recipients. Here we deliver consensus recommendations to help clinicians provide screening and preventive care for MetS and cardiovascular disease among HCT recipients. All HCT survivors should be advised of the risks of MetS and encouraged to undergo recommended screening based on their predisposition and ongoing risk factors.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Majhail NS, Tao L, Bredeson C, Davies S, Dehn J, Gajewski JL et al. Prevalence of hematopoietic cell transplant survivors in the United States. Biol Blood Marrow Transplant 2013; 19: 1498–1501.
Bhatia S, Francisco L, Carter A, Sun CL, Baker KS, Gurney JG et al. Late mortality after allogeneic hematopoietic cell transplantation and functional status of long-term survivors: report from the Bone Marrow Transplant Survivor Study. Blood 2007; 110: 3784–3792.
Bhatia S, Robison LL, Francisco L, Carter A, Liu Y, Grant M et al. Late mortality in survivors of autologous hematopoietic-cell transplantation: report from the Bone Marrow Transplant Survivor Study. Blood 2005; 105: 4215–4222.
Majhail NS, Flowers ME, Ness KK, Jagasia M, Carpenter PA, Arora M et al. High prevalence of metabolic syndrome after allogeneic hematopoietic cell transplantation. Bone Marrow Transplant 2009; 43: 49–54.
Paris C, Yates L, Lama P, Zepeda AJ, Gutierrez D, Palma J . Evaluation of metabolic syndrome after hematopoietic stem cell transplantation in children and adolescents. Pediatr Blood Cancer 2012; 59: 306–310.
Annaloro C, Usardi P, Airaghi L, Giunta V, Forti S, Orsatti A et al. Prevalence of metabolic syndrome in long-term survivors of hematopoietic stem cell transplantation. Bone Marrow Transplant 2008; 41: 797–804.
McMillen KK, Schmidt EM, Storer BE, Bar M . Metabolic syndrome appears early after hematopoietic cell transplantation. Metab Syndr Relat Disord 2014; 12: 367–371.
Oudin C, Auquier P, Bertrand Y, Contet A, Kanold J, Sirvent N et al. Metabolic syndrome in adults who received hematopoietic stem cell transplantation for acute childhood leukemia: an LEA study. Bone Marrow Transplant 2015; 50: 1438–1444.
Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation 2005; 112: 2735–2752.
Chow EJ, Mueller BA, Baker KS, Cushing-Haugen KL, Flowers ME, Martin PJ et al. Cardiovascular hospitalizations and mortality among recipients of hematopoietic stem cell transplantation. Ann Intern Med 2011; 155: 21–32.
Oudin C, Simeoni MC, Sirvent N, Contet A, Begu-Le Coroller A, Bordigoni P et al. Prevalence and risk factors of the metabolic syndrome in adult survivors of childhood leukemia. Blood 2011; 117: 4442–4448.
Gurney JG, Ness KK, Sibley SD, O'Leary M, Dengel DR, Lee JM et al. Metabolic syndrome and growth hormone deficiency in adult survivors of childhood acute lymphoblastic leukemia. Cancer 2006; 107: 1303–1312.
Rizzo JD, Wingard JR, Tichelli A, Lee SJ, Van Lint MT, Burns LJ et al. Recommended screening and preventive practices for long-term survivors after hematopoietic cell transplantation: joint recommendations of the European Group for Blood and Marrow Transplantation, the Center for International Blood and Marrow Transplant Research, and the American Society of Blood and Marrow Transplantation. Biol Blood Marrow Transplant 2006; 12: 138–151.
Majhail NS, Rizzo JD, Lee SJ, Aljurf M, Atsuta Y, Bonfim C et al. Recommended screening and preventive practices for long-term survivors after hematopoietic cell transplantation. Biol Blood Marrow Transplant 2012; 18: 348–371.
Pulsipher MA, Skinner R, McDonald GB, Hingorani S, Armenian SH, Cooke KR et al. National Cancer Institute, National Heart, Lung and Blood Institute/Pediatric Blood and Marrow Transplantation Consortium First International Consensus Conference on late effects after pediatric hematopoietic cell transplantation: the need for pediatric-specific long-term follow-up guidelines. Biol Blood Marrow Transplant 2012; 18: 334–347.
Isomaa B, Almgren P, Tuomi T, Forsen B, Lahti K, Nissen M et al. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care 2001; 24: 683–689.
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009; 120: 1640–1645.
Shin JA, Lee JH, Lim SY, Ha HS, Kwon HS, Park YM et al. Metabolic syndrome as a predictor of type 2 diabetes, and its clinical interpretations and usefulness. J Diabetes Investig 2013; 4: 334–343.
International Diabetes Federation: the IDF consensus worldwide definition of the metabolic syndrome. Available at: http://www.idf.org/metabolic-syndrome.
Kaur J . A comprehensive review on metabolic syndrome. Cardiol Res Pract 2014; 2014: 943162.
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA 2001; 285: 2486–2497.
Alberti KG, Zimmet PZ . Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med 1998; 15: 539–553.
Mancia G, Bombelli M, Facchetti R, Casati A, Ronchi I, Quarti-Trevano F et al. Impact of different definitions of the metabolic syndrome on the prevalence of organ damage, cardiometabolic risk and cardiovascular events. J Hypertens 2010; 28: 999–1006.
Lin CC, Liu CS, Li CI, Lin WY, Lai MM, Lin T et al. The relation of metabolic syndrome according to five definitions to cardiovascular risk factors—a population-based study. BMC Public Health 2009; 9: 484.
Alberti KG, Zimmet P, Shaw J . The metabolic syndrome—a new worldwide definition. Lancet 2005; 366: 1059–1062.
Ogden CL, Carroll MD, Kit BK, Flegal KM . Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 2014; 311: 806–814.
World Health Organization Regional Office for Europe. Data and Statistics. Available at: http://www.euro.who.int/en/health-topics/noncommunicable-diseases/obesity/data-and-statistics.
Jensen MD, Ryan DH, Apovian CM, Ard JD, Comuzzie AG, Donato KA et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation 2014; 129: S102–S138.
Despres JP, Lemieux I . Abdominal obesity and metabolic syndrome. Nature 2006; 444: 881–887.
Amato MC, Guarnotta V, Giordano C . Body composition assessment for the definition of cardiometabolic risk. J Endocrinol Invest 2013; 36: 537–543.
Sorror ML, Maris MB, Storb R, Baron F, Sandmaier BM, Maloney DG et al. Hematopoietic cell transplantation (HCT)-specific comorbidity index: a new tool for risk assessment before allogeneic HCT. Blood 2005; 106: 2912–2919.
Aplenc R, Zhang M-J, Sung L, Zhu X, Ho VT, Cooke K et al. Effect of body mass in children with hematologic malignancies undergoing allogeneic bone marrow transplantation. Blood 2014; 123: 3504–3511.
Fuji S, Kim S-W, Yoshimura K-i, Akiyama H, Okamoto S-i, Sao H et al. Possible association between obesity and posttransplantation complications including infectious diseases and acute graft-versus-host disease. Biol Blood Marrow Transplant 2009; 15: 73–82.
Fuji S, Takano K, Mori T, Eto T, Taniguchi S, Ohashi K et al. Impact of pretransplant body mass index on the clinical outcome after allogeneic hematopoietic SCT. Bone Marrow Transplant 2014; 49: 1505–1512.
Baker KS, Chow E, Steinberger J . Metabolic syndrome and cardiovascular risk in survivors after hematopoietic cell transplantation. Bone Marrow Transplant 2012; 47: 619–625.
Narici MV, Maffulli N . Sarcopenia: characteristics, mechanisms and functional significance. Br Med Bull 2010; 95: 139–159.
Kyle UG, Chalandon Y, Miralbell R, Karsegard VL, Hans D, Trombetti A et al. Longitudinal follow-up of body composition in hematopoietic stem cell transplant patients. Bone Marrow Transplant 2005; 35: 1171–1177.
Li C, Liu P, Liu L, Zhang X, Yang P, Sheng H et al. Metabolic syndrome in hematologic malignancies survivors: a meta-analysis. Med Oncol 2015; 32: 422.
Greenfield DM, Boland E, Ezaydi Y, Ross RJ, Ahmedzai SH, Snowden JA . Endocrine, metabolic, nutritional and body composition abnormalities are common in advanced intensively-treated (transplanted) multiple myeloma. Bone Marrow Transplant 2014; 49: 907–912.
Mostoufi-Moab S, Ginsberg JP, Bunin N, Zemel BS, Shults J, Thayu M et al. Body composition abnormalities in long-term survivors of pediatric hematopoietic stem cell transplantation. J Pediatr 2012; 160: 122–128.
National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002; 106: 3143–3421.
Thompson WG, Gau GT . Hypertriglyceridemia and its pharmacologic treatment among US adults—invited commentary. Arch Intern Med 2009; 169: 578–579.
Fodor G . Primary prevention of CVD: treating dyslipidaemia. BMJ Clin Evid 2008; 2008. pii: 0215.
Scheidt-Nave C, Du Y, Knopf H, Schienkiewitz A, Ziese T, Nowossadeck E et al. Prevalence of dyslipidemia among adults in Germany: results of the German Health Interview and Examination Survey for Adults (DEGS 1). Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2013; 56: 661–667.
Gonzalez-Juanatey JR, Millan J, Alegria E, Guijarro C, Lozano JV, Vitale GC . Prevalence and characteristics of lipid abnormalities in patients treated with statins in primary and secondary prevention in Spain. DYSIS-Spain Study. Rev Esp Cardiol 2011; 64: 286–294.
Tichelli A, Bucher C, Rovo A, Stussi G, Stern M, Paulussen M et al. Premature cardiovascular disease after allogeneic hematopoietic stem-cell transplantation. Blood 2007; 110: 3463–3471.
Kagoya Y, Seo S, Nannya Y, Kurokawa M . Hyperlipidemia after allogeneic stem cell transplantation: prevalence, risk factors, and impact on prognosis. Clin Transplant 2012; 26: E168–E175.
Blaser BW, Kim HT, Alyea EP 3rd, Ho VT, Cutler C, Armand P et al. Hyperlipidemia and statin use after allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transplant 2012; 18: 575–583.
Chow EJ, Baker KS, Lee SJ, Flowers ME, Cushing-Haugen KL, Inamoto Y et al. Influence of conventional cardiovascular risk factors and lifestyle characteristics on cardiovascular disease after hematopoietic cell transplantation. J Clin Oncol 2014; 32: 191–198.
Griffith ML, Savani BN, Boord JB . Dyslipidemia after allogeneic hematopoietic stem cell transplantation: evaluation and management. Blood 2010; 116: 1197–1204.
Marini BL, Choi SW, Byersdorfer CA, Cronin S, Frame DG . Treatment of dyslipidemia in allogeneic hematopoietic stem cell transplant patients. Biol Blood Marrow Transplant 2015; 21: 809–820.
Chow EJ, Wong K, Lee SJ, Cushing-Haugen KL, Flowers ME, Friedman DL et al. Late cardiovascular complications after hematopoietic cell transplantation. Biol Blood Marrow Transplant 2014; 20: 794–800.
Felicetti F, D'Ascenzo F, Moretti C, Corrias A, Omede P, Marra WG et al. Prevalence of cardiovascular risk factors in long-term survivors of childhood cancer: 16 years follow up from a prospective registry. Eur J Prev Cardiol 2015; 22: 762–770.
McCrindle BW, Urbina EM, Dennison BA, Jacobson MS, Steinberger J, Rocchini AP et al. Drug therapy of high-risk lipid abnormalities in children and adolescents: a scientific statement from the American Heart Association Atherosclerosis, Hypertension, and Obesity in Youth Committee, Council of Cardiovascular Disease in the Young, with the Council on Cardiovascular Nursing. Circulation 2007; 115: 1948–1967.
Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J . Global burden of hypertension: analysis of worldwide data. Lancet 2005; 365: 217–223.
James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014; 311: 507–520.
Baker KS, Ness KK, Steinberger J, Carter A, Francisco L, Burns LJ et al. Diabetes, hypertension, and cardiovascular events in survivors of hematopoietic cell transplantation: a report from the bone marrow transplantation survivor study. Blood 2007; 109: 1765–1772.
Pophali PA, Klotz JK, Ito S, Jain NA, Koklanaris E, Le RQ et al. Male survivors of allogeneic hematopoietic stem cell transplantation have a long term persisting risk of cardiovascular events. Exp Hematol 2014; 42: 83–89.
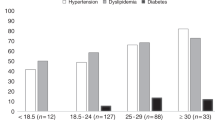
Majhail NS, Challa TR, Mulrooney DA, Baker KS, Burns LJ . Hypertension and diabetes mellitus in adult and pediatric survivors of allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transplant 2009; 15: 1100–1107.
American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care 2010; 33: S62–S69.
The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 1993; 329: 977–986.
UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 1998; 352: 837–853.
Schellenberg ES, Dryden DM, Vandermeer B, Ha C, Korownyk C . Lifestyle interventions for patients with and at risk for type 2 diabetes: a systematic review and meta-analysis. Ann Intern Med 2013; 159: 543–551.
Perreault L, Pan Q, Mather KJ, Watson KE, Hamman RF, Kahn SE et al. Effect of regression from prediabetes to normal glucose regulation on long-term reduction in diabetes risk: results from the Diabetes Prevention Program Outcomes Study. Lancet 2012; 379: 2243–2251.
Selph S, Dana T, Blazina I, Bougatsos C, Patel H, Chou R . Screening for type 2 diabetes mellitus: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med 2015; 162: 765–776.
Simmons RK, Echouffo-Tcheugui JB, Sharp SJ, Sargeant LA, Williams KM, Prevost AT et al. Screening for type 2 diabetes and population mortality over 10 years (ADDITION-Cambridge): a cluster-randomised controlled trial. Lancet 2012; 380: 1741–1748.
Griffith ML, Jagasia M, Jagasia SM . Diabetes mellitus after hematopoietic stem cell transplantation. Endocr Pract 2010; 16: 699–706.
Taskinen M, Saarinen-Pihkala UM, Hovi L, Lipsanen-Nyman M . Impaired glucose tolerance and dyslipidaemia as late effects after bone-marrow transplantation in childhood. Lancet 2000; 356: 993–997.
Bizzarri C, Pinto RM, Ciccone S, Brescia LP, Locatelli F, Cappa M . Early and progressive insulin resistance in young, non-obese cancer survivors treated with hematopoietic stem cell transplantation. Pediatr Blood Cancer 2015; 62: 1650–1655.
Wei C, Thyagiarajan MS, Hunt LP, Shield JP, Stevens MC, Crowne EC . Reduced insulin sensitivity in childhood survivors of haematopoietic stem cell transplantation is associated with lipodystropic and sarcopenic phenotypes. Pediatr Blood Cancer 2015; 62: 1992–1999.
Mostoufi-Moab S, Magland J, Isaacoff EJ, Sun W, Rajapakse CS, Zemel B et al. Adverse fat depots and marrow adiposity are associated with skeletal deficits and insulin resistance in long-term survivors of pediatric hematopoietic stem cell transplantation. J Bone Miner Res 2015; 30: 1657–1666.
Hirabayashi K, Nakazawa Y, Matsuura H, Hara Y, Kurata T, Hirabayashi K et al. Risk factors for diabetes mellitus and impaired glucose tolerance following allogeneic hematopoietic stem cell transplantation in pediatric patients with hematological malignancies. Int J Hematol 2014; 99: 477–486.
Chemaitilly W, Boulad F, Oeffinger KC, Sklar CA . Disorders of glucose homeostasis in young adults treated with total body irradiation during childhood: a pilot study. Bone Marrow Transplant 2009; 44: 339–343.
Hansson GK . Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med 2005; 352: 1685–1695.
Stoll G, Bendszus M . Inflammation and atherosclerosis: novel insights into plaque formation and destabilization. Stroke 2006; 37: 1923–1932.
Lloyd-Jones DM, Leip EP, Larson MG, D'Agostino RB, Beiser A, Wilson PW et al. Prediction of lifetime risk for cardiovascular disease by risk factor burden at 50 years of age. Circulation 2006; 113: 791–798.
Tichelli A, Passweg J, Wojcik D, Rovo A, Harousseau JL, Masszi T et al. Late cardiovascular events after allogeneic hematopoietic stem cell transplantation: a retrospective multicenter study of the Late Effects Working Party of the European Group for Blood and Marrow Transplantation. Haematologica 2008; 93: 1203–1210.
Armenian SH, Sun CL, Vase T, Ness KK, Blum E, Francisco L et al. Cardiovascular risk factors in hematopoietic cell transplantation survivors: role in development of subsequent cardiovascular disease. Blood 2012; 120: 4505–4512.
Chow EJ, Simmons JH, Roth CL, Baker KS, Hoffmeister PA, Sanders JE et al. Increased cardiometabolic traits in pediatric survivors of acute lymphoblastic leukemia treated with total body irradiation. Biol Blood Marrow Transplant 2010; 16: 1674–1681.
Lorini R, Cortona L, Scaramuzza A, De Stefano P, Locatelli F, Bonetti F et al. Hyperinsulinemia in children and adolescents after bone marrow transplantation. Bone Marrow Transplant 1995; 15: 873–877.
Rovó A, Daikeler T, Halter J, Heim D, Tsakiris DA, Stern M et al. Late altered organ function in very long-term survivors after allogeneic hematopoietic stem cell transplantation: a paired comparison with their HLA-identical sibling donor. Haematologica 2010; 96: 150–155.
Heidenreich PA, Trogdon JG, Khavjou OA, Butler J, Dracup K, Ezekowitz MD et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation 2011; 123: 933–944.
Heron M . Deaths: leading causes for 2007. Natl Vital Stat Rep 2011; 59: 1–95.
Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012; 380: 2095–2128.
Krishnamurthi RV, Feigin VL, Forouzanfar MH, Mensah GA, Connor M, Bennett DA et al. Global and regional burden of first-ever ischaemic and haemorrhagic stroke during 1990–2010: findings from the Global Burden of Disease Study 2010. Lancet Glob Health 2013; 1: e259–e281.
Lloyd-Jones D, Adams R, Carnethon M, De Simone G, Ferguson TB, Flegal K et al. Heart disease and stroke statistics—2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 2009; 119: 480–486.
Roach ES, Golomb MR, Adams R, Biller J, Daniels S, Deveber G et al. Management of stroke in infants and children: a scientific statement from a Special Writing Group of the American Heart Association Stroke Council and the Council on Cardiovascular Disease in the Young. Stroke 2008; 39: 2644–2691.
Riela AR, Roach ES . Etiology of stroke in children. J Child Neurol 1993; 8: 201–220.
Sun CL, Francisco L, Kawashima T, Leisenring W, Robison LL, Baker KS et al. Prevalence and predictors of chronic health conditions after hematopoietic cell transplantation: a report from the Bone Marrow Transplant Survivor Study. Blood 2010; 116: 3129–3139.
Bodas P, Rotz S . Cerebral vascular abnormalities in pediatric patients with sickle cell disease after hematopoietic cell transplant. J Pediatr Hematol Oncol 2014; 36: 190–193.
Walters MC, Hardy K, Edwards S, Adamkiewicz T, Barkovich J, Bernaudin F et al. Pulmonary, gonadal, and central nervous system status after bone marrow transplantation for sickle cell disease. Biol Blood Marrow Transplant 2010; 16: 263–272.
Bhatt VR, Balasetti V, Jasem JA, Giri S, Armitage JO, Loberiza FR Jr. et al. Central nervous system complications and outcomes after allogeneic hematopoietic stem cell transplantation. Clin Lymphoma Myeloma Leuk 2015; 15: 606–611.
Imataki O, Uemura M, Shintani T, Matsumoto K . Reversible cerebral vasoconstriction syndrome resulted in cerebral infarction after allogeneic stem cell transplantation: a case report. Ann Hematol 2014; 93: 895–896.
Rojas JC, Banerjee C, Siddiqui F, Nourbakhsh B, Powell CM . Pearls and oysters: acute ischemic stroke caused by atypical thrombotic thrombocytopenic purpura. Neurology 2013; 80: e235–e238.
Haghikia A, Heeren M, Bockmeyer C, Haubitz B, Gwinner W . Progressive multifocal cerebral infarction in a young kidney transplant recipient due to thrombotic microangiopathy. BMC Nephrol 2014; 15: 59.
Meschia JF, Bushnell C, Boden-Albala B, Braun LT, Bravata DM, Chaturvedi S et al. Guidelines for the primary prevention of stroke: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2014; 45: 3754–3832.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
DeFilipp, Z., Duarte, R., Snowden, J. et al. Metabolic syndrome and cardiovascular disease following hematopoietic cell transplantation: screening and preventive practice recommendations from CIBMTR and EBMT. Bone Marrow Transplant 52, 173–182 (2017). https://doi.org/10.1038/bmt.2016.203
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2016.203
This article is cited by
-
International recommendations for screening and preventative practices for long-term survivors of transplantation and cellular therapy: a 2023 update
Bone Marrow Transplantation (2024)
-
Management of dyslipidemia after allogeneic hematopoietic stem cell transplantation
Lipids in Health and Disease (2022)
-
Cardio-oncology in Austria: cardiotoxicity and surveillance of anti-cancer therapies
Wiener klinische Wochenschrift (2022)
-
Comparison of blood pressure values and expression of genes associated with hypertension in children before and after hematopoietic cell transplantation
Scientific Reports (2021)
-
Clinical, social, and psycho-oncological needs of adolescents and young adults (AYA) versus older patients following hematopoietic stem cell transplantation
Journal of Cancer Research and Clinical Oncology (2021)